IMPROVING HEALTH ACCESS THROUGH TELEHEALTH TELEHEALTH THE RURAL

- Slides: 10
IMPROVING HEALTH ACCESS THROUGH TELEHEALTH: TELEHEALTH THE RURAL CALIFORNIA EXPERIENCE Presented by Mario Gutierrez October 13, 2010
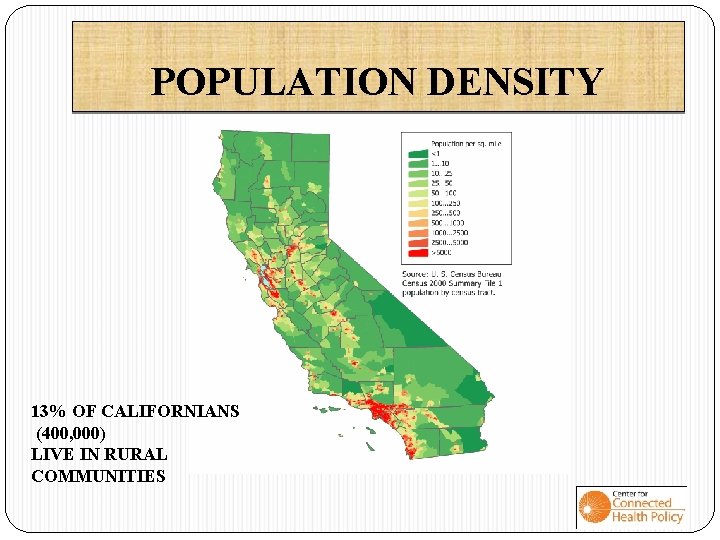
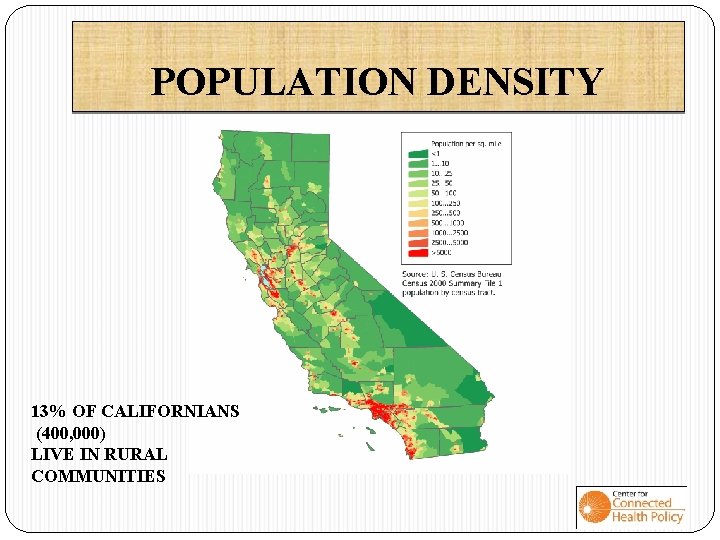
POPULATION DENSITY 13% OF CALIFORNIANS (400, 000) LIVE IN RURAL COMMUNITIES
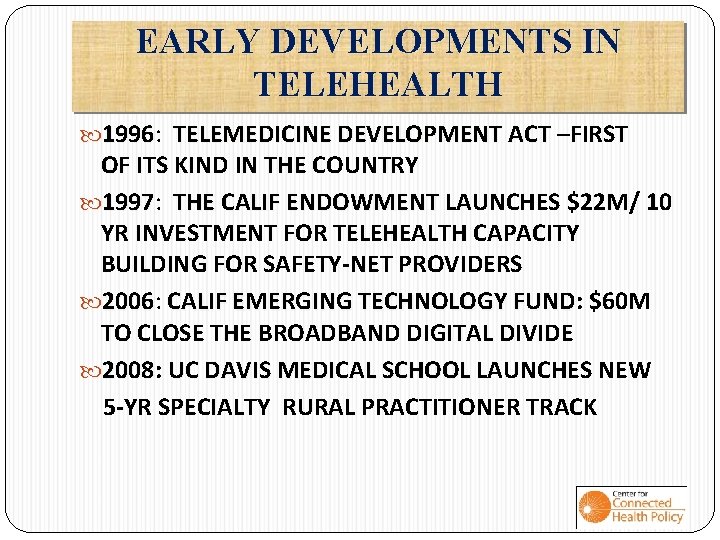
EARLY DEVELOPMENTS IN TELEHEALTH 1996: 1996 TELEMEDICINE DEVELOPMENT ACT –FIRST OF ITS KIND IN THE COUNTRY 1997: 1997 THE CALIF ENDOWMENT LAUNCHES $22 M/ 10 YR INVESTMENT FOR TELEHEALTH CAPACITY BUILDING FOR SAFETY-NET PROVIDERS 2006: 2006 CALIF EMERGING TECHNOLOGY FUND: FUND $60 M TO CLOSE THE BROADBAND DIGITAL DIVIDE 2008: 2008 UC DAVIS MEDICAL SCHOOL LAUNCHES NEW 5 -YR SPECIALTY RURAL PRACTITIONER TRACK
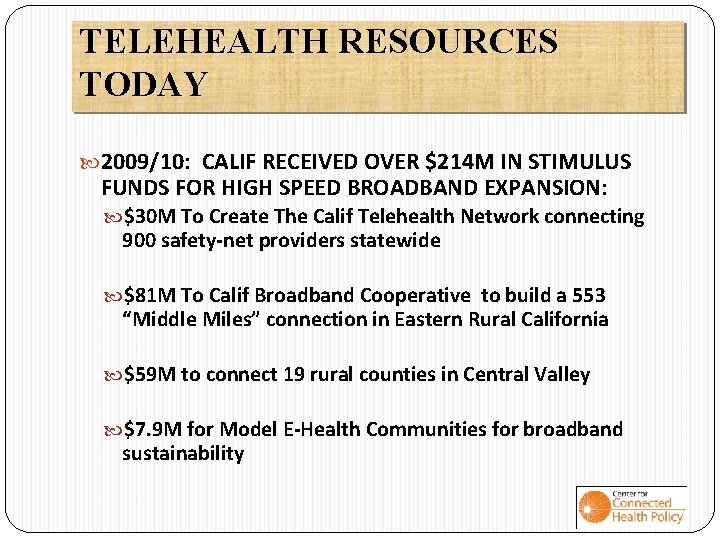
TELEHEALTH RESOURCES TODAY 2009/10: 2009/10 CALIF RECEIVED OVER $214 M IN STIMULUS FUNDS FOR HIGH SPEED BROADBAND EXPANSION: $30 M To Create The Calif Telehealth Network connecting 900 safety-net providers statewide $81 M To Calif Broadband Cooperative to build a 553 “Middle Miles” connection in Eastern Rural California $59 M to connect 19 rural counties in Central Valley $7. 9 M for Model E-Health Communities for broadband sustainability

CENTER FOR CONNECTED HEALTH POLICY • Supported by: The California Health Care Foundation • Projects Include: • Specialty Care Safety Net Initiative • Model Telehealth Statute Development • Telederm Utilization Research
SPECIALTY CARE SAFETY NET INITIATIVE Policy, statutory, and practice pattern barriers prevent UC Schools of Medicine from providing specialty care consults to safety net patients. Identifying and removing these barriers is essential to the long-term sustainability of UC based telehealth projects serving safety net patients. Three year project running through early 2012 Up to $1 million to 5 UC campuses Up to $1 million to 45 community health centers Vigorous assessment of challenges and benefits
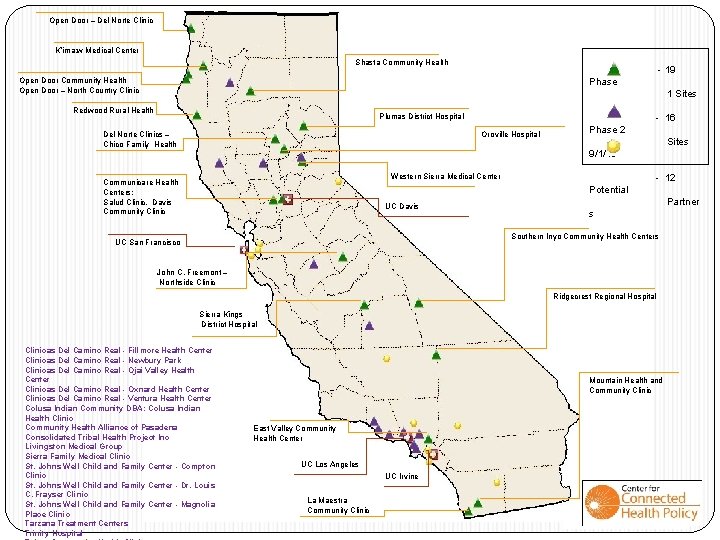
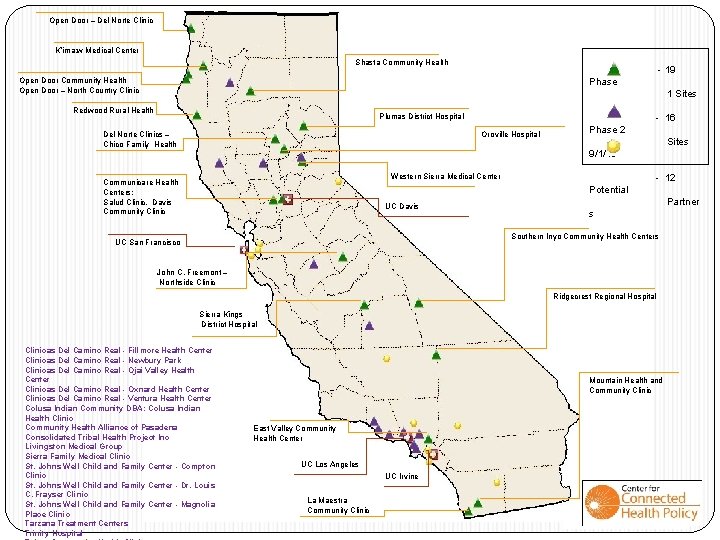
Open Door – Del Norte Clinic K’ima: w Medical Center Shasta Community Health - 19 Open Door Community Health Open Door – North Country Clinic Phase 1 Sites Redwood Rural Health Plumas District Hospital Del Norte Clinics – Chico Family Health - 16 Oroville Hospital Phase 2 Sites 9/1/10 Western Sierra Medical Center Communicare Health Centers: Salud Clinic, Davis Community Clinic - 12 Potential UC Davis Partner s Southern Inyo Community Health Centers UC San Francisco John C. Freemont – Northside Clinic Ridgecrest Regional Hospital Sierra Kings District Hospital Clinicas Del Camino Real - Fillmore Health Center Clinicas Del Camino Real - Newbury Park Clinicas Del Camino Real - Ojai Valley Health Center Clinicas Del Camino Real - Oxnard Health Center Clinicas Del Camino Real - Ventura Health Center Colusa Indian Community DBA: Colusa Indian Health Clinic Community Health Alliance of Pasadena Consolidated Tribal Health Project Inc Livingston Medical Group Sierra Family Medical Clinic St. Johns Well Child and Family Center - Compton Clinic St. Johns Well Child and Family Center - Dr. Louis C. Frayser Clinic St. Johns Well Child and Family Center - Magnolia Place Clinic Tarzana Treatment Centers Trinity Hospital Mountain Health and Community Clinic East Valley Community Health Center UC Los Angeles UC Irvine La Maestra Community Clinic
MODEL STATUTE DEVELOPMENT POLICY GOALS: Update the 1996 CA Telemedicine development Act Provide national leadership in the use of telehealth tools to re-shape health care into patient-centered, accountable, and efficient system Provide a framework for new legislation/regulatory change to advance the use and reimbursement of telehealth services Identify related state and federal policy/practice barriers that inhibit full application of telehealth
CHALLENGES MOVING FORWARD: State: Massive State annual budget deficits New Governor and legislative leaders Federal Level: Need fresh thinking to stimulate innovation and reimbursement policies for Medicaid and Medicare (CMS Center for Innovation) Interstate Licensure & Scope of Practice Policy Review Health Systems: Change comes slowly-rural practices need to behave differently. . Too Much Too Fast! HIE-EMR-TELEHEALTH need to be in synch for systems to function efficiently
TELEHEALTH BENEFITS FOR RURAL Strengthens Safety-Net as Patient-Centered Medical Home E-visits, continuity of care, chronic care management Gives Rural Hospitals New Life: e. ICU, LTC Workforce: Improves recruitment and CME access Public Health Home health care monitoring Emergency Disaster Preparation Monitoring Disparities Building Healthy Communities! Access to prevention & education information One E-application for all health social benefits Enhances overall quality of life-A life-line to the World