Urotherapy definitions and evidence Ann Raes Department of
- Slides: 16
Urotherapy: definitions and evidence Ann Raes Department of Pediatric Nephrology, University Hospital Ghent, Belgium Spring School 01 -06 June 2018
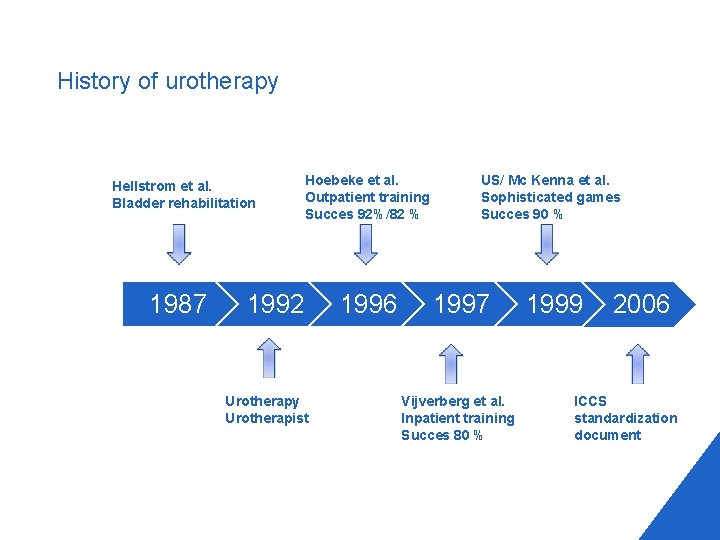
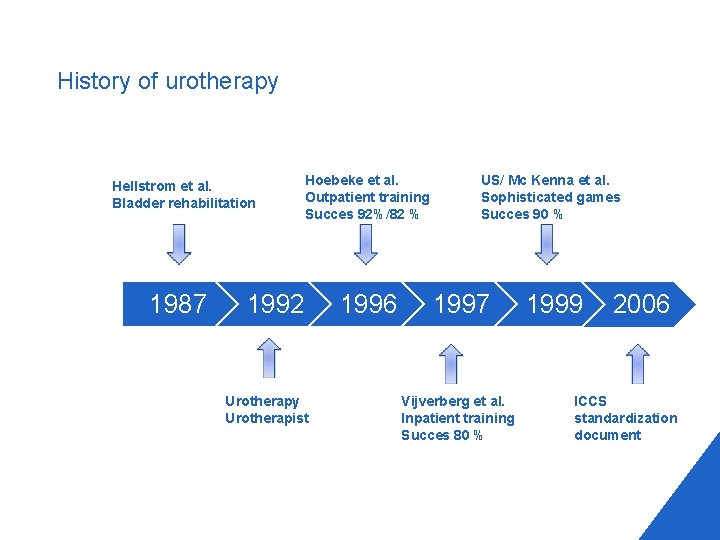
History of urotherapy Hellstrom et al. Bladder rehabilitation 1987 Hoebeke et al. Outpatient training Succes 92%/82 % 1992 Urotherapy Urotherapist 1996 US/ Mc Kenna et al. Sophisticated games Succes 90 % 1997 Vijverberg et al. Inpatient training Succes 80 % 1999 2006 ICCS standardization document
What is urotherapy ? 4 Nonsurgical, nonpharmacological treatment for 4 LUT dysfunction 4 Boweldysfunction 4 Combination of cognitive, behavioral and fysical training 4 Multidisciplinary approach 4 wide field of healthcare professionals
Standard urotherapy 4 Information and demystification 4 Education (family + child) on how to resolve the LUT (bowel) dysfunction 4 Life-style advice 4 Bladder /bowel diary 4 Motivation and reward
Advance urotherapy 4 Pelvic floor muscle retraining 4 Awareness and coordination 4(Uroflow)Biofeedbacktraining 4 Electrical stimulation (Neuromodulation) 4 TENS/PENS 4 Clean intermittent catheterization (>> residual volume) 4 Psychotherapy 4 Psychological comorbidity
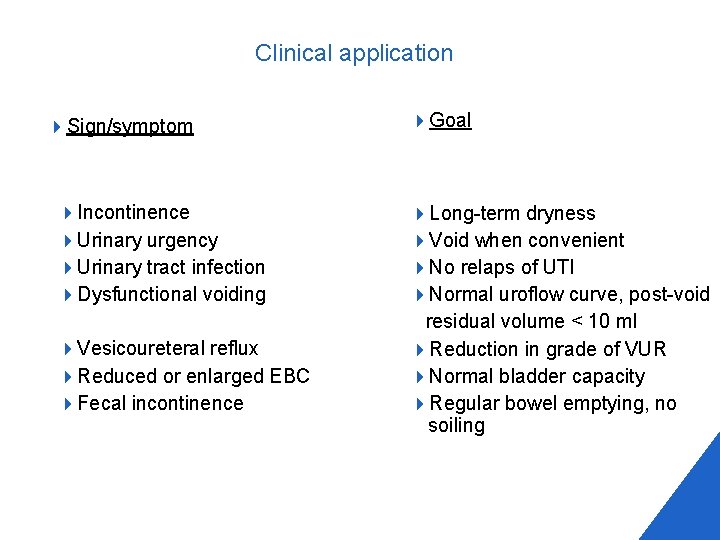
Clinical application 4 Sign/symptom 4 Incontinence 4 Urinary urgency 4 Urinary tract infection 4 Dysfunctional voiding 4 Vesicoureteral reflux 4 Reduced or enlarged EBC 4 Fecal incontinence 4 Goal 4 Long-term dryness 4 Void when convenient 4 No relaps of UTI 4 Normal uroflow curve, post-void residual volume < 10 ml 4 Reduction in grade of VUR 4 Normal bladder capacity 4 Regular bowel emptying, no soiling
Urotherapy in nocturnal enuresis 4 Appropriate fluid intake 4 regular fluid intake during the day 4 minimization of fluid and solute intake 1 -2 hours before sleep 4 Regular voiding during daytime 4 Good voiding posture 4 Emptying the bladder before going to bed 4 A diary of dry and wet nights should be kept for 4 Selfmonitoring and motivation 4 Treatment of constipation
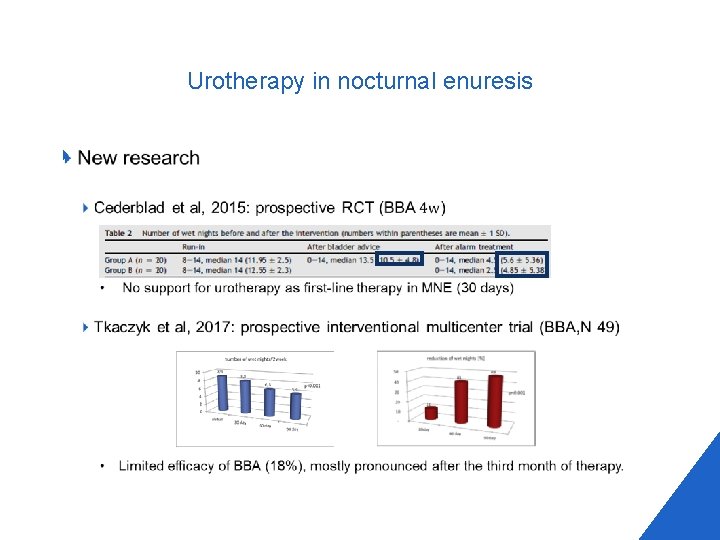
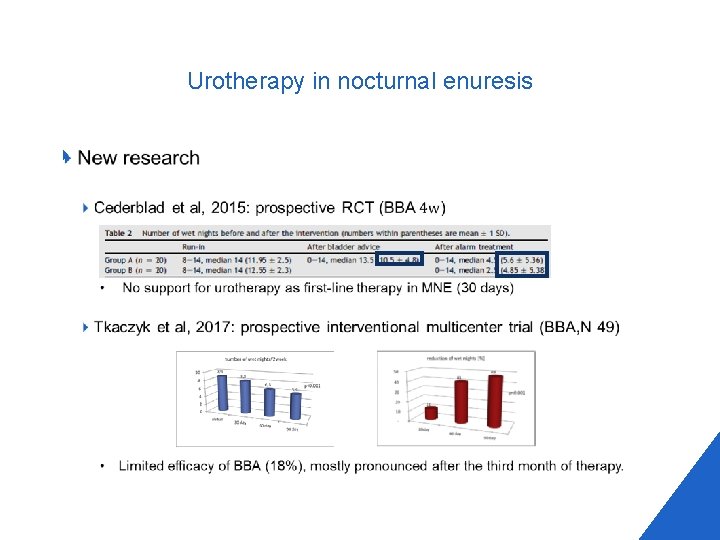
Urotherapy in nocturnal enuresis 4
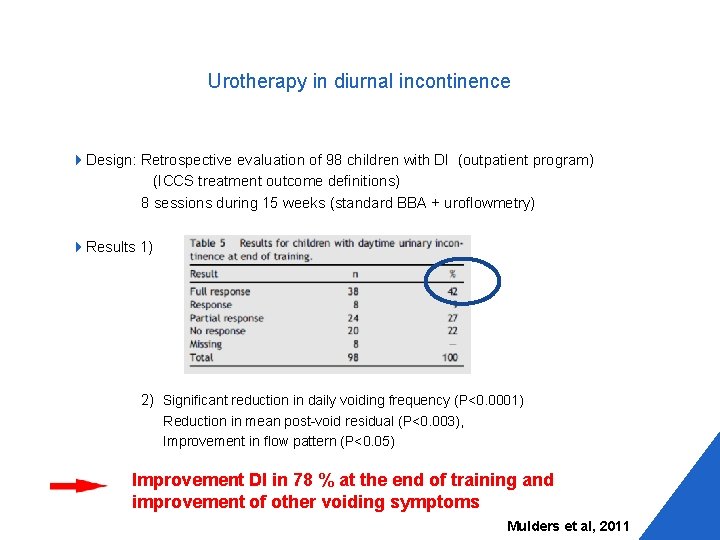
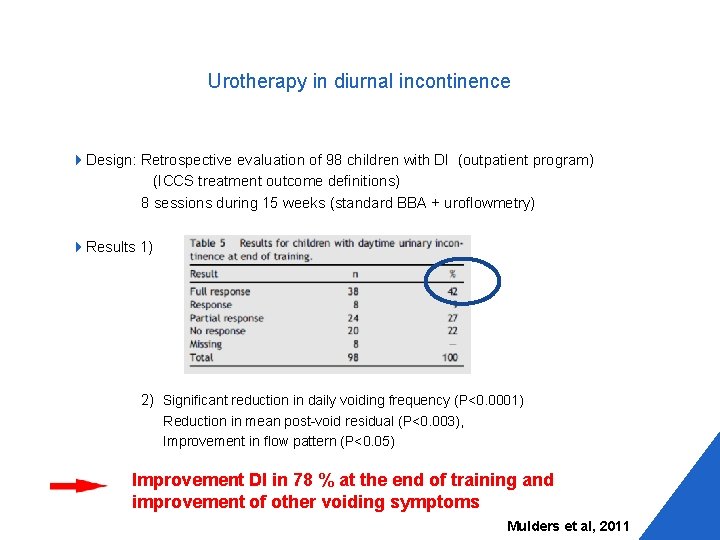
Urotherapy in diurnal incontinence 4 Design: Retrospective evaluation of 98 children with DI (outpatient program) (ICCS treatment outcome definitions) 8 sessions during 15 weeks (standard BBA + uroflowmetry) 4 Results 1) 2) Significant reduction in daily voiding frequency (P<0. 0001) Reduction in mean post-void residual (P<0. 003), Improvement in flow pattern (P<0. 05) Improvement DI in 78 % at the end of training and improvement of other voiding symptoms Mulders et al, 2011
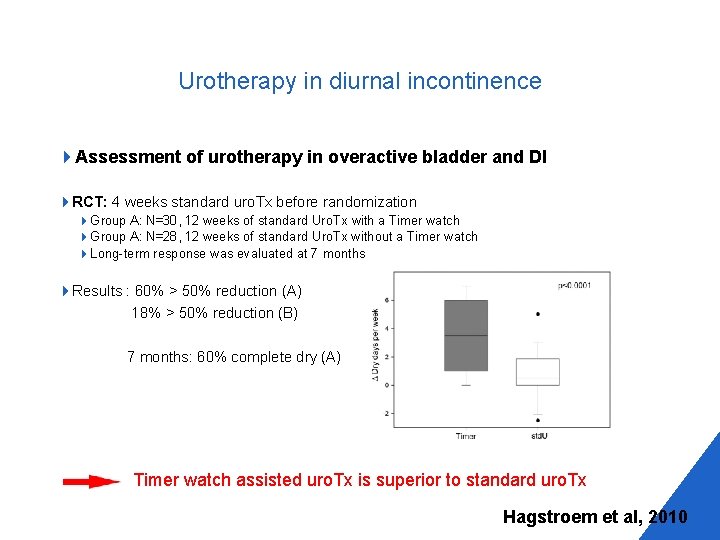
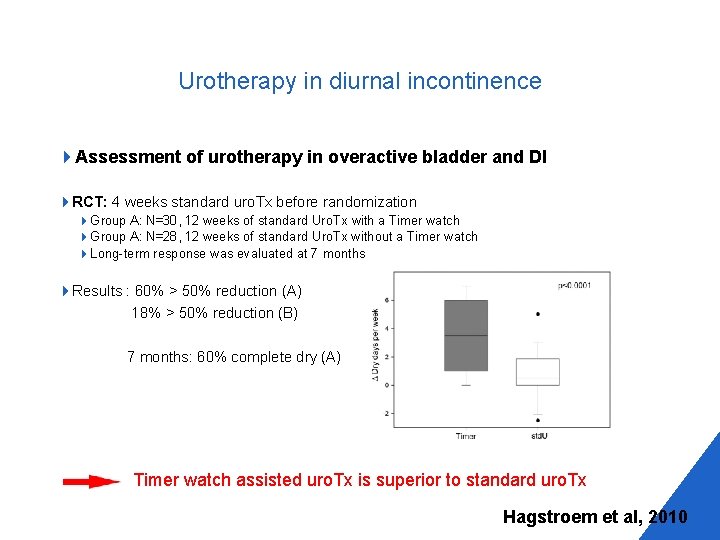
Urotherapy in diurnal incontinence 4 Assessment of urotherapy in overactive bladder and DI 4 RCT: 4 weeks standard uro. Tx before randomization 4 Group A: N=30, 12 weeks of standard Uro. Tx with a Timer watch 4 Group A: N=28, 12 weeks of standard Uro. Tx without a Timer watch 4 Long-term response was evaluated at 7 months 4 Results : 60% > 50% reduction (A) 18% > 50% reduction (B) 7 months: 60% complete dry (A) Timer watch assisted uro. Tx is superior to standard uro. Tx Hagstroem et al, 2010
Urotherapy in diurnal incontinence 4 Schafer et al, 2017: meta-analysis 4 18 studies (154) • N: 1502 treated with standard urotherapy (SU) 4 Effectiveness of SU in reduction in DI in children and adolescents Standard urotherapy is considered to be an effective intervention in comparison to expected cure rates based on spontaneous remission
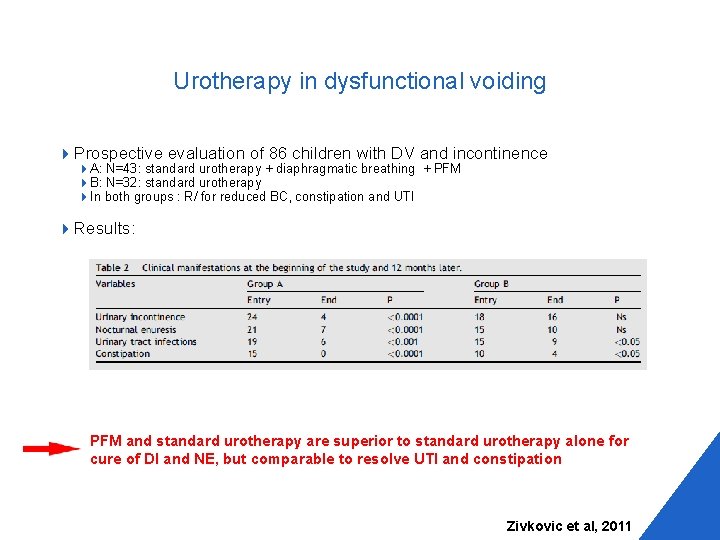
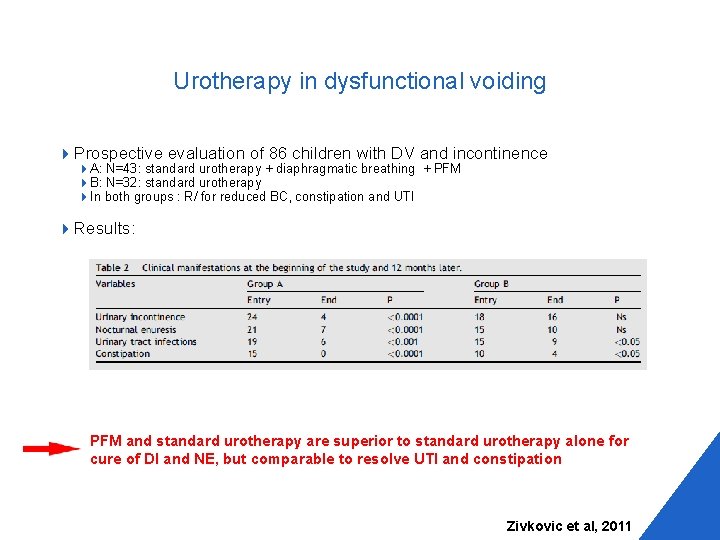
Urotherapy in dysfunctional voiding 4 Prospective evaluation of 86 children with DV and incontinence 4 A: N=43: standard urotherapy + diaphragmatic breathing + PFM 4 B: N=32: standard urotherapy 4 In both groups : R/ for reduced BC, constipation and UTI 4 Results: PFM and standard urotherapy are superior to standard urotherapy alone for cure of DI and NE, but comparable to resolve UTI and constipation Zivkovic et al, 2011
Biofeedback in dysfunctional voiding 4 Desantis et al. , 2011: systematic review 4 effectiveness in reduction in UTI and ID 4 27 studies (1 RCT and 26 case series) Positive results 80 % benefited from this treatment 4 Fazeli et al. , 2015: meta-analysis of RCT 4 effectiveness in reduction in UTI and ID 45 eligible studies (382 participants) were pooled Negative results Similar in incontinence in biofeedback and control groups No significant difference in likelihood of urinary tract infection
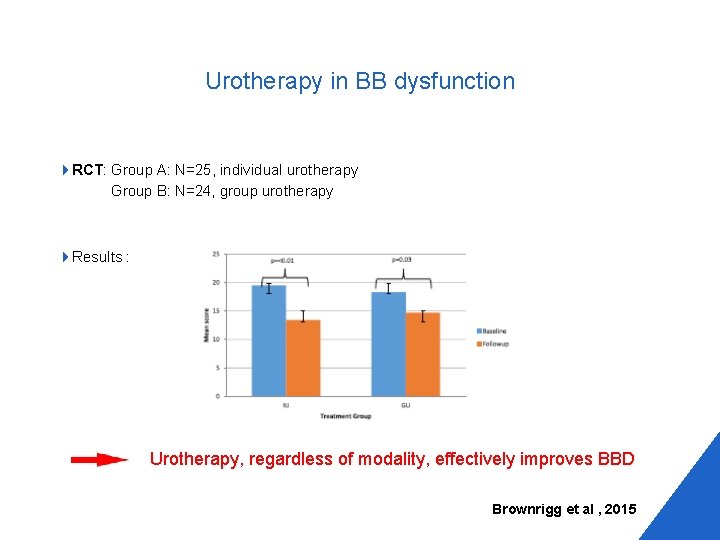
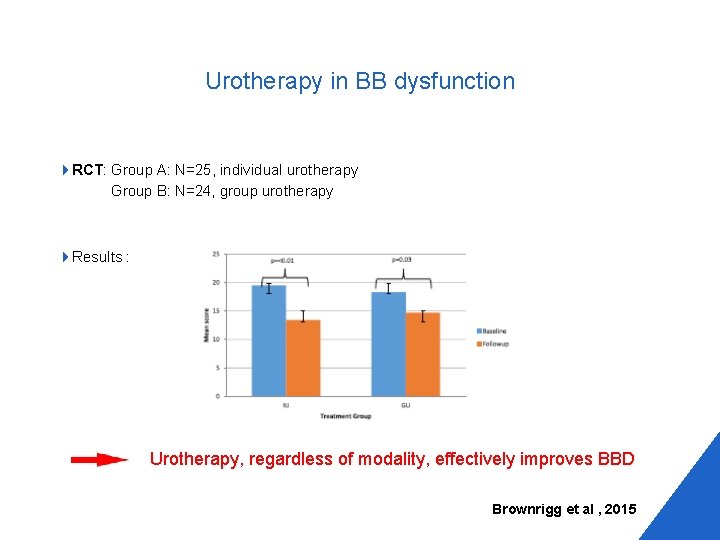
Urotherapy in BB dysfunction 4 RCT: Group A: N=25, individual urotherapy Group B: N=24, group urotherapy 4 Results : Urotherapy, regardless of modality, effectively improves BBD Brownrigg et al , 2015
Lessons from thirty years of urotherapy 4 Standard urotherapy is a valid therapeutic strategy for children with LUTS, but recommendation in MNE is questioned. 4 Despite adequate work-up a core of 20 -40% of children with LUTS at long-term follow up are resistant to standard urotherapy and need advanced urotherapy. 4 Treatment of defaecation problems in children with BBD enhances successful management of LUTS 4 Urotherapy effectively reduces symptoms related to BBD
Lessons from thirty years of urotherapy 4 There is need for RCT 4 With clear defined study groups 4 With standardized treatment modalities 4 With longer treatment- and follow-up periods 4 To be able to evaluate the effectiveness of each modality 4 To be able to compare the results of different programs 4 To define the best program
 Ann raes
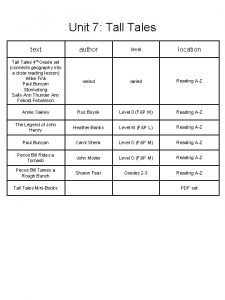
Ann raes Davy crockett character traits
Davy crockett character traits Second best bed poem
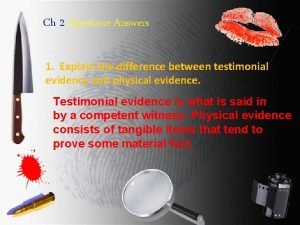
Second best bed poem Why does individual evidence have high probative value
Why does individual evidence have high probative value Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Secondary sources
Secondary sources Primary evidence vs secondary evidence
Primary evidence vs secondary evidence Primary evidence vs secondary evidence
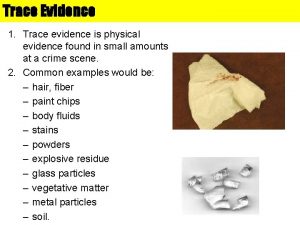
Primary evidence vs secondary evidence Why is fiber considered class evidence
Why is fiber considered class evidence Class vs individual evidence
Class vs individual evidence Individual vs class evidence
Individual vs class evidence Ecological fallacy meaning
Ecological fallacy meaning General department of criminal evidence
General department of criminal evidence Irony in julius caesar
Irony in julius caesar The problem of concept drift: definitions and related work
The problem of concept drift: definitions and related work The correct shutoff procedure for an oxyacetylene torch is:
The correct shutoff procedure for an oxyacetylene torch is: