TIA The calm before the storm Aims TIA

TIA The calm before the storm
Aims • TIA – what it is and what it’s not • Assessment and investigations • Management • Discuss risk factors • Secondary stroke prevention Slide 2
Stroke Definition v A transient ischemic attack (TIA) is defined as stroke symptoms and signs that resolve within 24 hours. In addition visual symptoms such as sudden onset of monocular visual loss should be included. (The National Institute of Clinical Excellence 2008 (NICE) v ASA – Transient episode of neurological dysfunction caused by focal brain, spinal cord or retinal ischaemia without evidence of acute infarction Slide 3
Incidence • 35 people out of every 100, 000 each year have a TIA. • 10– 20% of those who have had a TIA will go on to have a stroke within a month & the greatest risk is within the first 48 hours. Slide 4
Diagnostic challenges • Event occurred in the past, often not witnessed • -30% delay seeking medical attention for >24 hours • Reliant on patient’s history • -Pt may be unable to completely recall symptoms • -May use vague descriptions “dizziness”, “confused heaviness” • Clinical examination usually normal • Many causes of transient neurology (50% of pts referred to TIA clinic) Slide 5
Non focal symptoms • Faintness • Light headedness • General weakness • Confusion • Syncope • Non specific dizziness Slide 6
Transient Focal Neurology • TIA • epilepsy • Migraine aura (+/- headache) • Transient Global Amnesia • Multiple sclerosis • Intracranial structural lesion • Metabolic disturbance • Many more Slide 7
Transient monocular blindness (Amaurosis Fugax) • Sudden loss of vision in the whole or part of the visual field of one eye. Lasts seconds-minutes • Retinal ischeamia • Atherothromboembolism from ICA or cardiac embolism • Can be other cause of TMB eg glaucoma, Central or branch retinal vein thrombosis • Glaucoma • Retinal haemorrhage Slide 8
Case study 1 • At the gym, drove home • According to wife –”confused”, repeatedly asking “What day is it? • No limb or facial weakness • Symptoms resolved after 4 hours • Pt has no recollection of event Is this a TIA Slide 9
Transient Global Amnesia • Temporary, isolated disorder of memory • Impaired ability to form new memory • Asks pertinent questions repeatedly • Symptoms last < 24 hours • Unable to recall episode once recovered • Precise pathophysiology unclear Slide 10
Transient Global Amnesia • 3/100, 000 cases per annum • More common in males • Precipitants – physical exertion, cold water exposure, overwhelming emotional stress, pain • Annual recurrence rate 3% • No increased risk of stroke Slide 11
Case Study 2 – 27 year old male • Sudden onset numbness and weakness in (L) hand • Resolved within 1 hour • No past medical history IS THIS A TIA Slide 12
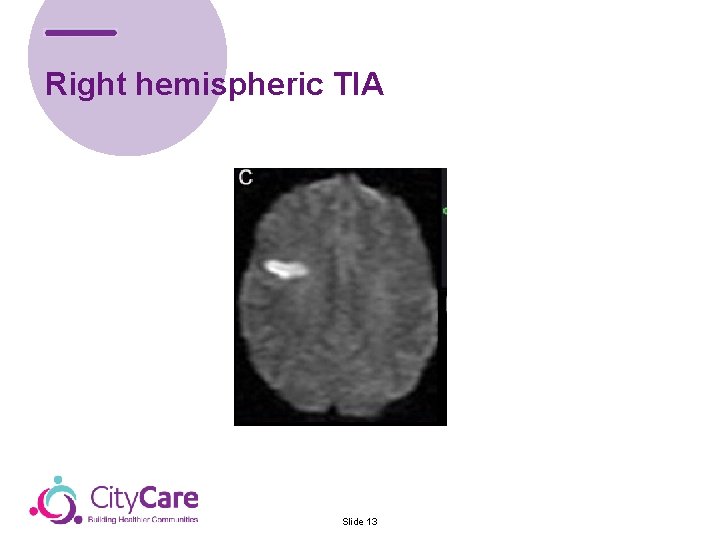
Right hemispheric TIA Slide 13
TIA – what's the urgency? • Common • Serious recurrent vascular events • Stroke, MI, death • Most occur in first few days • 5% stroke within 2 days • 11% stroke within 1 week Slide 14
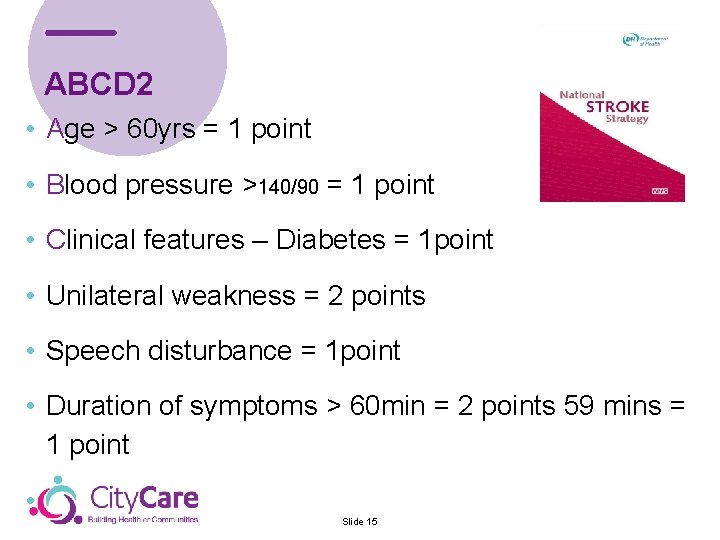
ABCD 2 • Age > 60 yrs = 1 point • Blood pressure >140/90 = 1 point • Clinical features – Diabetes = 1 point • Unilateral weakness = 2 points • Speech disturbance = 1 point • Duration of symptoms > 60 min = 2 points 59 mins = 1 point • Slide 15
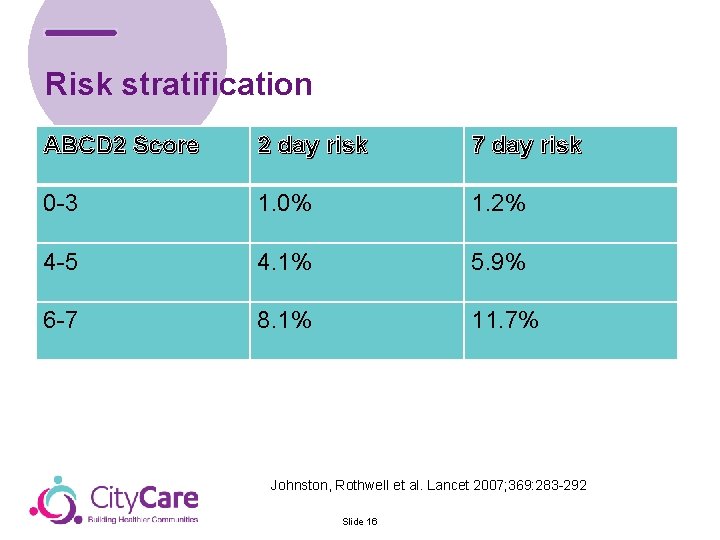
Risk stratification ABCD 2 Score 2 day risk 7 day risk 0 -3 1. 0% 1. 2% 4 -5 4. 1% 5. 9% 6 -7 8. 1% 11. 7% Johnston, Rothwell et al. Lancet 2007; 369: 283 -292 Slide 16
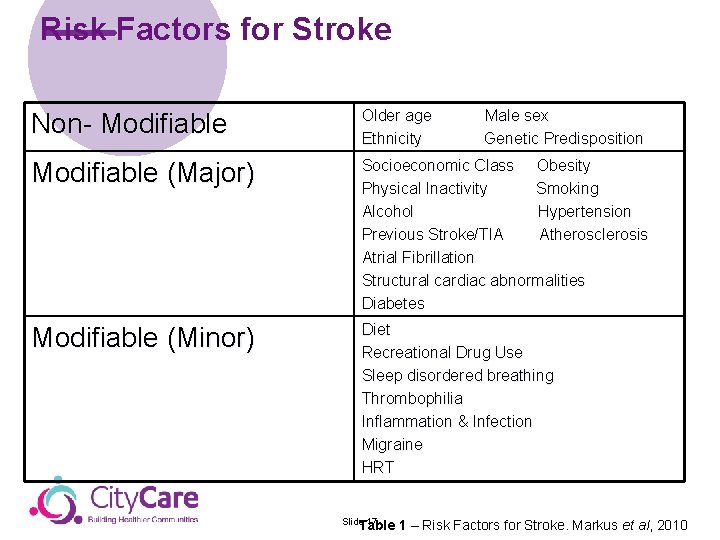
Risk Factors for Stroke Non- Modifiable Older age Ethnicity Modifiable (Major) Socioeconomic Class Obesity Physical Inactivity Smoking Alcohol Hypertension Previous Stroke/TIA Atherosclerosis Atrial Fibrillation Structural cardiac abnormalities Diabetes Modifiable (Minor) Diet Recreational Drug Use Sleep disordered breathing Thrombophilia Inflammation & Infection Migraine HRT Slide 17 Table Male sex Genetic Predisposition 1 – Risk Factors for Stroke. Markus et al, 2010
Risk Factors for Stroke n Non-modifiable Risk Factors - Helps identify those at greatest risk - Thereby enabling active treatment of those risk factors that can be modified in these patients Slide 18
Non-Modifiable risk factors • Age – most powerful independent risk factor • Gender – male higher risk • Family history - increased risk if a first-degree relative has had coronary heart disease or stroke before the age of 55 years (for a male relative) or 65 years (for a female relative). • Ethic group Slide 19
Modifiable risk factors • High blood pressure • Being over weight • Excessive alcohol • Smoking • Poor diet • High cholesterol • Lack of physical activity Slide 20
Atrial Fibrillation AF is the most common cause of cardio embolic stroke - Risk of stroke in people with AF is 5 -6 X greater than those in sinus rhythm - Paroxysmal AF has the same stroke risk as persistent AF and therefore should be treated the same Slide 21
Secondary prevention • Active management of modifiable risk factors • Carotid endarectomy • Pharmacological - concordance and compliance • Life style advice given to all (including information on driving & sex) • Blood pressure target • Cholesterol target 1 Slide 22
Stroke secondary prevention trials • • • Progress (BP lowering trial with ACE) Match (aspirin + clop) Caprie (clop v aspirin) Sparcl (atorvastatin) Blood Pressure Lowering Treatment Trialists’ Collaboration • Cochrane reviews Slide 23
Medication in practice • Anti platelet / anticoagulant - Clopidogrel, Warfarin, NOAC • Statin – Atorvastatin, • Anti hypertensive treatment –ACE , • Life long • (NICE 2008 RCP 2012) Slide 24
PCCS TIA Service • Follow on support to TIA Patient's diagnosed by NUH fast track service • Offered full health assessment, symptom and medication advise. • Support with lifestyle changes to reduce risk of TIA/Stroke • Access to phase 3 exercise programme • Access to cardiac team OT and councillor • Refer through SPAR Slide 25

Nottingham City. Care Partnership CIC 1 Standard Court Park Row Nottingham NG 1 6 GN e: citycare@nottinghamcitycare. nhs. uk t : 0115 883 9600 www. nottinghamcitycare. nhs. uk
- Slides: 26