201516 National Cancer Patient Experience Survey Ruth Hendy

- Slides: 8
2015/16 National Cancer Patient Experience Survey Ruth Hendy, UHBristol Lead Cancer Nurse

2015 NCPES • Inpatient and day case adult cancer patients, discharged from hospital 01/04/15 – 30/06/16 • Sent postal questionnaire Sept – Nov’ 16 • Response rate 66% • Results published July 2016 • To be repeated 2016 (results 2017) • 2015 revised methodology – Reduced questionnaire length (50 Qs re patient experience) – 14 unchanged Qs, 21 slightly amended, 15 new. – Case mix adjusted results (according to Trust populations)
Head and Neck results • Results only published for UHBristol and Glos (104 responses combined) – need 21 + responses to a Q, to be published
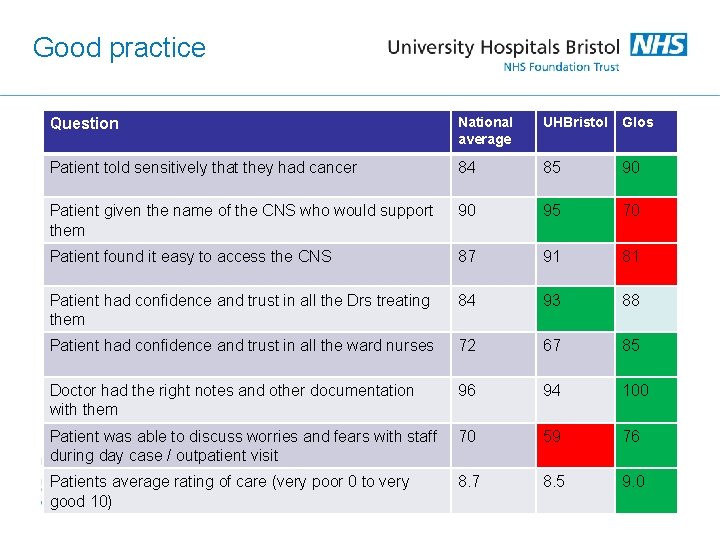
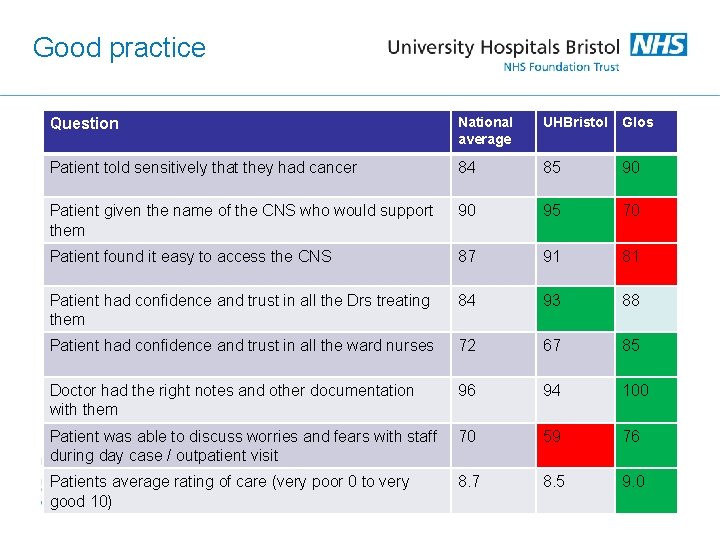
Good practice Question National average UHBristol Glos Patient told sensitively that they had cancer 84 85 90 Patient given the name of the CNS who would support them 90 95 70 Patient found it easy to access the CNS 87 91 81 Patient had confidence and trust in all the Drs treating them 84 93 88 Patient had confidence and trust in all the ward nurses 72 67 85 Doctor had the right notes and other documentation with them 96 94 100 Patient was able to discuss worries and fears with staff during day case / outpatient visit 70 59 76 Patients average rating of care (very poor 0 to very good 10) 8. 7 8. 5 9. 0
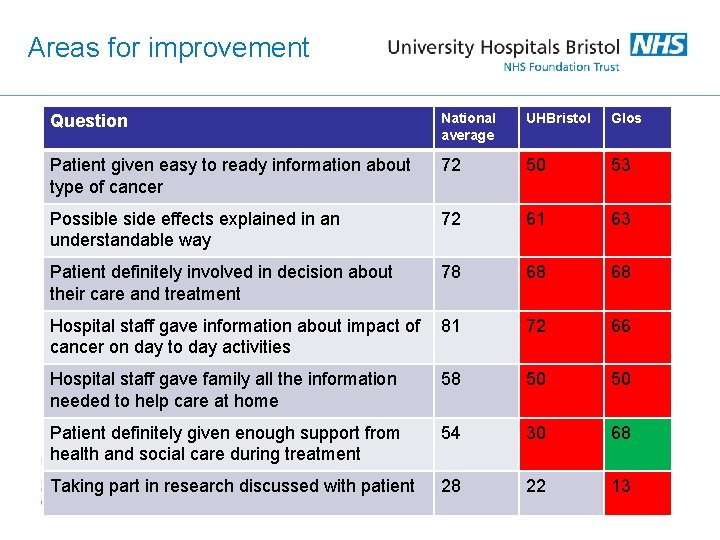
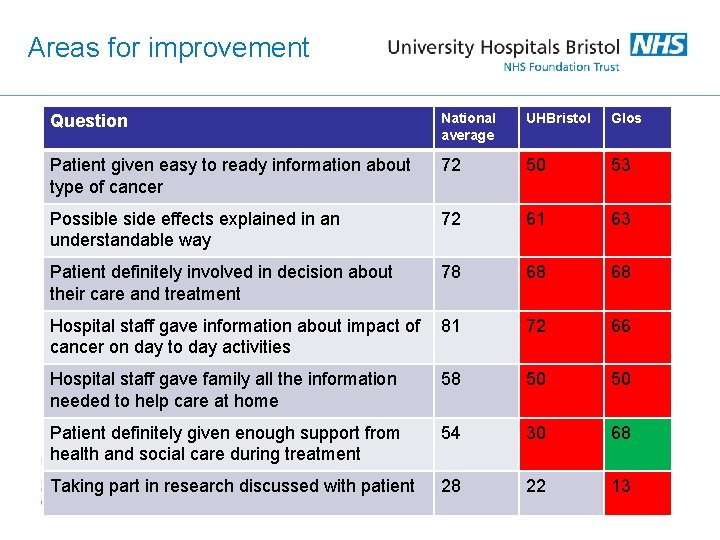
Areas for improvement Question National average UHBristol Glos Patient given easy to ready information about type of cancer 72 50 53 Possible side effects explained in an understandable way 72 61 63 Patient definitely involved in decision about their care and treatment 78 68 68 Hospital staff gave information about impact of cancer on day to day activities 81 72 66 Hospital staff gave family all the information needed to help care at home 58 50 50 Patient definitely given enough support from health and social care during treatment 54 30 68 Taking part in research discussed with patient 28 22 13
Headlines from additional 2015 patient experience activity in UHBristol+ shared care patients • ‘shared care’ provided genuine potential to negatively impact patient experience • A negative experience at the start (eg. delayed diagnosis, cancelled operation), will in most cases negatively impact the whole pathway experience • access to keyworker is paramount • ‘enough’ care – do what you say and stop me getting anxious / worried
Next steps • SSG / MDT to agree priority areas, discuss and plan local actions • Collective CNSs to continue to collaborate on shared-care across pathway – Referrals/ handovers – continuity in care – Shared information (eg. pathway leaflet) • Continued roll-out of ‘recovery package’ across SSG – Holistic needs assessments – Attendance at Health and Wellbeing events / clinics – Treatment summaries for GPs