The Use of Anencephalic Neonates as Organ Donors
- Slides: 14
The Use of Anencephalic Neonates as Organ Donors JAMA 1995 James G. Anderson, Ph. D. Professor of Sociology Purdue University
Current Law Requires persons to be dead before organs may be removed for transplantation.
Shortage of Organs for Infants and Children • Each year 500 children need a heart, 500 children need a liver, 4 -500 children need a kidney in the U. S. • 30 -50% of children under 2 years die while waiting for a transplant • Overall 40 -70% children die while waiting for a transplant
Anencephaly • Each year in the US 2000 -3000 infants are born with only a brain stem that supports the bodies autonomic functions • These infants do not experience consciousness • The infantas have a short life span less than 50% survive one day or more less than 10% survive more than one week
Benefits of Parental Donation • Many children will be saved • Parents find psychological stress alleviated somewhat
Objections • • • Prohibition against removal from living persons Inaccuracy of diagnosis Slippery slope concerns Few useable organs are obtained Public trust will be reduced in the organ procurement system
AMA Opinion It is ethically permissible to use anencephalic neonates as organ donors if: • The diagnosis is certain and is confirmed by two persons with special expertise. • The parents of the neonate initiate any discussion about organ donation and indicate their desire in writing. • There is compliance with the Council’s Guidelines for the Transplantation of Organs
Case A • While Theresa Ann Campo Pearson was in the womb, the tube around her embryonic central nervous system failed to close at one end. Consequently, she never developed a brain. When her parents learned at the eighth month of pregnancy that their baby would die within days of birth, they petitioned the Florida courts to declare Theresa brain dead. If Theresa’s organs could be taken while her brain stem kept her heart and lungs functioning, her parents could offer her kidneys, lungs, liver and heart to infants awaiting transplants.
Questions • Should Theresa’s parents request be granted since most infants needing a transplant will die before one becomes available? • If the courts rule in favor of the parents’ request, will this allow some good to come from this tragedy”? • Would granting the parents’ request result in the devaluation of human life where terminally ill patients will come to be viewed as collection of spare parts?
Question • Would declaring the baby brain dead in order to take her organs amount to killing a dying baby so that its organs could be used by someone else? • Should there be an exception to the “brain death” rule in the case of anencephalic neonates?
Case B • Baby Gabrielle was born in London, Ontario without most of her brain. In a radical departure from routine medical practice, the infant was placed on a respirator so that her heart could be salvaged for a transplant operation. Gabrielle’s parents stated that “They wanted to see that their baby would touch others and contribute to life in some way. ” The baby, while still connected to a respirator, was flown to California. After 48 hours, doctors turned off the respirator every 6 hours to test her breathing. When it was determined that Gabrielle could no longer breathe without the respirator, she was declared legally brain dead. Her heart was transplanted into a newborn boy.
Questions • Did placing Gabrielle on a respirator prolong her life and suffering beyond normal expectations? • Was it ethical to keep baby Gabrielle alive just for the purpose of preserving her organs for transplantation? • Does this case establish a precedent whereby the life of other terminally ill patients could be prolonged in order to preserve their organs for donation to others?
Case C • Ms. F, a woman in 32 nd week of her pregnancy, is seen by her physician for a routine prenatal exam. During the exam, it is noted that the fetus’s growth is less than expected and the patient is sent for an ultrasound exam. . The ultrasound shows that the fetus’s head is grossly malformed consistent with the diagnosis of anencephaly. Ms. F’s physician explains that, if born alive, the child will die within days. There are three choices: abortion, continuing the pregnancy and allowing the child to die, or continuing the pregnancy with the hope of donating the child’s organs. Ms. F chooses the third option. At 38 weeks there is decreased fetal movement, a sign that the fetus may be dying. Ms. F requests a C-section so that the child’s organs could be used for transplantation.
Questions • Should her physician accede to Ms. F’s request? • Are the risks to Ms. F of a cesarean section justified in this case?
 Warm chain
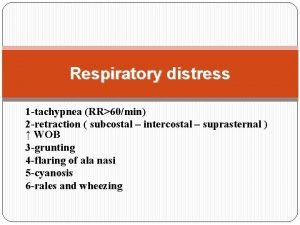
Warm chain Tachypnea causes
Tachypnea causes Grading of jaundice in neonates
Grading of jaundice in neonates Normal cbc in neonates
Normal cbc in neonates Kjs_1999
Kjs_1999 High risk neonates definition
High risk neonates definition Mechanisms of heat loss in newborn
Mechanisms of heat loss in newborn Neonatal energy triangle
Neonatal energy triangle Bhutani nomogram
Bhutani nomogram Organ and organ system
Organ and organ system Cell tissue organ organ system organism
Cell tissue organ organ system organism Organ organ pernafasan
Organ organ pernafasan Tissue are grouped together to form various
Tissue are grouped together to form various Penyusun sistem saraf pusat adalah
Penyusun sistem saraf pusat adalah Organ penyususn sistem gerak pada manusia adalah
Organ penyususn sistem gerak pada manusia adalah