Telehealth The Cornwall Experience Dave Tyas Telehealth and
- Slides: 19
Telehealth: The Cornwall Experience Dave Tyas Telehealth and Service Improvement Manager
What am I going to talk about today? • Telehealth in Cornwall – current position • How we got there – the process, the structure and the challenges • Patient and Clinical Experience • Next Steps in Cornwall
Telehealth – a work in progress…… • Started in 2009 as part of WSD • Mainstreamed in April 2010 with recurrent funding Now • 1000 people installed • 650 actively being monitored • Conditions covered: Diabetes, CHF, COPD, Stroke, Falls Risk, UTI • Referrals from Acute, Community and Primary Care Future • Expand service to over 1000 active users by end of the financial year • Individual systems in peoples homes and multi-user systems for residential / nursing care • Develop the service with other conditions / circumstances
How we got there……. WSD Timeline 2008 • Formation of the WSD project team including management, clinicians, programme support staff and field teams • Engagement with GP’s to sign up practices (45 signed up) • Procurement of Telehealth equipment from Tunstall 2009 • Commenced installations (Feb) • Refined processes and established team • Data collection for evaluation 2010 • Completed WSD installations • Service mainstreamed and opened up to other conditions
How we got there……. Team Structure Central service monitoring 80% of the patients: • Service operations lead • Senior Telehealth Nurse • 3. 5 x Telehealth Nurses • 3 x Patient Support Operators • 2 x Engineers • 2 x Assistant Practitioners =12 FTE 20% monitoring covered by community matrons and specialist nurse teams
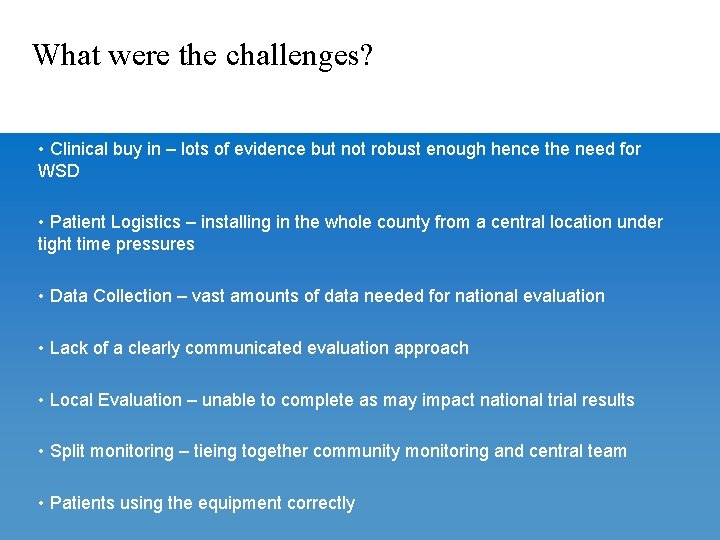
What were the challenges? • Clinical buy in – lots of evidence but not robust enough hence the need for WSD • Patient Logistics – installing in the whole county from a central location under tight time pressures • Data Collection – vast amounts of data needed for national evaluation • Lack of a clearly communicated evaluation approach • Local Evaluation – unable to complete as may impact national trial results • Split monitoring – tieing together community monitoring and central team • Patients using the equipment correctly
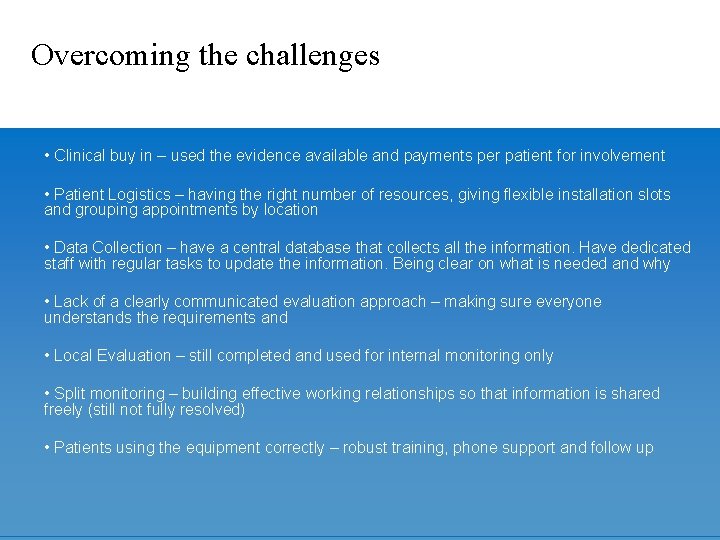
Overcoming the challenges • Clinical buy in – used the evidence available and payments per patient for involvement • Patient Logistics – having the right number of resources, giving flexible installation slots and grouping appointments by location • Data Collection – have a central database that collects all the information. Have dedicated staff with regular tasks to update the information. Being clear on what is needed and why • Lack of a clearly communicated evaluation approach – making sure everyone understands the requirements and • Local Evaluation – still completed and used for internal monitoring only • Split monitoring – building effective working relationships so that information is shared freely (still not fully resolved) • Patients using the equipment correctly – robust training, phone support and follow up
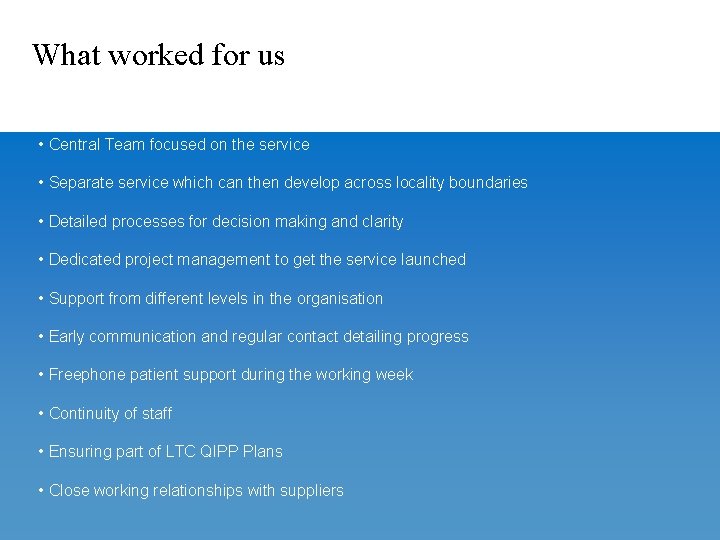
What worked for us • Central Team focused on the service • Separate service which can then develop across locality boundaries • Detailed processes for decision making and clarity • Dedicated project management to get the service launched • Support from different levels in the organisation • Early communication and regular contact detailing progress • Freephone patient support during the working week • Continuity of staff • Ensuring part of LTC QIPP Plans • Close working relationships with suppliers
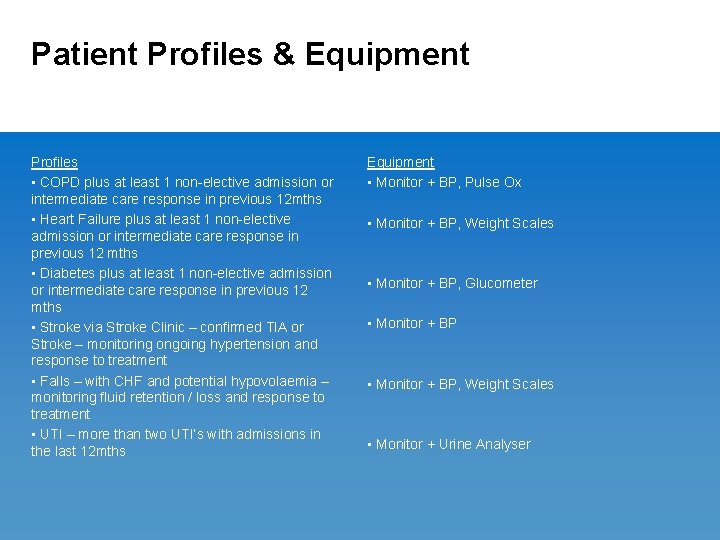
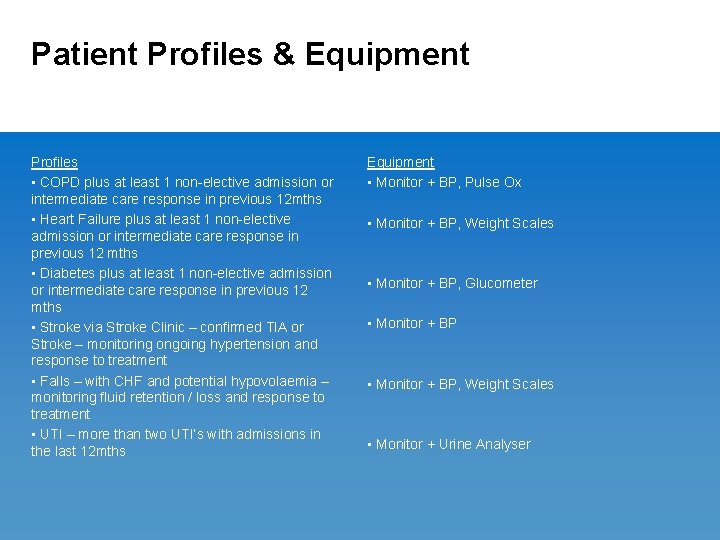
Patient Profiles & Equipment Profiles • COPD plus at least 1 non-elective admission or intermediate care response in previous 12 mths • Heart Failure plus at least 1 non-elective admission or intermediate care response in previous 12 mths • Diabetes plus at least 1 non-elective admission or intermediate care response in previous 12 mths • Stroke via Stroke Clinic – confirmed TIA or Stroke – monitoring ongoing hypertension and response to treatment • Falls – with CHF and potential hypovolaemia – monitoring fluid retention / loss and response to treatment • UTI – more than two UTI’s with admissions in the last 12 mths Equipment • Monitor + BP, Pulse Ox • Monitor + BP, Weight Scales • Monitor + BP, Glucometer • Monitor + BP, Weight Scales • Monitor + Urine Analyser
Monitoring Process • Non-transmissions and technical issues monitored by PSO • Clinical monitoring completed 9 -5 – focus on developing trends • Intervention ranges from telephone triage to emergency referral • Education and support is provided as part of day to day contact • Onus is on the patient to act the majority of the time – clinical feedback / info provided to primary/secondary care clinicians
Who benefits from Telehealth? 3 types of people: 1. Not interested in home monitoring – reliant on utilising care when they become ill / symptomatic 2. Interested in home monitoring but need the constant support of a clinician 3. Interested in home monitoring and utilising the information to Self Care! Focus on types 2 and 3 but consider how to convert type 1!
Clinical Experience Positive for some, mixed for others: Plus points • Impact on capacity – it has the potential to save visits in remote locations • Supports clinical care and management – getting to know patients biometrics which often signify and exacerbation. • Enhances patient independence and empowerment – empowers patients and helps to get them motivated about managing their own conditions with visual evidence Requirements • Only works if the patient is engaged and wants to manage their own condition • Care management systems need to adapt to imbed the technology – clinicians need to commit to making it work • Technology on its own will not have the necessary impact Clinical engagement will only be effective with the required evidence!
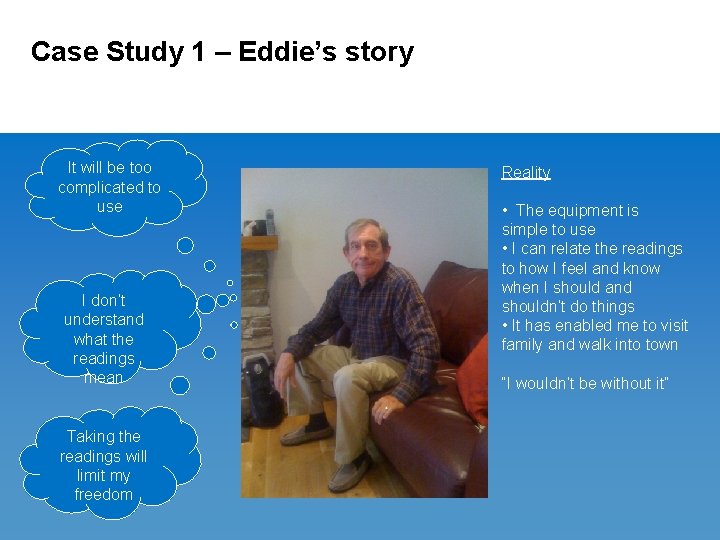
Case Study 1 – Eddie’s story It will be too complicated to use I don’t understand what the readings mean Taking the readings will limit my freedom Reality • The equipment is simple to use • I can relate the readings to how I feel and know when I should and shouldn’t do things • It has enabled me to visit family and walk into town “I wouldn’t be without it”
Case Study 2 – Changing Perception 66 yr old male – COPD Keyworker – Julie Coles RSN – feedback as follows: Problems: Early detection of exacerbation a problem Person not wanting home oxygen Action taken: Short Burst Oxygen Therapy instigated Early detection of exacerbation – antibiotic therapy Outcome: Has successfully reduced admissions Person more aware of early signs of exacerbation
Case Study 3 – Branching out and working with carers • • 78 year old user suffering from Dementia with husband as carer – had emergency meds in the home User symptomatic of UTI detected by follow up to question set - complained around lunchtime that she was experiencing a burning sensation and a strong urine odour Husband decided to test her urine and then called the results into the Telehealth nurse team The results came back as positive for early onset of UTI The husband started his wife on emergency meds He expressed his relief that he could now do something about it - his comments were that if he tried to make an appointment with his GP he would be unlikely to get one until Monday and that this would be too late. In addition taking a urine sample now would not then be processed until after the weekend Follow up with user – symptoms eased over the weekend following intake of meds • Previous experience from discussion with carer – would have resulted in admission • • •
Benefits to Patients • • • Visual impact of seeing biometrics – giving up smoking, losing weight Early diagnosis of problems – irregular heart beat, postural blood pressure drop, high blood pressure Diagnosis of serious illness – diabetic ketoacidosis, low blood oxygen levels Overall, quality of life effects have been amazing! • “It gives me peace of mind to know my daily readings. If they vary significantly it gives an opportunity to review recent lifestyle changes and consider their effect” • “To start with I wasn’t sure about the equipment and couldn’t see how it could help me now I wouldn’t want to be without it – it’s a good lifeline” • “I now have a better idea of when to adjust and increase my medication to combat symptoms. Before Telehealth I tended to leave it too late thinking I would get better and sometimes I would be taken to hospital”
The collective view – not just individuals…. . • Survey May 2011 – 500 Cornwall Telehealth users • 54% response rate • 90% users got some benefit from utilising Telehealth • 89% felt that the equipment was easy to use • 78% felt that the equipment helped them to manage their condition and that they got a benefit from clinical monitoring Keywords: “Anxiety reduction, independence, security”
Next Steps in Cornwall • Expansion of service throughout community, acute and primary care • 12 mth trial of RISC tool for Telehealth patient selection • Installation of multi-user Telehealth systems in care homes and remote locations (Isles of Scilly) • Investigation into early discharge and step down from acute care at home • Referrals from health and social care hubs
Any Questions?
 Veryan work experience
Veryan work experience Tyas ayu sex
Tyas ayu sex Nicola tyas
Nicola tyas Rumus kadar air
Rumus kadar air Nicola tyas sex
Nicola tyas sex Telehealth and telemedicine
Telehealth and telemedicine Telenursing and remote access telehealth
Telenursing and remote access telehealth Ctel telehealth
Ctel telehealth Office for the advancement of telehealth
Office for the advancement of telehealth Flo telehealth
Flo telehealth Indirect experience
Indirect experience Experience expectant vs experience dependent
Experience expectant vs experience dependent Continuity vs discontinuity
Continuity vs discontinuity Henry, duke of cornwall
Henry, duke of cornwall Susannah cornwall
Susannah cornwall Criminal record
Criminal record Satellite broadband cornwall
Satellite broadband cornwall Mundic block test cornwall
Mundic block test cornwall Linda cornwall
Linda cornwall Inclusion cornwall
Inclusion cornwall