2214 North Central Avenue Phoenix Arizona 85004 p



- Slides: 12
2214 North Central Avenue, Phoenix, Arizona 85004 p 602. 258. 4822, f 602. 258. 4825 www. itcaonline. com
Arizona Tribal Health Policy Forum Thursday, January 12, 2017 Phoenix, Arizona
Implications of the CMS Medicaid Managed Care Final Rule and 100% FMAP Available to Non-IHS/Tribal Facilities https: //www. cms. gov/Outreach-and. Education/American-Indian-Alaska-Native/AIAN/All. Tribes-Calls. html
Headline • February 26, 2016 - CMS State Health Official (SHO) letter (SHO#16 -002) Federal Funding for Services “Received Through” an IHS/Tribal Facility and Furnished to Medicaid-Eligible American Indians and Alaska Natives • IHS/Tribal facilities may enter into care coordination agreements with non. IHS/Tribal providers, including UIO’s, to furnish services for AI/AN Medicaid beneficiaries. The amounts paid by the state for services per the agreements would be eligible for the enhanced federal matching authorized by 1905(b) of the Social Security Act at a rate of 100 percent. • Previously the service had to be a “facility service” that a Medicaid facility can provide under Medicaid law and regulation. • In the new interpretation, any service can be considered to be “received through” an IHS/Tribal facility for 100 percent FMAP, if they are IHS/Tribally authorized services covered by the Medicaid State Plan, including Long Term Services and Emergency and Non-Emergency Medical Transportation.
Headline • October 5, 2016 - CMS All Tribes Call (Webinar) - Medicaid and Children’s Health Insurance Program (CHIP) Managed Care Final Rule (Effective Date 7/25/16). Includes “Standards for Contracts Involving Indians, Indian Health Care Providers and Indian Managed Care Entities” to be phased in on or after 7/1/17. • When an IHCP is enrolled in Medicaid/CHIP as a FQHC, but is not in a MCO network, the IHCP must be paid the FQHC payment rate under the State plan, including any supplemental payment due from the state. • When an IHCP is not enrolled in Medicaid/CHIP as a FQHC, and regardless of whether the IHCP participates in the network, the IHCP must receive the applicable IHS encounter rate published annually in the Federal Register. • If the amount an IHCP receives from a MCO is less than the encounter or fee-for-service rate, the state must make a supplemental payment to the IHCP to make up the difference.
Headline • MCO’s, must permit an out-of-network IHCP to refer an Indian to a network provider for covered services. • To require Medicaid/CHIP beneficiaries to enroll in managed care to receive coverage, a state must obtain approval from CMS through a Medicaid state plan amendment, a 1915(b) waiver, or through the section 1115 demonstration authority. • States have authority to exclude Indians from mandatory managed care enrollment. Historically, CMS has not approved section 1115(a) demonstrations that have mandated Indians into managed care.
Headline • November 9, 2016 - CMS All-Tribes-Call (Webinar) - Indian Health Care Addendum for Contracting with Medicaid and CHIP Managed Care Entities • ITU Addendum outlines all the federal laws, regulations, and protections that are binding on MCOs and identifies several specific provisions that have been established in federal law that apply when contracting with an IHCP. • Use of this ITU Addendum benefits both managed care entities and IHCPs by lowering perceived barriers to contracting with IHCPs, and minimizing potential disputes.
Headline • December 5, 2016 – AHCCCS Healthcare Services for Native Americans Report. The 2016 Arizona State budget required AHCCCS to report the following information: • Estimates of State and Federal expenditures for Native Americans (Fee-for-service vs. capitated costs) • Assessment of the state fiscal implications of federal guidance regarding claiming 100% federal funds per the 2/26/16 SHO Letter: a) Services furnished by non-IHS/638’s through care coordination agreements b) Services by IHS/638 agents, employees or contracted providers that previously did not qualify for 100% federal funds • Strategies to encourage written care coordination agreements • Analysis of the SHO#16 -002 Letter on Native Americans in AZ.

Care Coordination Agreements - Steps Noted by AHCCCS: • Both IHS/Tribal and the non-IHS/Tribal provider must be registered Medicaid providers. • The Service must be requested by an IHS/Tribal practitioner. • Patients must have established relationships with IHS/Tribal providers. • Care must be provided pursuant to a written care coordination agreement. • The AHCCCS American Indian Medical Home (AIMH) proposal includes criteria for care coordination, case management and data exchange. IHS/Tribal facilities that participate would be paid on a per member per month basis for patients that are served by the AIMH. • Despite the administrative burdens. . . “AHCCCS is hopeful that this will provide a roadmap for the development of the written care coordination agreements necessary to obtain the 100% federal match for non-IHS/Tribal facility services. ”
Headline • March 24, 2011 – Past CMS Region IX guidance to AHCCCS had clarified the 100% Federal match for services provided by an agent, employee or contracted provider of the IHS/638 facility as long as the IHS/638 bills for the services directly. • The service may be provided in or outside of the facility. Inpatient and outpatient hospital services may be paid at the All-Inclusive Rate (AIR), while other services may be paid the AHCCCS Capped Fee Schedule or other approved rate. • If an IHS/638 facility is unable to provide necessary treatment, Medicaid eligible AI/ANs who enroll in AIHP may use non-IHS/638 providers for the service. These services are matched at the regular FMAP (69. 24% for categorical populations and 89. 5%-100% for restored/expansion populations. The Medicaid State Plan lists the payment rates that apply to non-IHS/638 providers.

12/14/16 - CMS Informational Bulletin Summary of Indian Provisions in Final Managed Care Regulations • December 15, 2016 - CMS Tribal Consultation on the Reimbursement Rate for Services Provided Outside of an IHS/Tribal Facility (Managed Care Regulations) • Under care coordination agreements, a Tribal facility that bills for services provided outside of the facility, the services provided by non. IHS/Tribal providers will have to be identified as “IHS/Tribal facility services. ” Services that can be claimed as such are reimbursed at the facility rate authorized in the Medicaid state plan. • To remedy the four walls limitation, CMS has determined that a Tribal facility enrolled as a provider of clinic services that bills for the services at the rate applicable to the non-Tribal provider and the service, should be re-designated as an FQHC. State Medicaid agencies will be given a grace period to consult with Tribes on a state plan amendment to designate payment for Tribal FQHC services at the IHS AIR as an Alternate Payment Model (APM).

Thank you for your time, attention and questions! Alida Montiel, Health Systems Director, Inter Tribal Council of Arizona (Alida. Montiel@itcaonline. com)
 Cientista phoenix arizona sangue
Cientista phoenix arizona sangue Condolyx
Condolyx Lesson 1 the industrial north
Lesson 1 the industrial north The north pole ____ a latitude of 90 degrees north
The north pole ____ a latitude of 90 degrees north True north vs magnetic north
True north vs magnetic north Integrated care system north east
Integrated care system north east How many regions are in texas
How many regions are in texas North and central african societies
North and central african societies Central plains cities texas
Central plains cities texas North central texas regional certification agency
North central texas regional certification agency North central plains texas landmarks
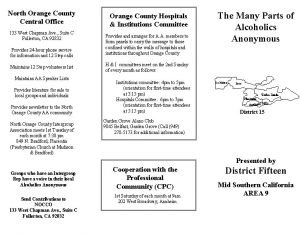
North central plains texas landmarks Orange county central office
Orange county central office North central state college jobs
North central state college jobs