Vaginas are SCARY Gynaecology HMO Teaching April 2018



- Slides: 29

Vaginas are SCARY … Gynaecology HMO Teaching April 2018 Dr Sarah Cox Senior O&G Registrar
Gynaecology in the ED • https: //youtu. be/3 Hw. J_0 BSN 8 k
Acute pelvic pain • In the emergency assessment of women of reproductive age it is important to exclude: – Ectopic pregnancy – Acute PID – Ovarian cyst – Endometriosis • And you may be left with a diagnosis of Primary Dysmenorrhoea
Investigation with USS • Unless you are suspecting appendicitis, intermittent ovarian torsion or a tubo-ovarian abcess, there is VERY LITTLE role for URGENT ED investigation for pelvic pain in non-pregnant, fertile females • If the b. HCG is NEGATIVE, it is NOT an ectopic pregnancy
PID • Diagnosis requires a patient at risk • Usually younger patient (15 – 25 years) • New partner or multiple partners • Or a partner at risk e. g. one that travels • • It is a bilateral disease Pelvic peritoneal tenderness is a subtle sign WCC & ESR or C-reactive protein can be useful Requires careful microbiology • Test for all STD’s simultaneously • A role for laparoscopy in diagnosis
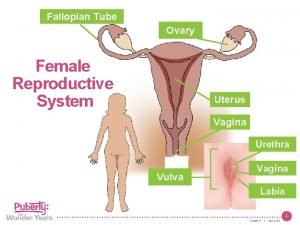
What is PID? • Inflammation of female pelvic structures • Ascending spread of infection from the cervix through the uterus, to fallopian tubes, ovaries and adjacent peritoneum • Upper genital tract infection • It is not infection in the vagina or vulva
Two types of PID • Acute • • Patient has generalised symptoms Lasts a few days May recur in episodes Very infectious in this stage • Chronic • • Patient may have no symptoms Occurs over months and years Progressive organ damage & change May burn out (arrest)
Causes of PID • 85 – 95% is due to specific sexually transmitted organisms • Neisseria gonorrhoea • Chlamydia trachomatis • Others e. g. Mycoplasma species • 5 – 15% begins after reproductive tract damage • From pregnancy • From surgical procedures e. g. D&C • Includes insertion of IUCD
PID Risk Factors • • Age of 1 st intercourse Number of sexual partners Number of sexual contacts by the sexual partner Cultural practices • Polygamy, • Sex workers • Attitudes to menstruation and pregnancy • • Frequency of intercourse (Age) IUCD design Poor health resources Antibiotic exposure (resistance)
PID • Requires a high index of suspicion in a patient “at risk” when there is: • • Lower abdominal pain (90%) Fever (sometimes with malaise, vomiting) Mucopurulent discharge from cervix Pelvic tenderness • Tests • • Raised WCC Endocervical swab for organisms or PCR Ultrasound evidence of pelvic fluid collections Laparoscopy
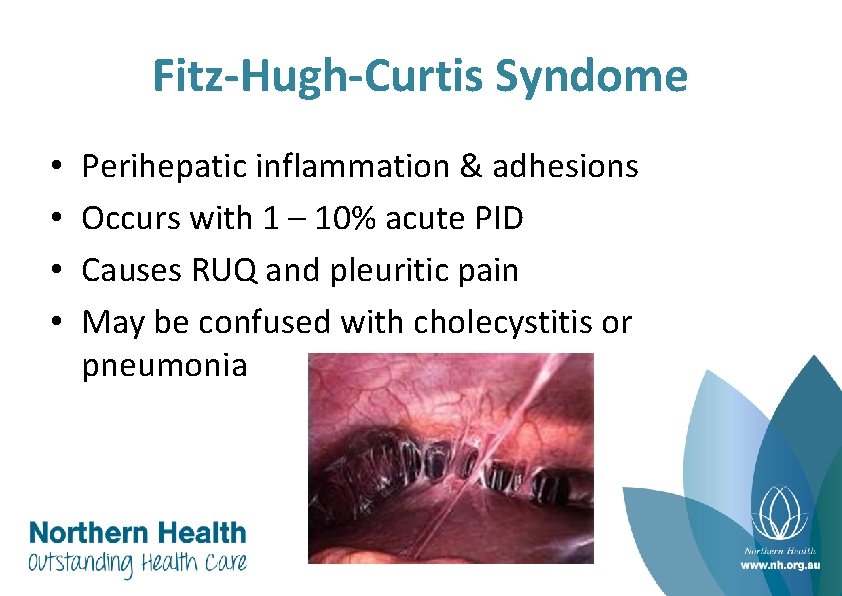
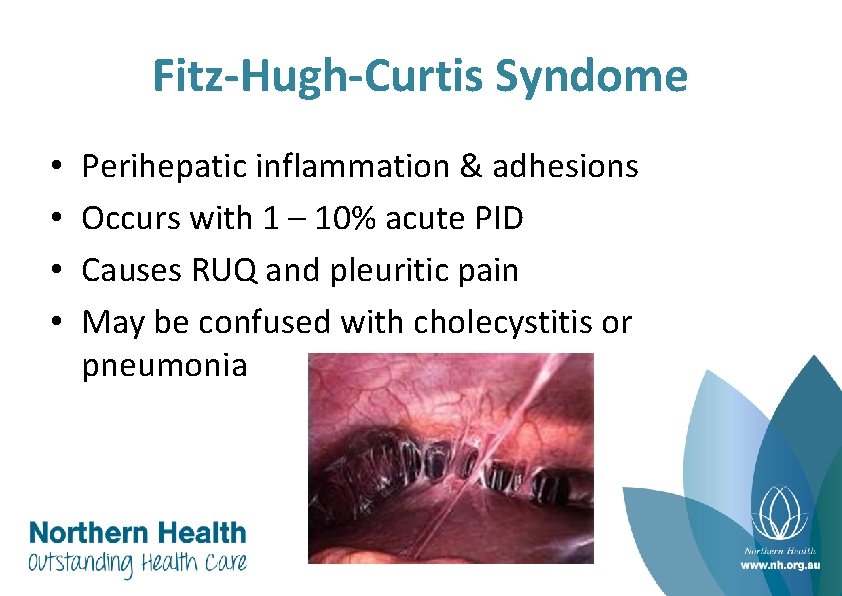
Fitz-Hugh-Curtis Syndome • • Perihepatic inflammation & adhesions Occurs with 1 – 10% acute PID Causes RUQ and pleuritic pain May be confused with cholecystitis or pneumonia
Ovarian cysts • Very common • But not always the source of pain • Pain can be due to: • • Rapid enlargement Rupture Haemorrhage - typical of the corpus luteum Torsion (rare) • Ultrasound is both a boon and a bane because • • Paraovarian cysts • Mesenetric cysts & Adhesive collections • Hydrosalpinx, Bladder or even Ureter May be imaged but do not cause acute pain
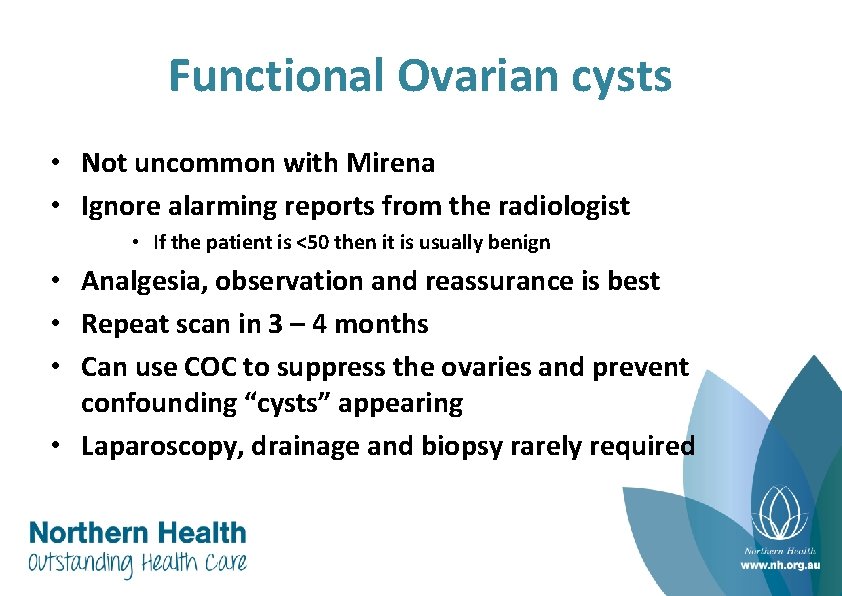
Functional Ovarian cysts • Not uncommon with Mirena • Ignore alarming reports from the radiologist • If the patient is <50 then it is usually benign • Analgesia, observation and reassurance is best • Repeat scan in 3 – 4 months • Can use COC to suppress the ovaries and prevent confounding “cysts” appearing • Laparoscopy, drainage and biopsy rarely required
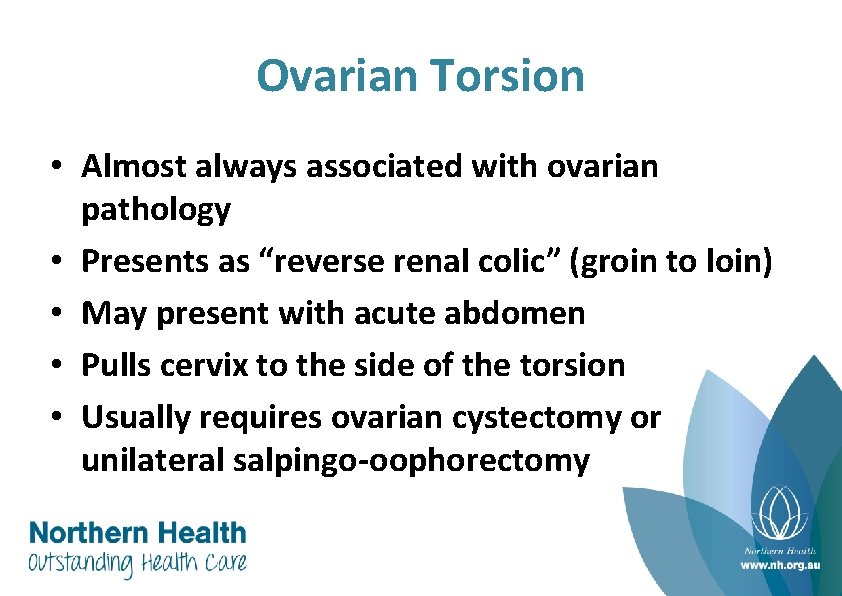
Ovarian Torsion • Almost always associated with ovarian pathology • Presents as “reverse renal colic” (groin to loin) • May present with acute abdomen • Pulls cervix to the side of the torsion • Usually requires ovarian cystectomy or unilateral salpingo-oophorectomy
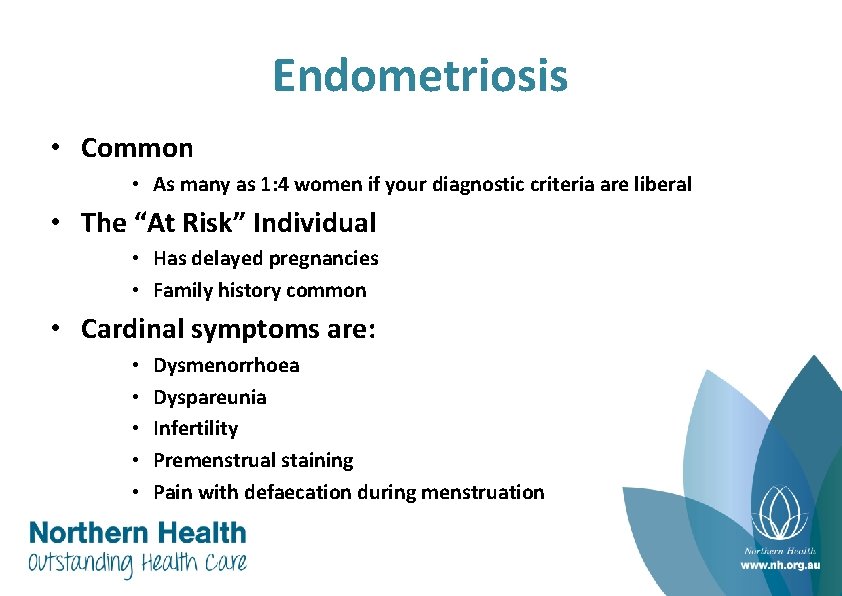
Endometriosis • Common • As many as 1: 4 women if your diagnostic criteria are liberal • The “At Risk” Individual • Has delayed pregnancies • Family history common • Cardinal symptoms are: • • • Dysmenorrhoea Dyspareunia Infertility Premenstrual staining Pain with defaecation during menstruation
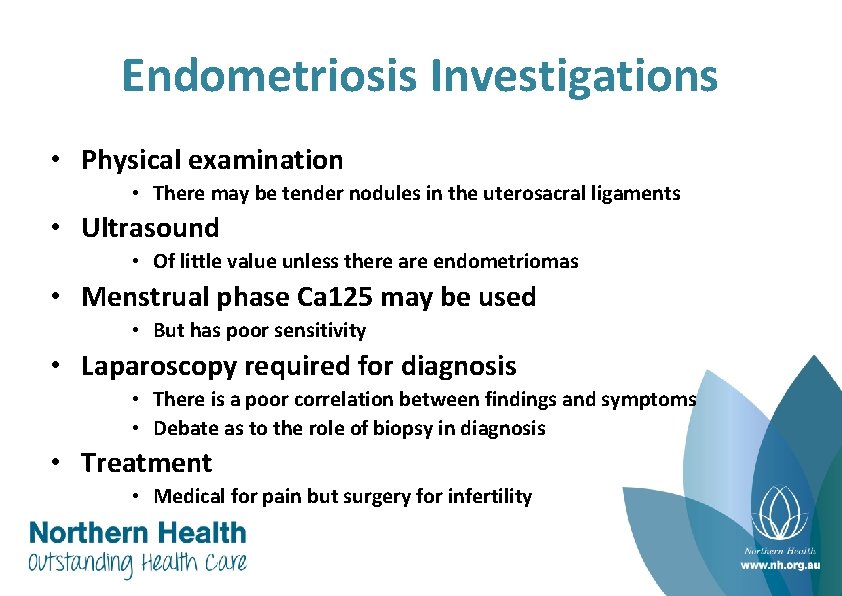
Endometriosis Investigations • Physical examination • There may be tender nodules in the uterosacral ligaments • Ultrasound • Of little value unless there are endometriomas • Menstrual phase Ca 125 may be used • But has poor sensitivity • Laparoscopy required for diagnosis • There is a poor correlation between findings and symptoms • Debate as to the role of biopsy in diagnosis • Treatment • Medical for pain but surgery for infertility
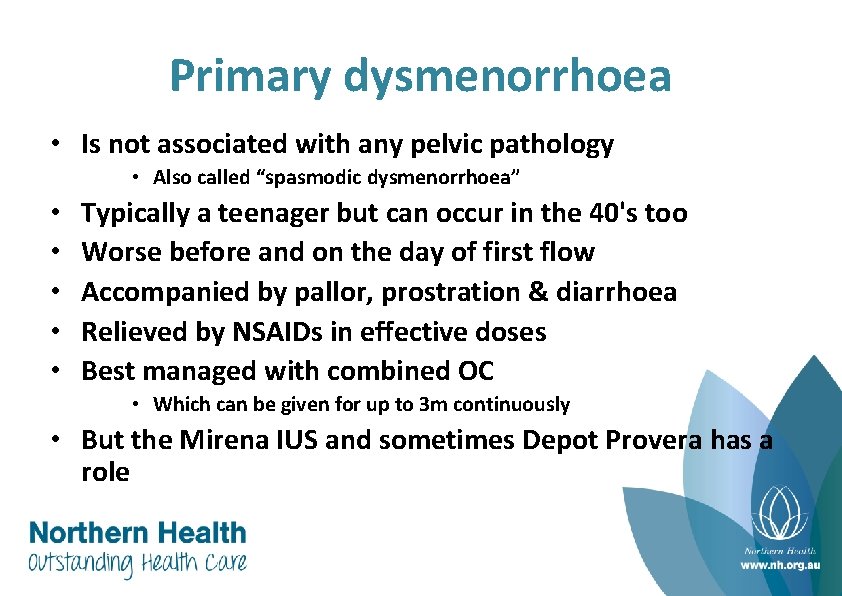
Primary dysmenorrhoea • Is not associated with any pelvic pathology • Also called “spasmodic dysmenorrhoea” • • • Typically a teenager but can occur in the 40's too Worse before and on the day of first flow Accompanied by pallor, prostration & diarrhoea Relieved by NSAIDs in effective doses Best managed with combined OC • Which can be given for up to 3 m continuously • But the Mirena IUS and sometimes Depot Provera has a role
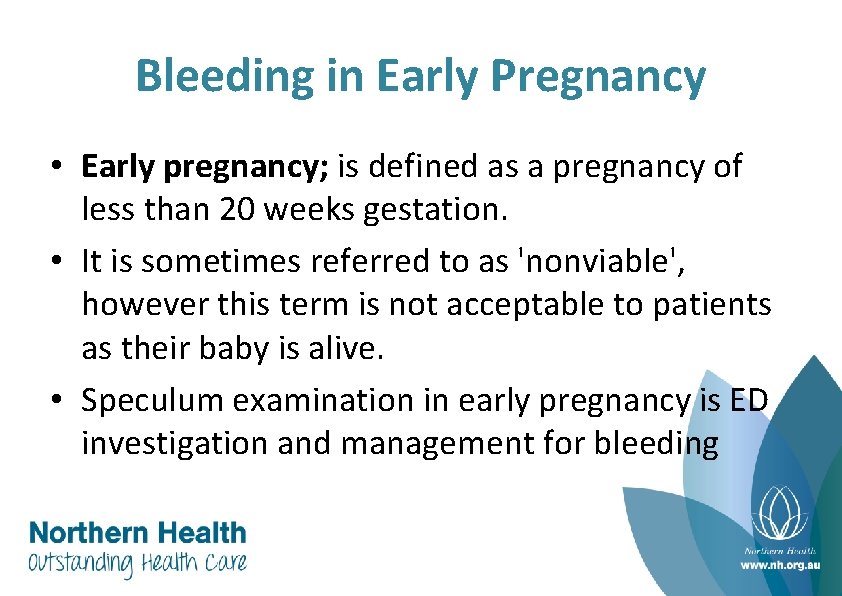
Bleeding in Early Pregnancy • Early pregnancy; is defined as a pregnancy of less than 20 weeks gestation. • It is sometimes referred to as 'nonviable', however this term is not acceptable to patients as their baby is alive. • Speculum examination in early pregnancy is ED investigation and management for bleeding
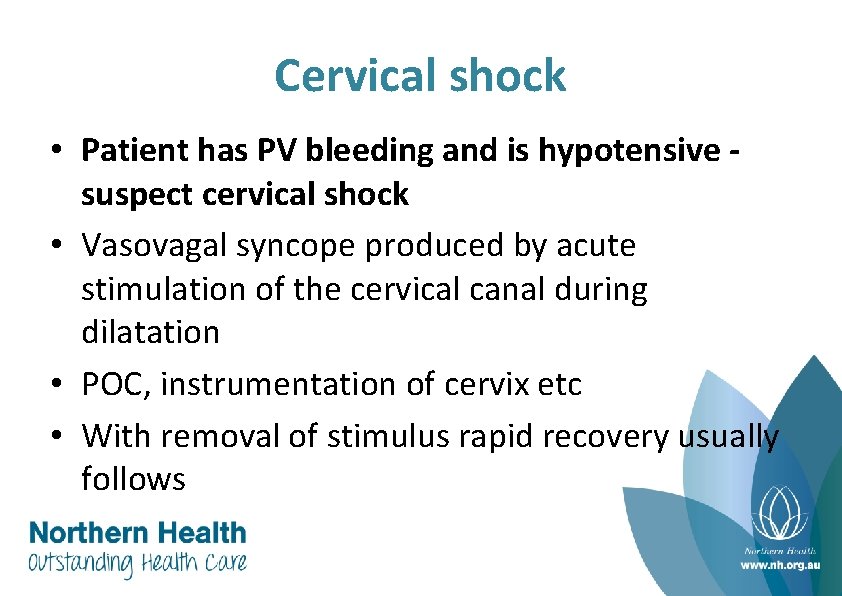
Cervical shock • Patient has PV bleeding and is hypotensive suspect cervical shock • Vasovagal syncope produced by acute stimulation of the cervical canal during dilatation • POC, instrumentation of cervix etc • With removal of stimulus rapid recovery usually follows
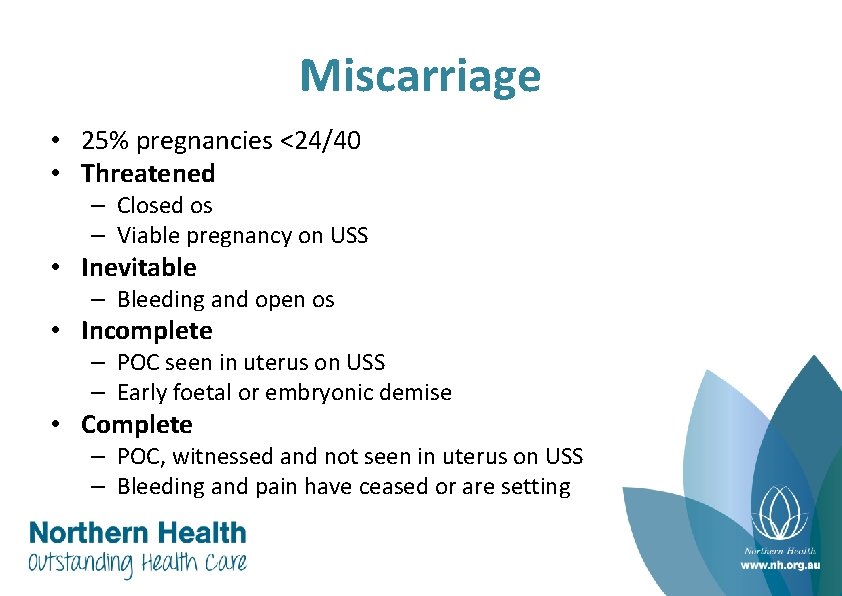
Miscarriage • 25% pregnancies <24/40 • Threatened – Closed os – Viable pregnancy on USS • Inevitable – Bleeding and open os • Incomplete – POC seen in uterus on USS – Early foetal or embryonic demise • Complete – POC, witnessed and not seen in uterus on USS – Bleeding and pain have ceased or are setting
b. HCG • Threshold βHCG – level at which intrauterine gestational sac can be seen with TVUS • 1000 -2000 IU/L (6500 IU/L for TAUS) • β-HCG – First 60 days (weeks 4 -8) doubles every 1. 4 to 2. 1 days • Taking two β-HCG 48 hours apart can be helpful • <20% increase or a reduction it is 100% sensitive for foetal demise or ectopic • If β-HCG >50, 000 ectopic pregnancy very unlikely

Assessment of Early Pregnancy • Quantative pregnancy test (useful if uterine pregnancy prev. confirmed on USS but suspected fetal demise or heterotopic HOWEVER USS is preferred in this instance) • LMP and menstrual history • Bleeding - amount, compared to usual period, any clots/tissue • Previous ectopic, PID, operation on fallopian tube, pregnancy whilst using IUD • Pain - severity and site • Establish physiological status, examine abdomen • Keep fasting • Analgesia • Group and hold esp Rh status for ? Anti-D
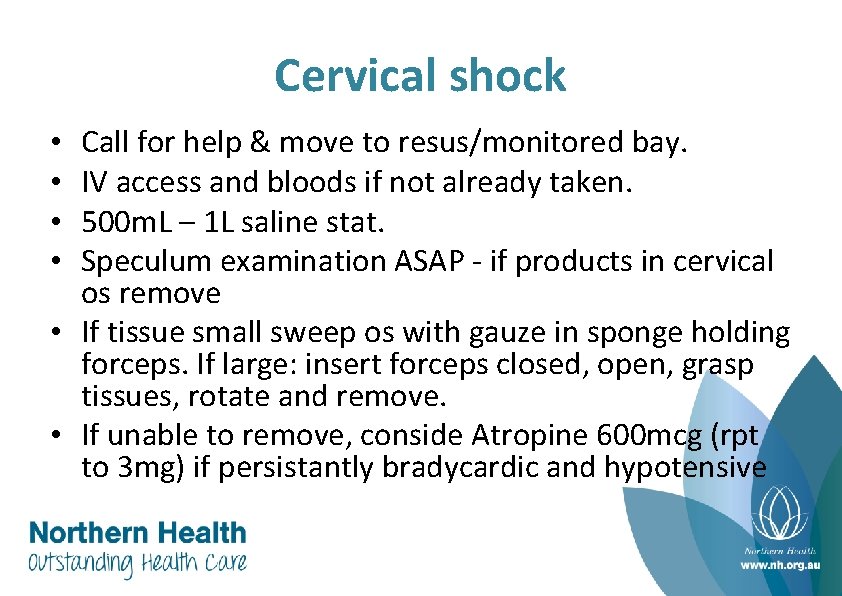
Cervical shock Call for help & move to resus/monitored bay. IV access and bloods if not already taken. 500 m. L – 1 L saline stat. Speculum examination ASAP - if products in cervical os remove • If tissue small sweep os with gauze in sponge holding forceps. If large: insert forceps closed, open, grasp tissues, rotate and remove. • If unable to remove, conside Atropine 600 mcg (rpt to 3 mg) if persistantly bradycardic and hypotensive • •
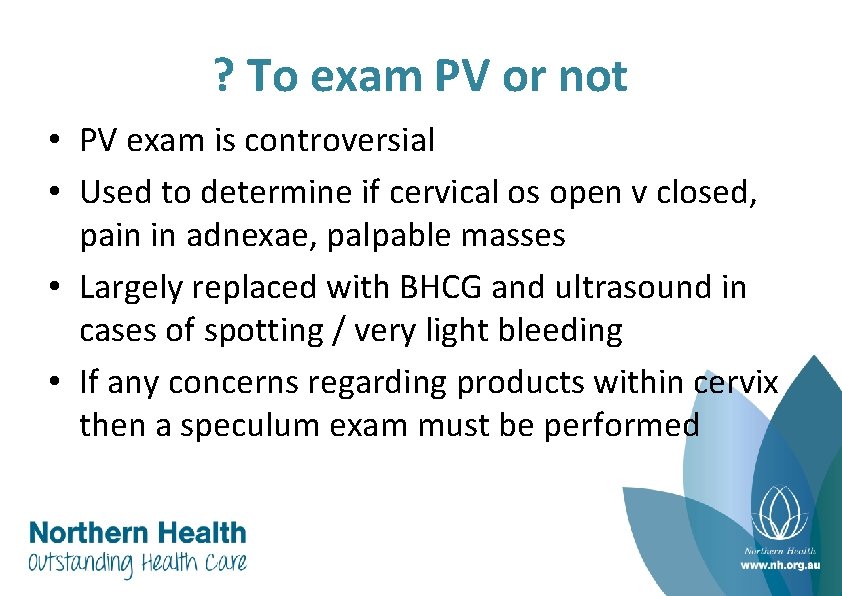
? To exam PV or not • PV exam is controversial • Used to determine if cervical os open v closed, pain in adnexae, palpable masses • Largely replaced with BHCG and ultrasound in cases of spotting / very light bleeding • If any concerns regarding products within cervix then a speculum exam must be performed

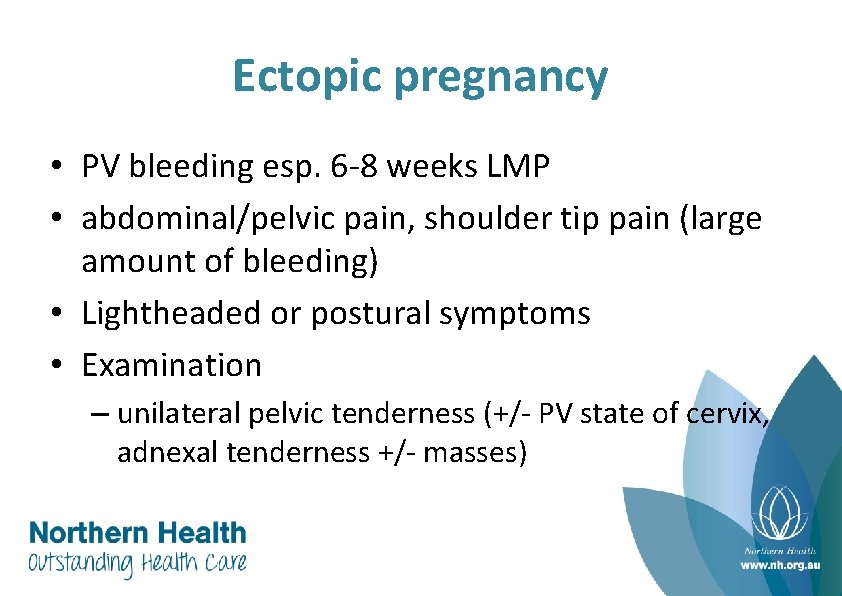
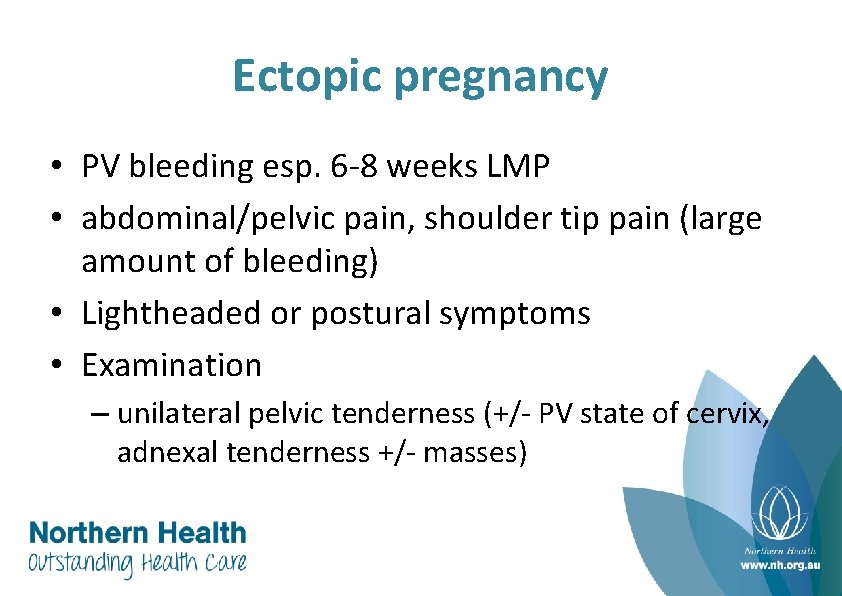
Ectopic pregnancy • PV bleeding esp. 6 -8 weeks LMP • abdominal/pelvic pain, shoulder tip pain (large amount of bleeding) • Lightheaded or postural symptoms • Examination – unilateral pelvic tenderness (+/- PV state of cervix, adnexal tenderness +/- masses)
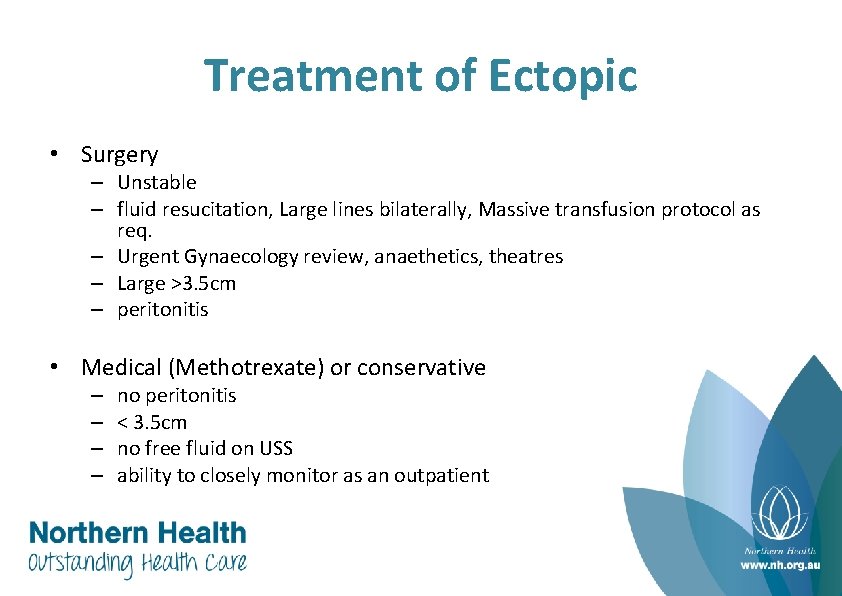
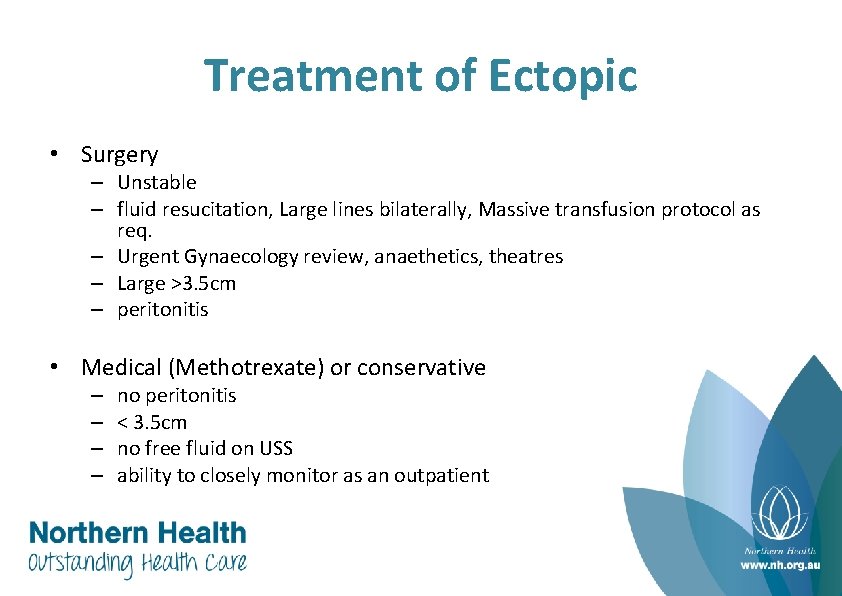
Treatment of Ectopic • Surgery – Unstable – fluid resucitation, Large lines bilaterally, Massive transfusion protocol as req. – Urgent Gynaecology review, anaethetics, theatres – Large >3. 5 cm – peritonitis • Medical (Methotrexate) or conservative – – no peritonitis < 3. 5 cm no free fluid on USS ability to closely monitor as an outpatient
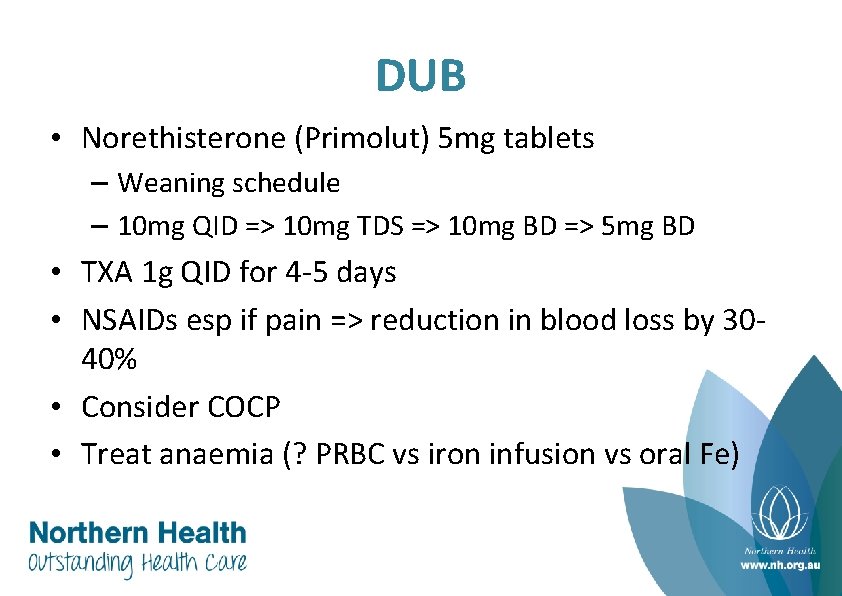
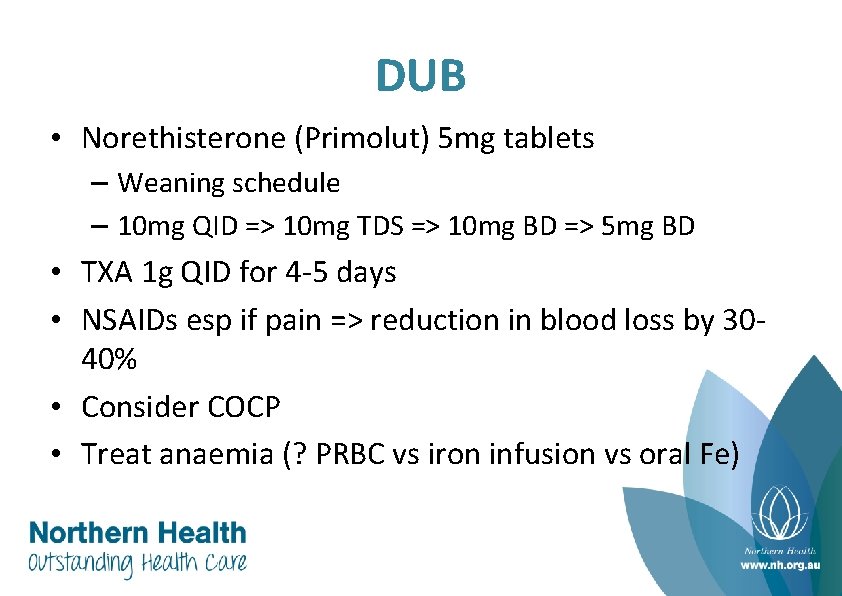
DUB • Norethisterone (Primolut) 5 mg tablets – Weaning schedule – 10 mg QID => 10 mg TDS => 10 mg BD => 5 mg BD • TXA 1 g QID for 4 -5 days • NSAIDs esp if pain => reduction in blood loss by 3040% • Consider COCP • Treat anaemia (? PRBC vs iron infusion vs oral Fe)
 Mikael ferm
Mikael ferm Poultry reproductive system
Poultry reproductive system Cervix definition
Cervix definition H3387 010 01 - hmo
H3387 010 01 - hmo Uc blue and gold hmo
Uc blue and gold hmo H3359 019 01 - hmo
H3359 019 01 - hmo What does hmo stand for
What does hmo stand for Hmo research network
Hmo research network Hmo meaning
Hmo meaning Psbp health net ppo
Psbp health net ppo Vivity hmo cedars sinai
Vivity hmo cedars sinai 99366 cpt code
99366 cpt code Hmo gesundheitsplan
Hmo gesundheitsplan Harvard pilgrim hmo
Harvard pilgrim hmo Harbourside gynaecology centre
Harbourside gynaecology centre Ninewells hospital outpatients area 3
Ninewells hospital outpatients area 3 Lcb gynae
Lcb gynae Bangalore society of obstetrics & gynaecology
Bangalore society of obstetrics & gynaecology B a f c j e
B a f c j e Two sentence horror stories
Two sentence horror stories Anixir
Anixir Compound complex sentences
Compound complex sentences How would you describe torrence's viewpoint on scary tales
How would you describe torrence's viewpoint on scary tales I am big pentameter
I am big pentameter Intimate antonym
Intimate antonym Extreme adjective for boring
Extreme adjective for boring Scary hyperbole examples
Scary hyperbole examples Scary tone examples
Scary tone examples Scary poems
Scary poems Claude cahun autobiography
Claude cahun autobiography