The role of Intensive Home Treatment for Maternal



- Slides: 15
The role of Intensive Home Treatment for Maternal Mental Illness Dr Colin Crawford Consultant Psychiatrist & Fiona Smith Senior Charge Nurse Both work for Perinatal service and IHTT
Karen age 34 First pregnancy planned twin pregnancy Difficult pregnancy Swine flu at 30 weeks Babies born at 33 weeks by Caesarian Section Onset of Postpartum Psychosis at day 3 Suicidal ideation tried to jump of second floor window of maternity unit • Admitted to Mother and Baby unit for prolonged period • On discharge followed by CMHT • • •

Most recent pregnancy Unplanned Pregnancy single pregnancy Discontinued Imipramine 50 mgs Referred to the perinatal service Seen early in pregnancy and reviewed regularly Well but some anxiety about becoming unwell following childbirth • Perinatal Management Plan developed and Pre birth planning meeting held • Olanzapine 5 mgs provided to her to bring to labour ward • • •
Baby born on due date • • 3 rd degree tear Breast feeding Seen daily by the perinatal team in post natal ward Day 2 not well with predominant “racing thoughts” and anxiety Started Olanzapine 5 mgs Day 3 keen to get home with husband did not want hospital admission husband happy to support going home Risks assessed taken on by IHTT with review where possible with IHTT perinatal team members Initially Twice daily visits
Progress • Seen by IHTT for a total of 10 weeks • Initially daily and gradually less frequently • Medication changed and at time of discharge was on Olanzapine 10 mgs and Imipramine 150 mgs • Had used Diazepam 2 mgs p. r. n. • Continued to breast feed and baby thrived • Liaison with CPN, HV, GP

What Made It Possible? Good home support Patient keen for a different experience Patient had better understanding of symptoms Regular risk assessment at every visit 24 hour phone contact Regular medical review and adjustment of medication • Good pre-birth planning • Knowing that Mother and Baby unit an option • • •
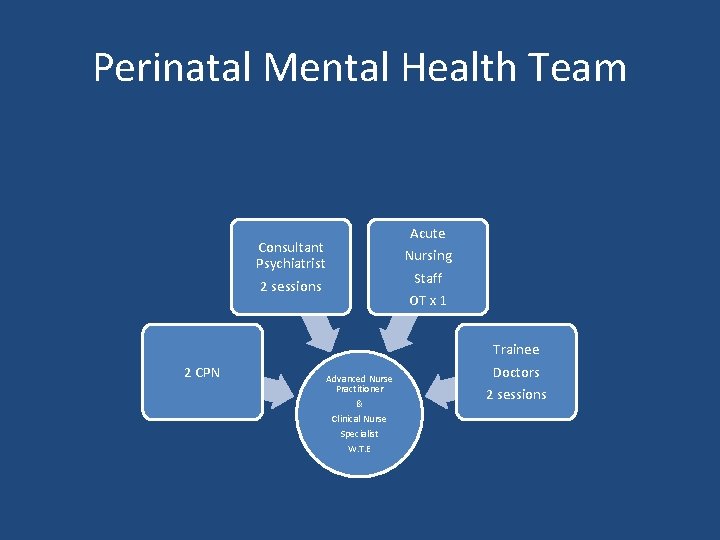
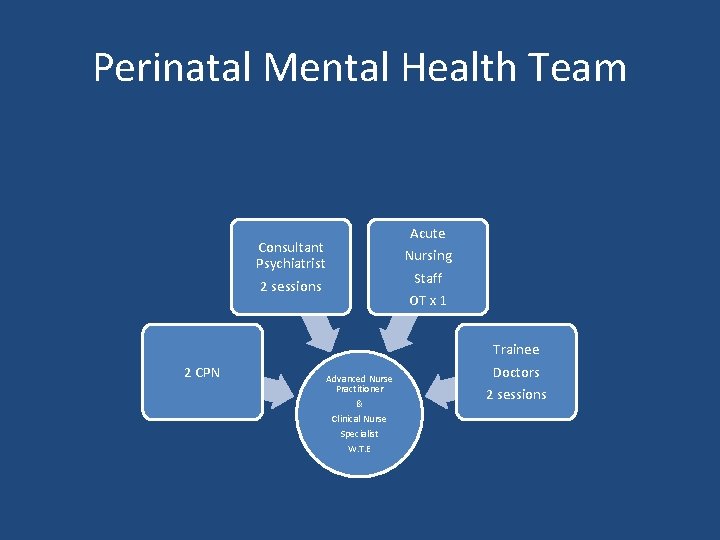
Perinatal Mental Health Team Acute Nursing Staff Consultant Psychiatrist 2 sessions 2 CPN OT x 1 Advanced Nurse Practitioner & Clinical Nurse Specialist W. T. E Trainee Doctors 2 sessions
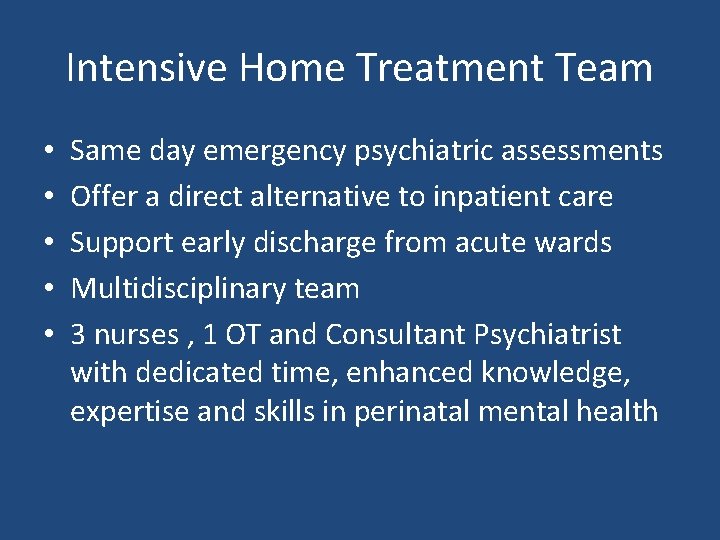
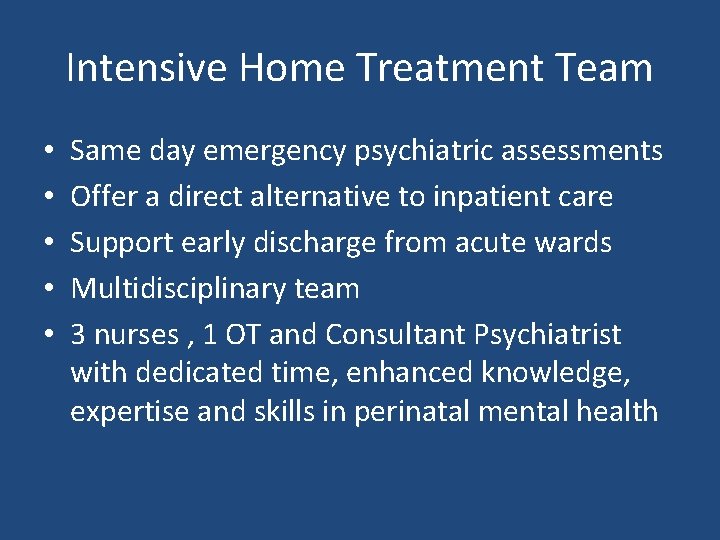
Intensive Home Treatment Team • • • Same day emergency psychiatric assessments Offer a direct alternative to inpatient care Support early discharge from acute wards Multidisciplinary team 3 nurses , 1 OT and Consultant Psychiatrist with dedicated time, enhanced knowledge, expertise and skills in perinatal mental health
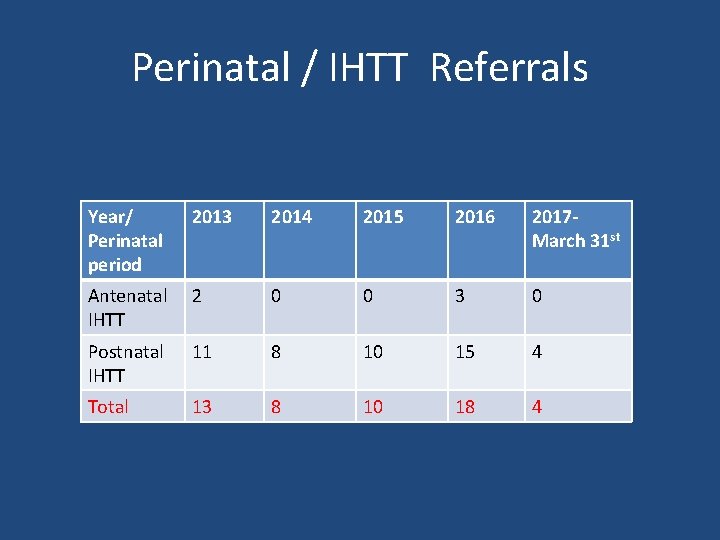
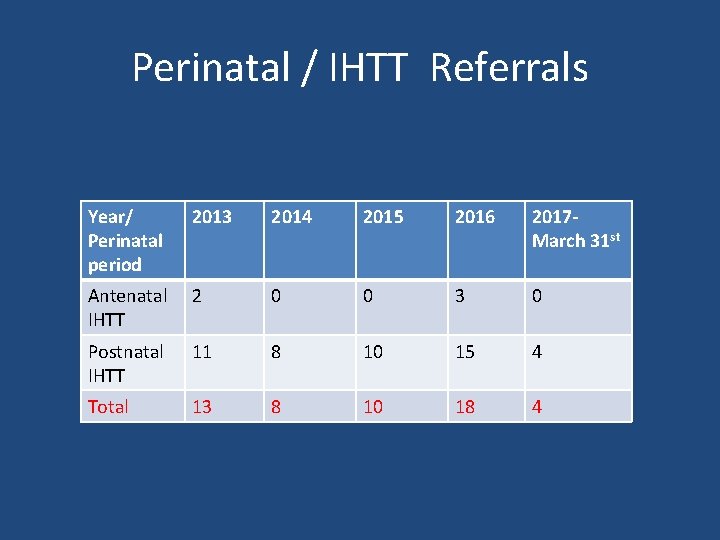
Perinatal / IHTT Referrals Year/ Perinatal period 2013 2014 2015 2016 2017 March 31 st Antenatal IHTT 2 0 0 3 0 Postnatal IHTT 11 8 10 15 4 Total 13 8 10 18 4
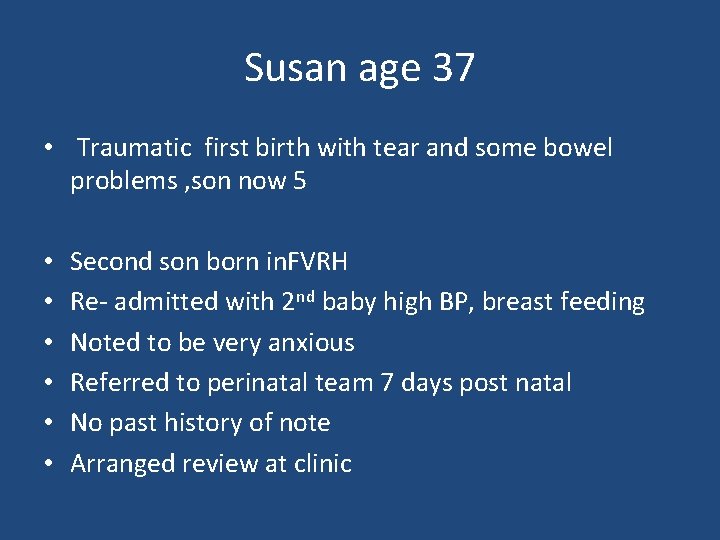
Susan age 37 • Traumatic first birth with tear and some bowel problems , son now 5 • • • Second son born in. FVRH Re- admitted with 2 nd baby high BP, breast feeding Noted to be very anxious Referred to perinatal team 7 days post natal No past history of note Arranged review at clinic
Cont • Seen at perinatal clinic still anxious about physical health prescribed Paroxetine 20 mgs. • Referred IHTT at 8 weeks anxious about health but also delusions of reference and auditory hallucinations • Husband very anxious and not coping making home treatment unsustainable • Admitted to Mother and baby unit
Referred back to IHTT • One month admission to M and B • Prescribed Olanzapine 5 mgs b. d. and continued Paroxetine • Much improved but husband in particular still very anxious • One month input by IHTT • Followed up by Perinatal service till baby just over a year old and had been able to come off all medication
What Made it Not Possible • Home Treatment not possible for all the treatment. • Carer strain when symptoms became clearly psychotic • Symptom escalation prior to admission to M and B unit • No risks of self harm or harm to baby • No past psychiatric symptoms or significant personal history
Summary Need good reliable home support Need integration of IHTT and Perinatal service Regular risk assessment essential 24 hour back up support helpful Good for step down from Mother and Baby unit • Working with experienced Perinatal clinicians helps build confidence • • •

Any questions?
 Maternal effect and maternal inheritance
Maternal effect and maternal inheritance Maternal effect and maternal inheritance
Maternal effect and maternal inheritance Ramona t mercer theory
Ramona t mercer theory Intensive phase of tb treatment
Intensive phase of tb treatment Rollenmodell
Rollenmodell Role conflict occurs when fulfilling the role expectations
Role conflict occurs when fulfilling the role expectations Azure web role worker role example
Azure web role worker role example Perbedaan home care dan home visit
Perbedaan home care dan home visit Oak springs mobile home park
Oak springs mobile home park Homes for sale in roebuck sc
Homes for sale in roebuck sc Let's go to my house let's go today
Let's go to my house let's go today Unit 1 home sweet home
Unit 1 home sweet home She said that, home economics stands for the ideal home.
She said that, home economics stands for the ideal home. John heartfield
John heartfield Pengertian homecare
Pengertian homecare Softly and tenderly jesus is calling
Softly and tenderly jesus is calling