Salford Integrated Care Programme Salfords approach to integrated





- Slides: 31

Salford Integrated Care Programme Salford’s approach to integrated care for older people - work in progress Updated 13 December 2012
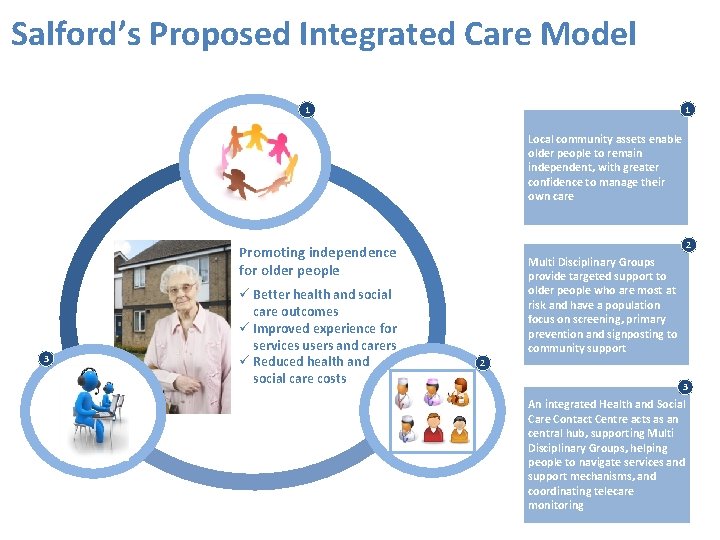
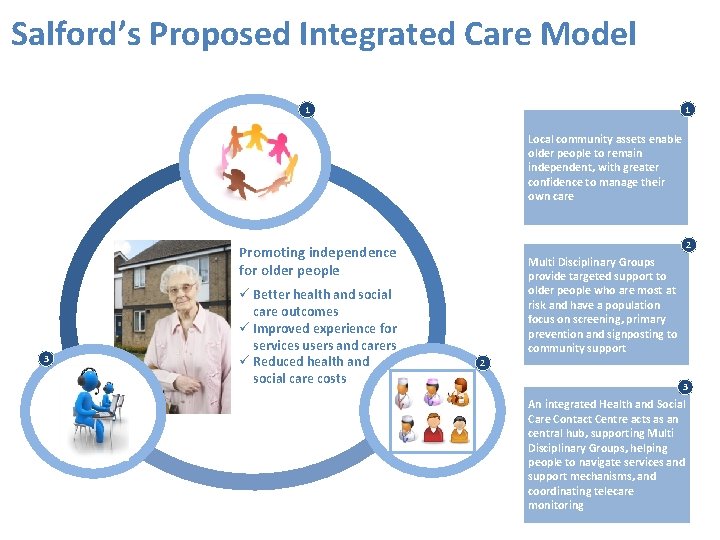
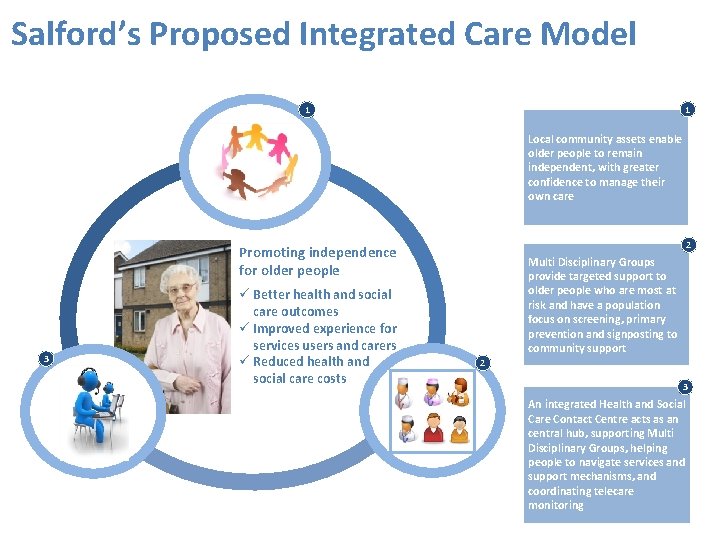
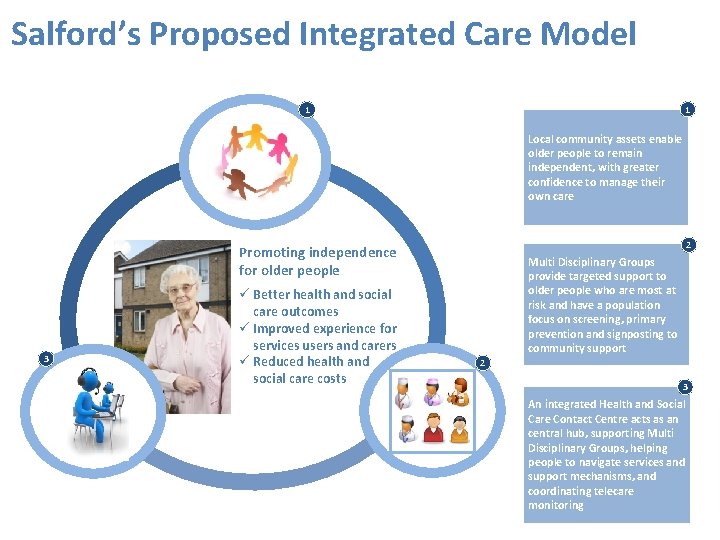
Salford’s Proposed Integrated Care Model 1 1 Local community assets enable older people to remain independent, with greater confidence to manage their own care 2 Promoting independence for older people 3 Better health and social care outcomes Improved experience for services users and carers Reduced health and social care costs Multi Disciplinary Groups provide targeted support to older people who are most at risk and have a population focus on screening, primary prevention and signposting to community support 2 3 An integrated Health and Social Care Contact Centre acts as an central hub, supporting Multi Disciplinary Groups, helping people to navigate services and support mechanisms, and coordinating telecare monitoring
We need your input Feedback received from Scheduled for review ICP Integrated Care Board ICP Care Standards Reference Group ICP Information Subgroup ICP Comms, Engagement & HR Subgroup ICP Finance Subgroup Health & Wellbeing ICB District Nurse leads SCC Directorate Management Group CCG Informal Board SCC Public Health Senior Managers meeting • SRFT Salford Healthcare Board • SRFT Leaders Forum • SCC Managers Forum • • • • • • Telehealthcare Strategy Group Salford Health Matters SRFT Strategy Advisory Group Eccles Neighbourhood CCG meeting SCC Health Improvement Team Swinton Neighbourhood CCG meeting Care Homes Group Health & Wellbeing Board Third sector / CVS Salford & Trafford LMC GP Practice meetings

Salford’s Approach Promote independence for older people, delivering: 1. Better health and social care outcomes 2. Improved experience for services users and carers 3. Reduced health and social care costs 4
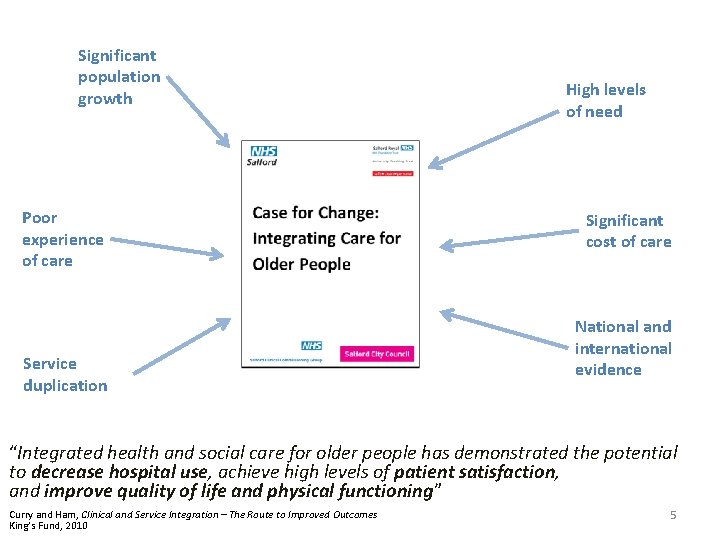
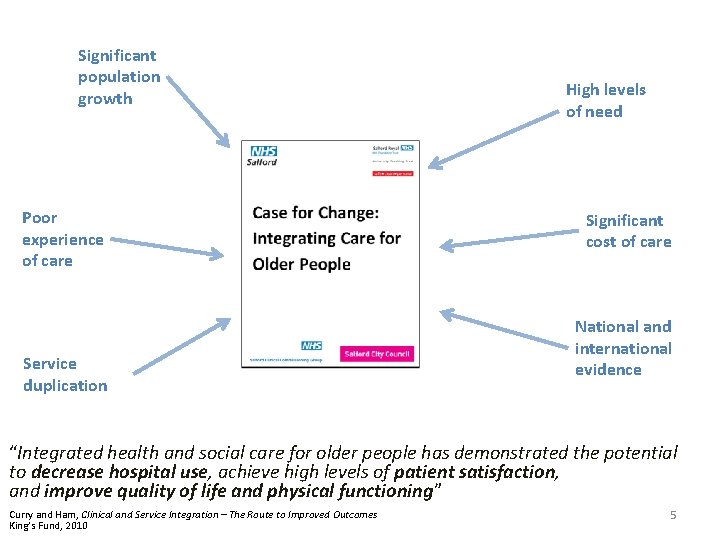
Significant population growth Poor experience of care Service duplication High levels of need Significant cost of care National and international evidence “Integrated health and social care for older people has demonstrated the potential to decrease hospital use, achieve high levels of patient satisfaction, and improve quality of life and physical functioning” Curry and Ham, Clinical and Service Integration – The Route to Improved Outcomes King’s Fund, 2010 5
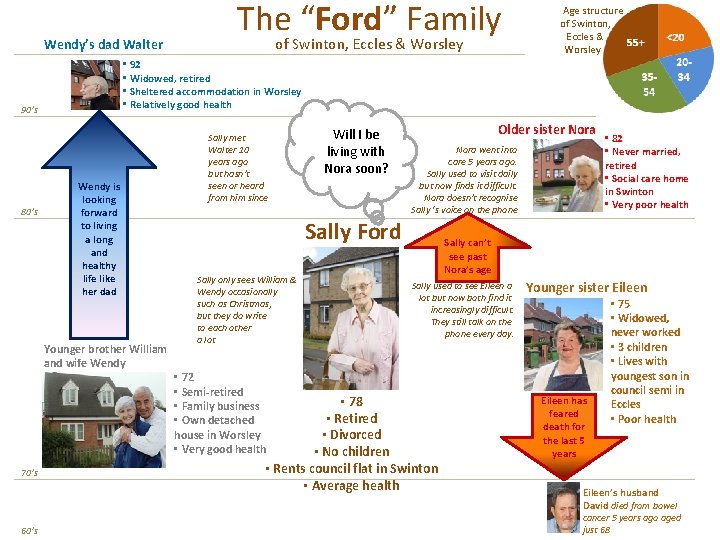
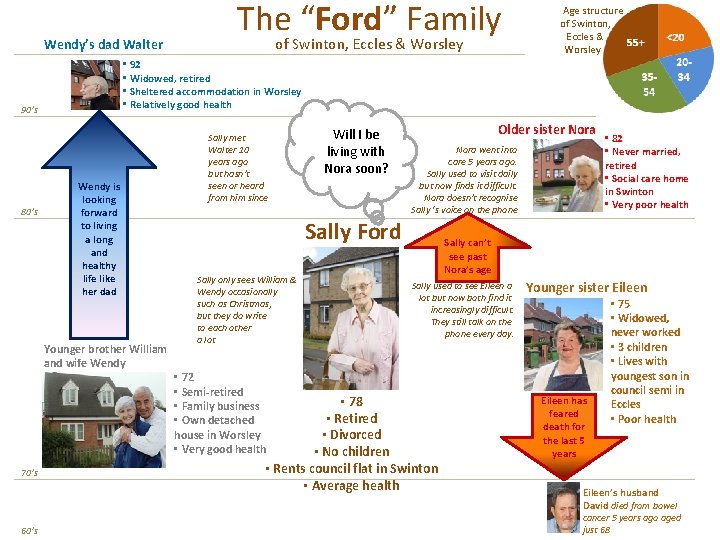
Wendy’s dad Walter Wendy is looking forward to living a long and healthy life like her dad Younger brother William and wife Wendy 70’s 60’s of Swinton, Eccles & Worsley • 92 • Widowed, retired • Sheltered accommodation in Worsley • Relatively good health 90’s 80’s The “Ford” Family Age structure of Swinton, Eccles & Worsley Sally met Walter 10 years ago but hasn’t seen or heard from him since Will I be living with Nora soon? Older sister Nora went into care 5 years ago. Sally used to visit daily but now finds it difficult. Nora doesn’t recognise Sally ‘s voice on the phone Sally Ford Sally only sees William & Wendy occasionally such as Christmas, but they do write to each other a lot • 72 • Semi-retired • Family business • Own detached house in Worsley • Very good health • 82 • Never married, retired • Social care home in Swinton • Very poor health Sally can’t see past Nora’s age Sally used to see Eileen a lot but now both find it increasingly difficult. They still talk on the phone every day. • 78 • Retired • Divorced • No children • Rents council flat in Swinton • Average health Younger sister Eileen has feared death for the last 5 years • 75 • Widowed, never worked • 3 children • Lives with youngest son in council semi in Eccles • Poor health Eileen’s husband David died from bowel cancer 5 years ago aged just 68
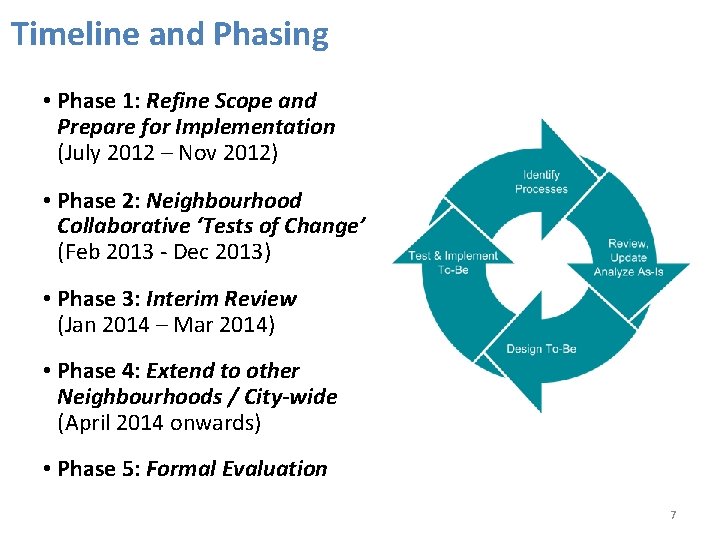
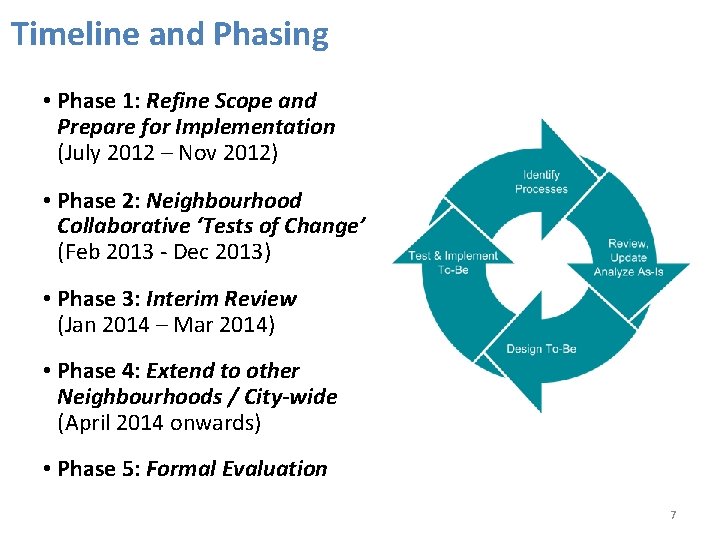
Timeline and Phasing • Phase 1: Refine Scope and Prepare for Implementation (July 2012 – Nov 2012) • Phase 2: Neighbourhood Collaborative ‘Tests of Change’ (Feb 2013 - Dec 2013) • Phase 3: Interim Review (Jan 2014 – Mar 2014) • Phase 4: Extend to other Neighbourhoods / City-wide (April 2014 onwards) • Phase 5: Formal Evaluation 7
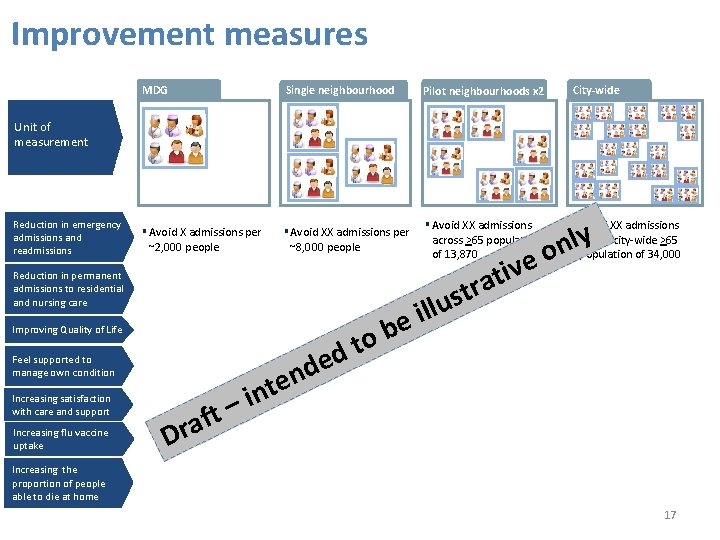
Our Improvement measures 1. Reducing emergency admissions and readmissions 2. Reducing permanent admissions to residential and nursing care 3. Improving Quality of Life for users and carers 4. Increasing the proportion of Older People that feel supported to manage own condition 5. Increasing satisfaction with the care and support provided to Older People 6. Increasing flu vaccine uptake for Older People 7. Increasing the proportion of Older People that die at home (or in their preferred place of dying) 8

Developing Salford’s model for integrated care
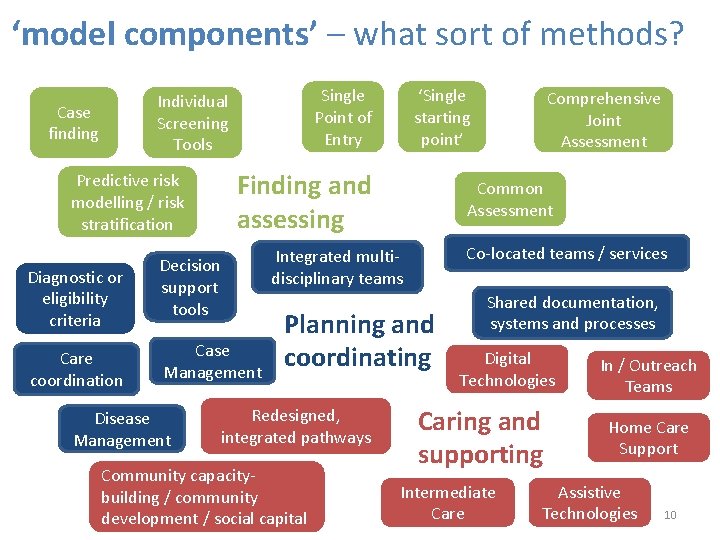
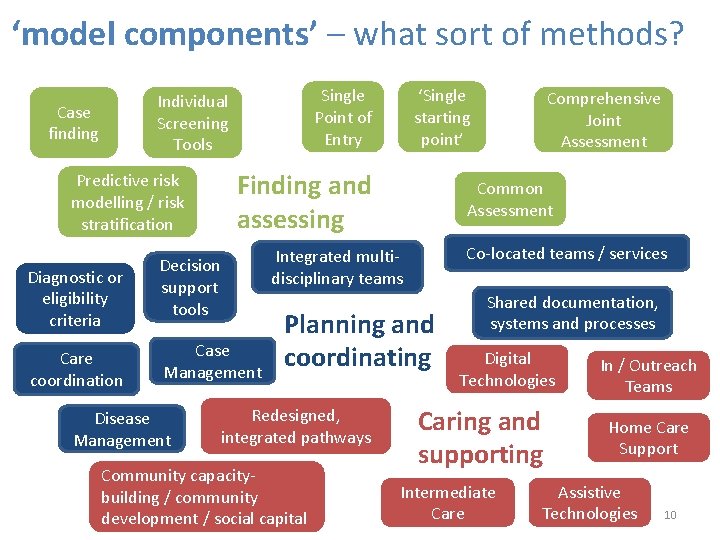
‘model components’ – what sort of methods? Single Point of Entry Individual Screening Tools Case finding Finding and assessing Predictive risk modelling / risk stratification Diagnostic or eligibility criteria Care coordination Decision support tools Case Management Disease Management ‘Single starting point’ Common Assessment Co-located teams / services Integrated multidisciplinary teams Planning and coordinating Redesigned, integrated pathways Community capacitybuilding / community development / social capital Comprehensive Joint Assessment Shared documentation, systems and processes Digital Technologies Caring and supporting Intermediate Care In / Outreach Teams Home Care Support Assistive Technologies 10
Top 10 priorities from Salford’s engagement • • • Integrate IT systems and care records Rationalise points of access (e. g. single contact centre, shared portal) Increased support for carers and to enable self-management Asset mapping (incl. use of neighbours, third sector, community signposting) Maintained Directory of Services for the public and professionals Extended / consistent hours (incl. 24/7 response) Engagement and communication with service users regarding change Care Coordinator / Key Workers to support people with complex needs Pooled budget / joint management for health and social care MDT / forum for supporting people with complex needs 11
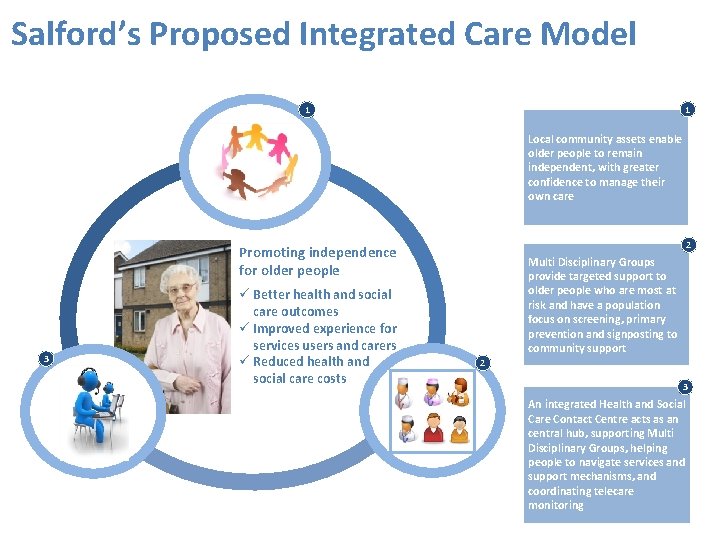
Salford’s Proposed Integrated Care Model 1 1 Local community assets enable older people to remain independent, with greater confidence to manage their own care 2 Promoting independence for older people 3 Better health and social care outcomes Improved experience for services users and carers Reduced health and social care costs Multi Disciplinary Groups provide targeted support to older people who are most at risk and have a population focus on screening, primary prevention and signposting to community support 2 3 An integrated Health and Social Care Contact Centre acts as an central hub, supporting Multi Disciplinary Groups, helping people to navigate services and support mechanisms, and coordinating telecare monitoring

Local Community Assets 2 1 Befriending Carer Support 3 10 Way to Wellbeing Local venues 4 9 Housing & Transport Local Employers 8 7 Volunteers Self Care 6 5 Telecare Community Groups 13
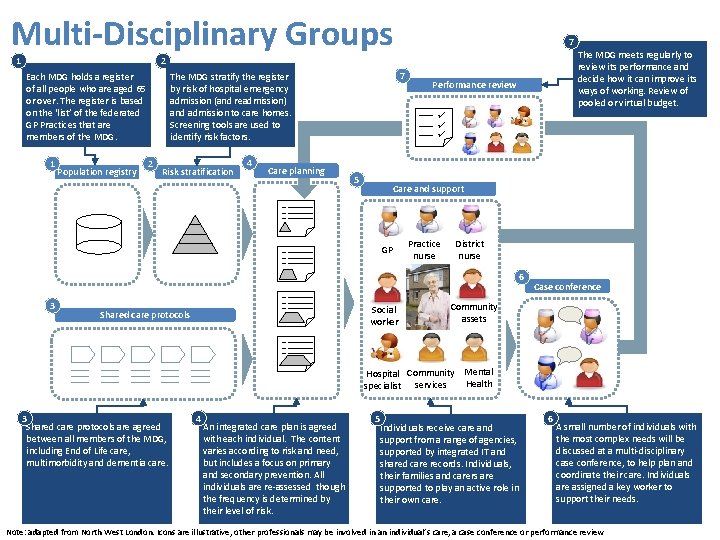
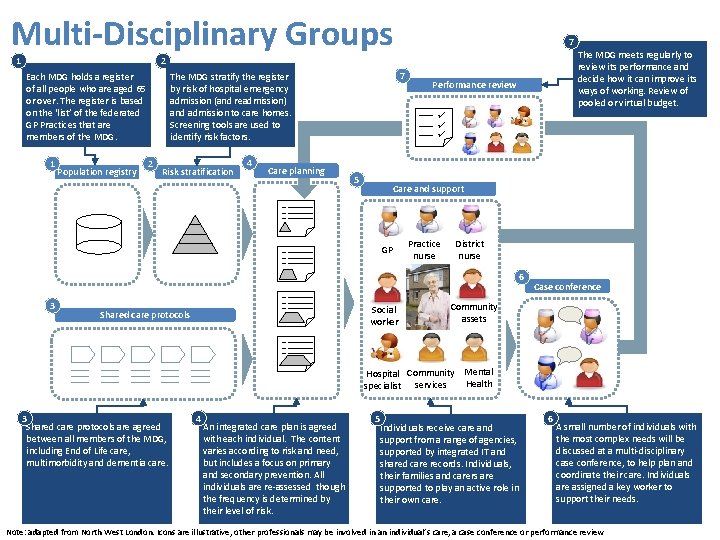
Multi-Disciplinary Groups 1 7 The MDG meets regularly to review its performance and decide how it can improve its ways of working. Review of pooled or virtual budget. 2 1 Population registry 2 7 The MDG stratify the register by risk of hospital emergency admission (and readmission) and admission to care homes. Screening tools are used to identify risk factors. Each MDG holds a register of all people who are aged 65 or over. The register is based on the ‘list’ of the federated GP Practices that are members of the MDG. Risk stratification 4 Care planning Performance review 5 Care and support GP Practice nurse District nurse 6 3 Social worker Shared care protocols Case conference Community assets Hospital Community Mental Health specialist services 3 Shared care protocols are agreed between all members of the MDG, including End of Life care, multimorbidity and dementia care. 4 An integrated care plan is agreed with each individual. The content varies according to risk and need, but includes a focus on primary and secondary prevention. All individuals are re-assessed though the frequency is determined by their level of risk. 5 Individuals receive care and support from a range of agencies, supported by integrated IT and shared care records. Individuals, their families and carers are supported to play an active role in their own care. 6 A small number of individuals with the most complex needs will be discussed at a multi-disciplinary case conference, to help plan and coordinate their care. Individuals are assigned a key worker to support their needs. Note: adapted from North West London. Icons are illustrative, other professionals may be involved in an individual’s care, a case conference or performance review

Integrated Health & Social Care Contact Team Providing people with information about their conditions, promoting healthy behaviours and helping with the emotional impact of chronic illness. People could be followed up over the phone for a specific period to encourage them to be more active participants in their care Post Discharge Support Self Care support Helping people to gain the knowledge, skills, tools and confidence to become active participants in their care so that they can reach their selfidentified goals. Health coaching Proactive follow up for people following their discharge from hospital. This could include a phone call within 48 hours of discharge. People at ‘high risk’ of readmission (stage 2 in MDG) would be followed up for 30 days or more. Navigation Remote Telecare Monitoring Guiding people to the appropriate part of the health and social care system to get the support they need. This function could link to a directory of services to support people in accessing local community assets. This could integrate existing care monitoring systems (e. g. community alarms) and new telehealth solutions, acting as central monitoring hub. 15
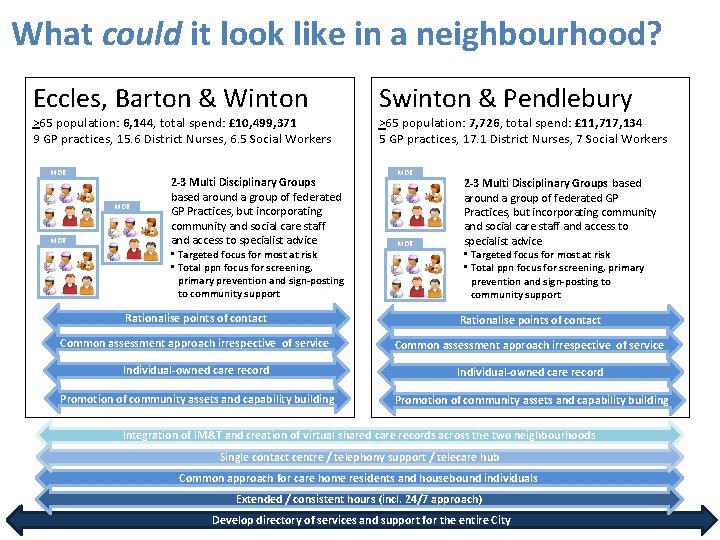
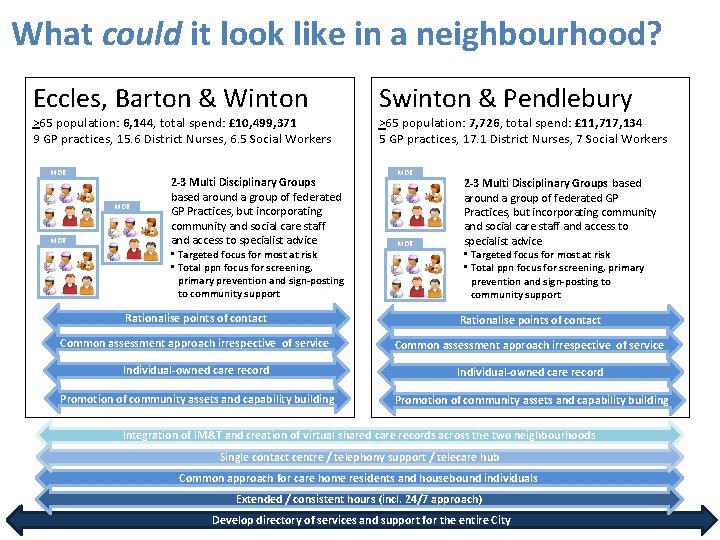
What could it look like in a neighbourhood? Eccles, Barton & Winton >65 population: 6, 144, total spend: £ 10, 499, 371 9 GP practices, 15. 6 District Nurses, 6. 5 Social Workers MDT MDT 2 -3 Multi Disciplinary Groups based around a group of federated GP Practices, but incorporating community and social care staff and access to specialist advice • Targeted focus for most at risk • Total ppn focus for screening, primary prevention and sign-posting to community support Swinton & Pendlebury >65 population: 7, 726, total spend: £ 11, 717, 134 5 GP practices, 17. 1 District Nurses, 7 Social Workers MDT 2 -3 Multi Disciplinary Groups based around a group of federated GP Practices, but incorporating community and social care staff and access to specialist advice • Targeted focus for most at risk • Total ppn focus for screening, primary prevention and sign-posting to community support Rationalise points of contact Common assessment approach irrespective of service Individual-owned care record Promotion of community assets and capability building Integration of IM&T and creation of virtual shared care records across the two neighbourhoods Single contact centre / telephony support / telecare hub Common approach for care home residents and housebound individuals Extended / consistent hours (incl. 24/7 approach) Develop directory of services and support for the entire City
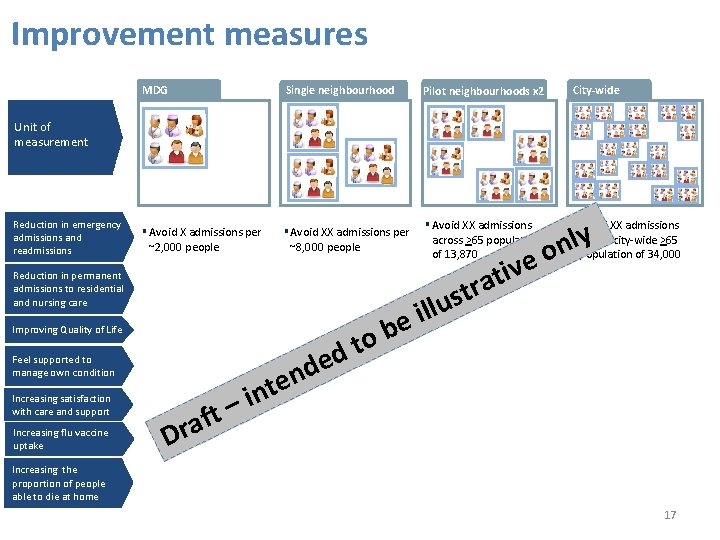
Improvement measures MDG Single neighbourhood ▪ Avoid X admissions per ▪ Avoid XX admissions per ▪ Avoid XX admissions across >65 population Pilot neighbourhoods x 2 City-wide Unit of measurement Reduction in emergency admissions and readmissions ~2, 000 people ~8, 000 people Reduction in permanent admissions to residential and nursing care b o t d Improving Quality of Life Feel supported to manage own condition – t f ra Increasing satisfaction with care and support Increasing flu vaccine uptake e v i t a r st of 13, 870 lu l i e ▪ Avoid XX admissions y l n o across city-wide >65 population of 34, 000 e d n e t in D Increasing the proportion of people able to die at home 17
Proposed partnership principles for MDGs • Holistic focus on Sally Ford and her family • Twin approach of ‘putting the fires out’ (targeting high users of service / those at greatest risk) and ‘fire prevention’ (primary prevention / early intervention) • Partnership of equals and collaborative approach, multi-disciplinary and multi-organisational • Shared leadership and accountability for performance • Commitment to honesty, trust and continuous improvement • Significant engagement with service users, carers and local communities 18
What would be different - for Sally Ford and her family? Greater independence Reduced isolation Confidence in managing own condition and care Know who to contact when necessary Increased community support available, with specialist care available when necessary • Support to plan for later stages in life • • • 19
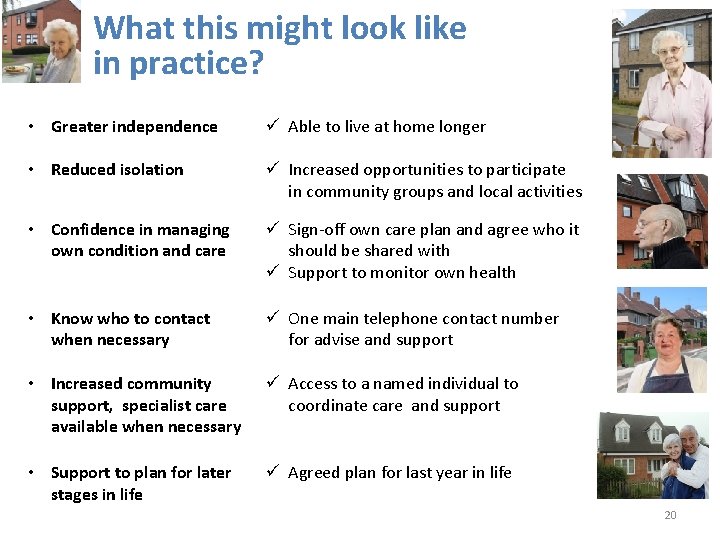
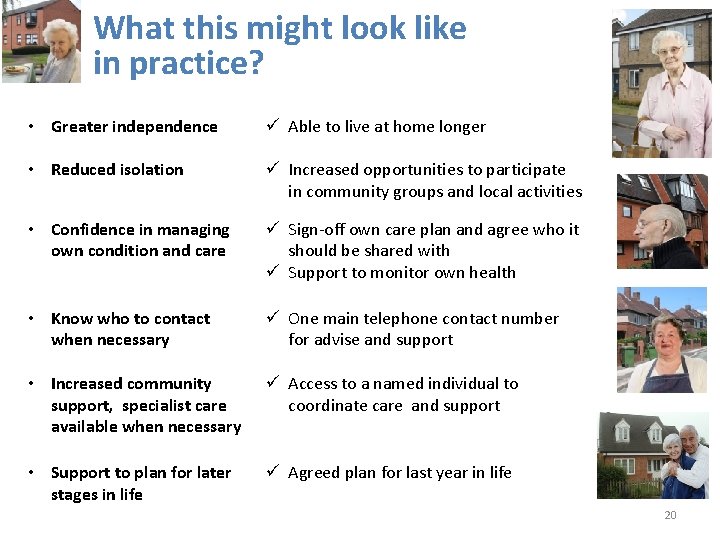
What this might look like in practice? • Greater independence Able to live at home longer • Reduced isolation Increased opportunities to participate in community groups and local activities • Confidence in managing own condition and care Sign-off own care plan and agree who it should be shared with Support to monitor own health • Know who to contact when necessary One main telephone contact number for advise and support • Increased community support, specialist care available when necessary Access to a named individual to coordinate care and support • Support to plan for later stages in life Agreed plan for last year in life 20
What would be different for public services? • Better able to provide holistic care for Sally and her family • Planned response to the challenges facing the public sector, minimising adverse consequences for staff and the public • Reduced duplication and fragmentation between services • Greater focus on prevention and planned care, reducing emergency demand • Closer working between professionals, teams and services • Professionals supported to manage risk and take decisions • System easier to understand navigate • Increased sense of purpose and job satisfaction 21
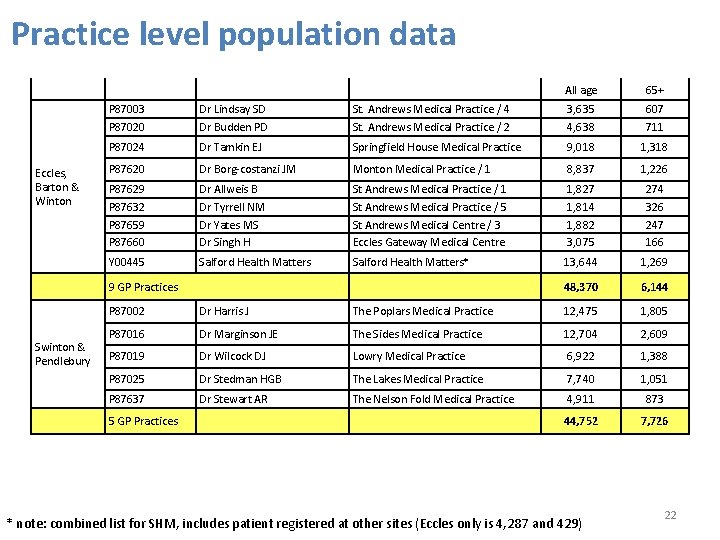
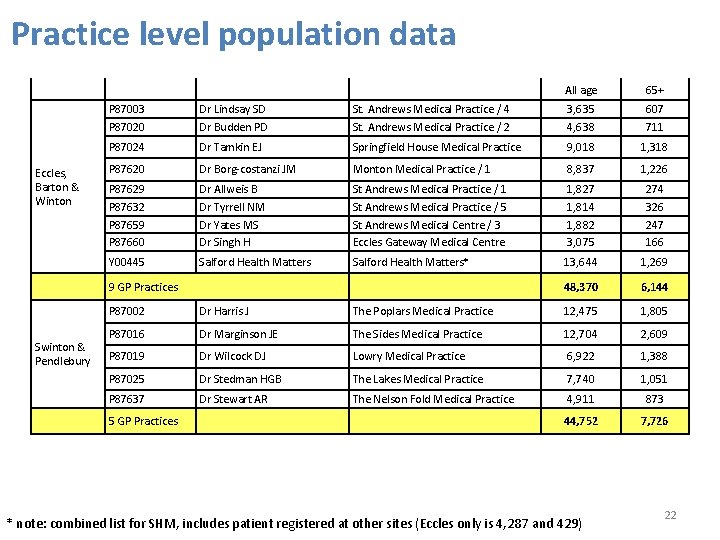
Practice level population data Eccles, Barton & Winton Swinton & Pendlebury All age 65+ P 87003 P 87020 Dr Lindsay SD Dr Budden PD St. Andrews Medical Practice / 4 St. Andrews Medical Practice / 2 3, 635 4, 638 607 711 P 87024 Dr Tamkin EJ Springfield House Medical Practice 9, 018 1, 318 P 87620 Dr Borg-costanzi JM Monton Medical Practice / 1 8, 837 1, 226 P 87629 P 87632 P 87659 P 87660 Dr Allweis B Dr Tyrrell NM Dr Yates MS Dr Singh H St Andrews Medical Practice / 1 St Andrews Medical Practice / 5 St Andrews Medical Centre / 3 Eccles Gateway Medical Centre 1, 827 1, 814 1, 882 3, 075 274 326 247 166 Y 00445 Salford Health Matters* 13, 644 1, 269 48, 370 6, 144 9 GP Practices P 87002 Dr Harris J The Poplars Medical Practice 12, 475 1, 805 P 87016 Dr Marginson JE The Sides Medical Practice 12, 704 2, 609 P 87019 Dr Wilcock DJ Lowry Medical Practice 6, 922 1, 388 P 87025 Dr Stedman HGB The Lakes Medical Practice 7, 740 1, 051 P 87637 Dr Stewart AR The Nelson Fold Medical Practice 4, 911 873 5 GP Practices 44, 752 7, 726 * note: combined list for SHM, includes patient registered at other sites (Eccles only is 4, 287 and 429) 22
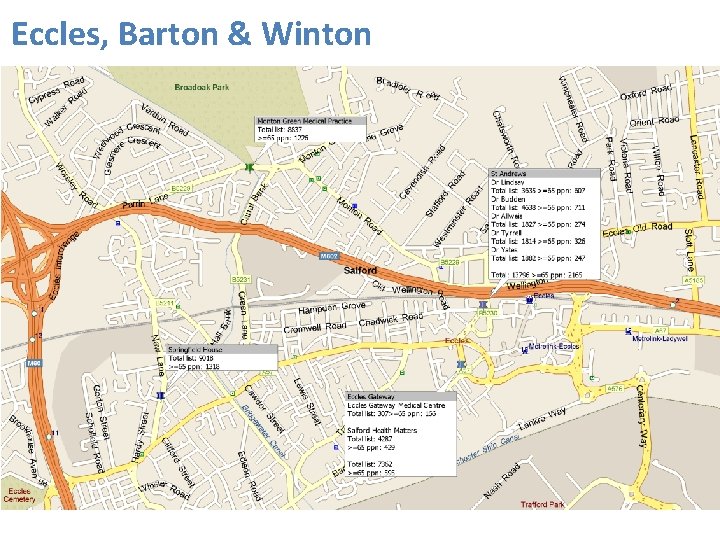
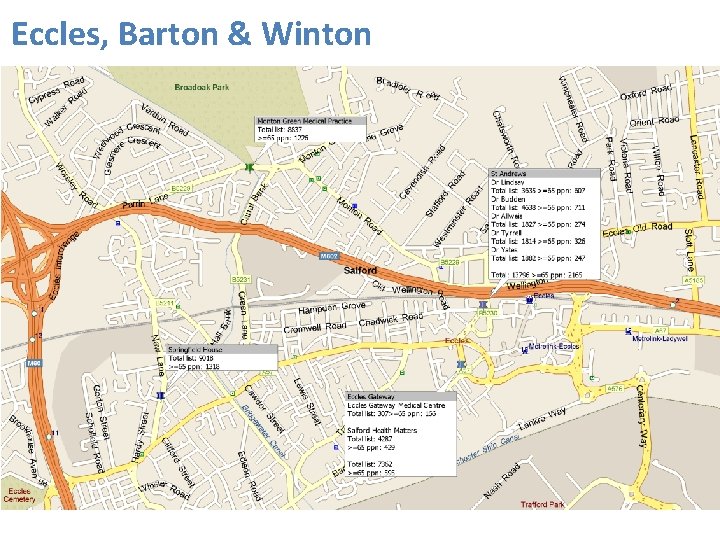
Eccles, Barton & Winton
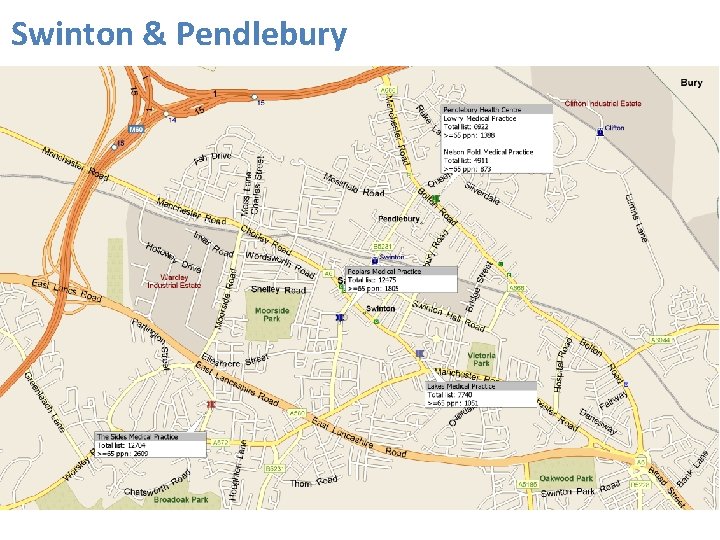
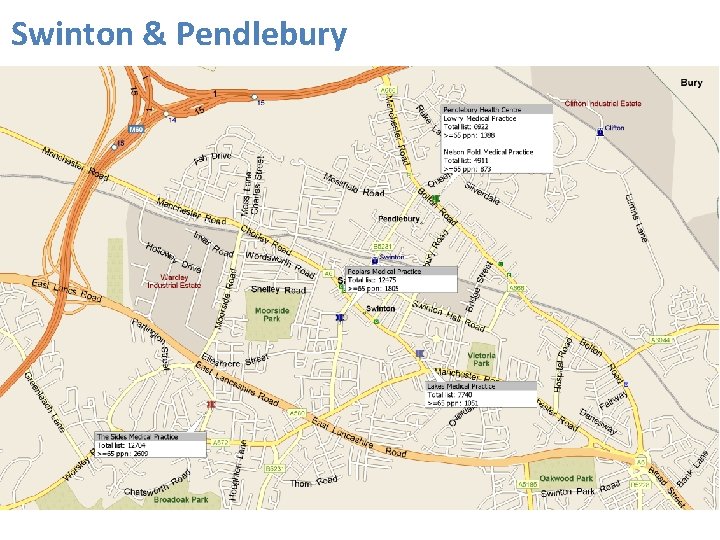
Swinton & Pendlebury
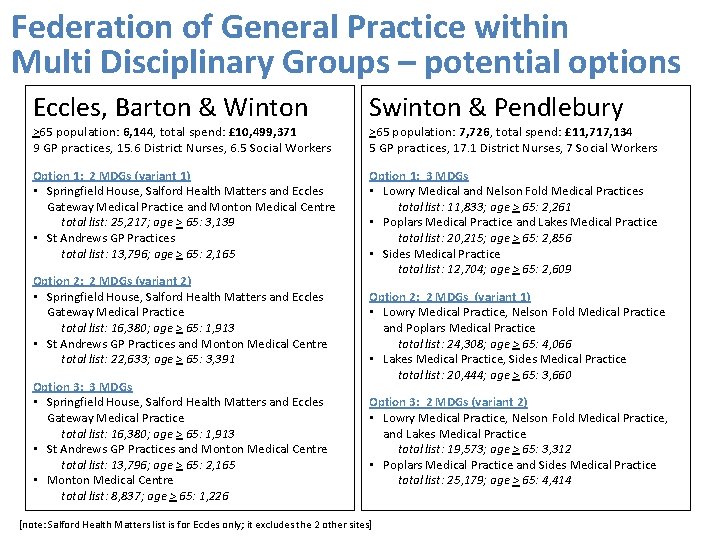
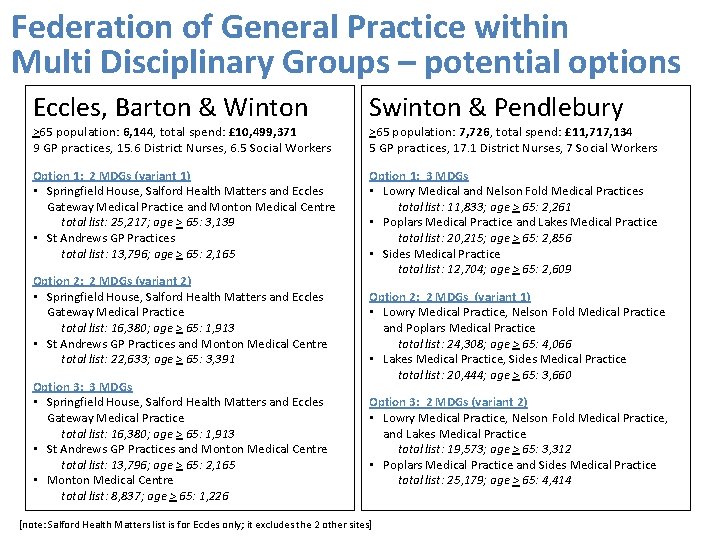
Federation of General Practice within Multi Disciplinary Groups – potential options Eccles, Barton & Winton Swinton & Pendlebury Option 1: 2 MDGs (variant 1) • Springfield House, Salford Health Matters and Eccles Gateway Medical Practice and Monton Medical Centre total list: 25, 217; age > 65: 3, 139 • St Andrews GP Practices total list: 13, 796; age > 65: 2, 165 Option 1: 3 MDGs • Lowry Medical and Nelson Fold Medical Practices total list: 11, 833; age > 65: 2, 261 • Poplars Medical Practice and Lakes Medical Practice total list: 20, 215; age > 65: 2, 856 • Sides Medical Practice total list: 12, 704; age > 65: 2, 609 >65 population: 6, 144, total spend: £ 10, 499, 371 9 GP practices, 15. 6 District Nurses, 6. 5 Social Workers Option 2: 2 MDGs (variant 2) • Springfield House, Salford Health Matters and Eccles Gateway Medical Practice total list: 16, 380; age > 65: 1, 913 • St Andrews GP Practices and Monton Medical Centre total list: 22, 633; age > 65: 3, 391 Option 3: 3 MDGs • Springfield House, Salford Health Matters and Eccles Gateway Medical Practice total list: 16, 380; age > 65: 1, 913 • St Andrews GP Practices and Monton Medical Centre total list: 13, 796; age > 65: 2, 165 • Monton Medical Centre total list: 8, 837; age > 65: 1, 226 >65 population: 7, 726, total spend: £ 11, 717, 134 5 GP practices, 17. 1 District Nurses, 7 Social Workers Option 2: 2 MDGs (variant 1) • Lowry Medical Practice, Nelson Fold Medical Practice and Poplars Medical Practice total list: 24, 308; age > 65: 4, 066 • Lakes Medical Practice, Sides Medical Practice total list: 20, 444; age > 65: 3, 660 Option 3: 2 MDGs (variant 2) • Lowry Medical Practice, Nelson Fold Medical Practice, and Lakes Medical Practice total list: 19, 573; age > 65: 3, 312 • Poplars Medical Practice and Sides Medical Practice total list: 25, 179; age > 65: 4, 414 [note: Salford Health Matters list is for Eccles only; it excludes the 2 other sites]
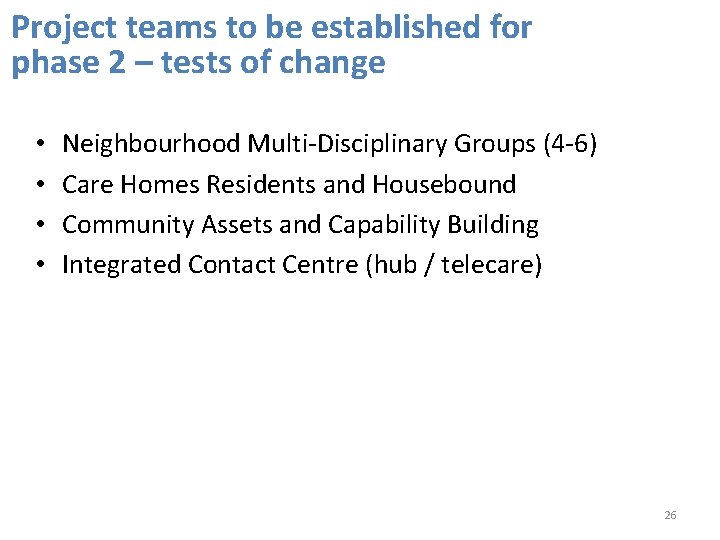
Project teams to be established for phase 2 – tests of change • • Neighbourhood Multi-Disciplinary Groups (4 -6) Care Homes Residents and Housebound Community Assets and Capability Building Integrated Contact Centre (hub / telecare) 26
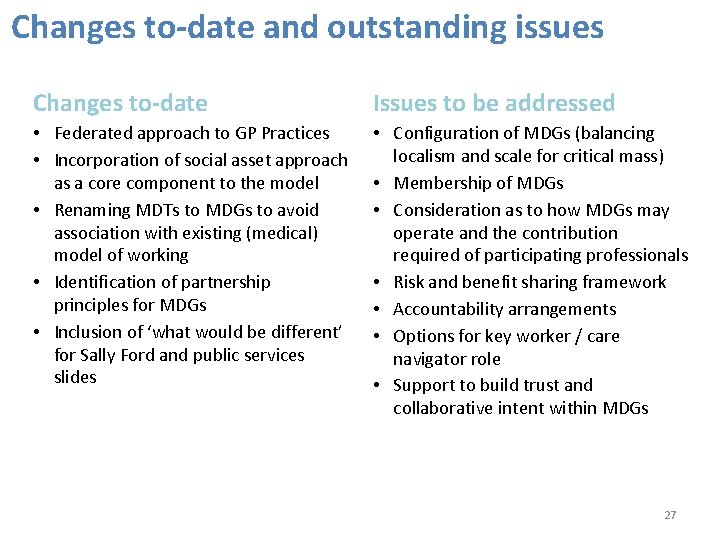
Changes to-date and outstanding issues Changes to-date Issues to be addressed • Federated approach to GP Practices • Incorporation of social asset approach as a core component to the model • Renaming MDTs to MDGs to avoid association with existing (medical) model of working • Identification of partnership principles for MDGs • Inclusion of ‘what would be different’ for Sally Ford and public services slides • Configuration of MDGs (balancing localism and scale for critical mass) • Membership of MDGs • Consideration as to how MDGs may operate and the contribution required of participating professionals • Risk and benefit sharing framework • Accountability arrangements • Options for key worker / care navigator role • Support to build trust and collaborative intent within MDGs 27
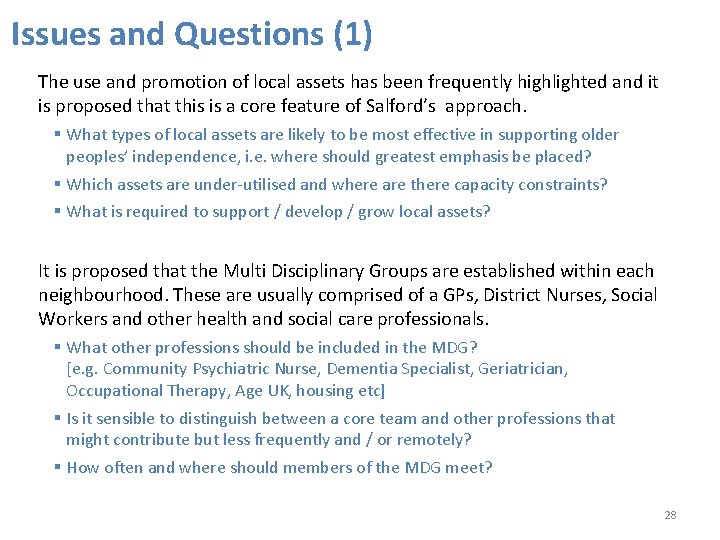
Issues and Questions (1) The use and promotion of local assets has been frequently highlighted and it is proposed that this is a core feature of Salford’s approach. § What types of local assets are likely to be most effective in supporting older peoples’ independence, i. e. where should greatest emphasis be placed? § Which assets are under-utilised and where are there capacity constraints? § What is required to support / develop / grow local assets? It is proposed that the Multi Disciplinary Groups are established within each neighbourhood. These are usually comprised of a GPs, District Nurses, Social Workers and other health and social care professionals. § What other professions should be included in the MDG? [e. g. Community Psychiatric Nurse, Dementia Specialist, Geriatrician, Occupational Therapy, Age UK, housing etc] § Is it sensible to distinguish between a core team and other professions that might contribute but less frequently and / or remotely? § How often and where should members of the MDG meet? 28
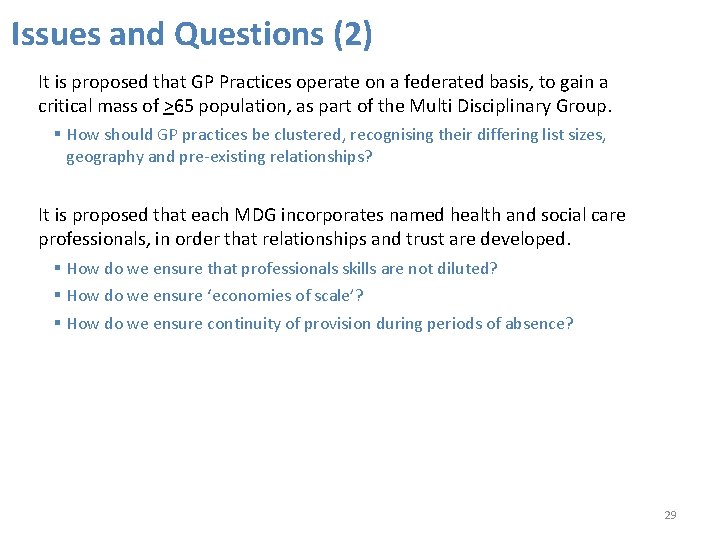
Issues and Questions (2) It is proposed that GP Practices operate on a federated basis, to gain a critical mass of >65 population, as part of the Multi Disciplinary Group. § How should GP practices be clustered, recognising their differing list sizes, geography and pre-existing relationships? It is proposed that each MDG incorporates named health and social care professionals, in order that relationships and trust are developed. § How do we ensure that professionals skills are not diluted? § How do we ensure ‘economies of scale’? § How do we ensure continuity of provision during periods of absence? 29
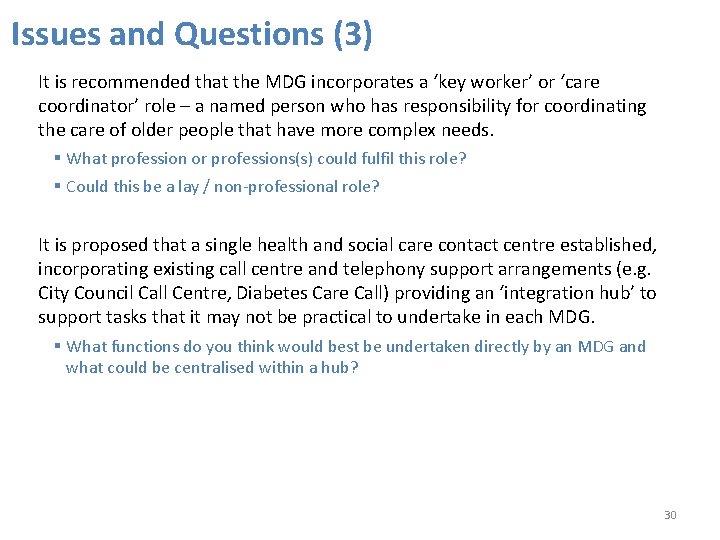
Issues and Questions (3) It is recommended that the MDG incorporates a ‘key worker’ or ‘care coordinator’ role – a named person who has responsibility for coordinating the care of older people that have more complex needs. § What profession or professions(s) could fulfil this role? § Could this be a lay / non-professional role? It is proposed that a single health and social care contact centre established, incorporating existing call centre and telephony support arrangements (e. g. City Council Call Centre, Diabetes Care Call) providing an ‘integration hub’ to support tasks that it may not be practical to undertake in each MDG. § What functions do you think would best be undertaken directly by an MDG and what could be centralised within a hub? 30
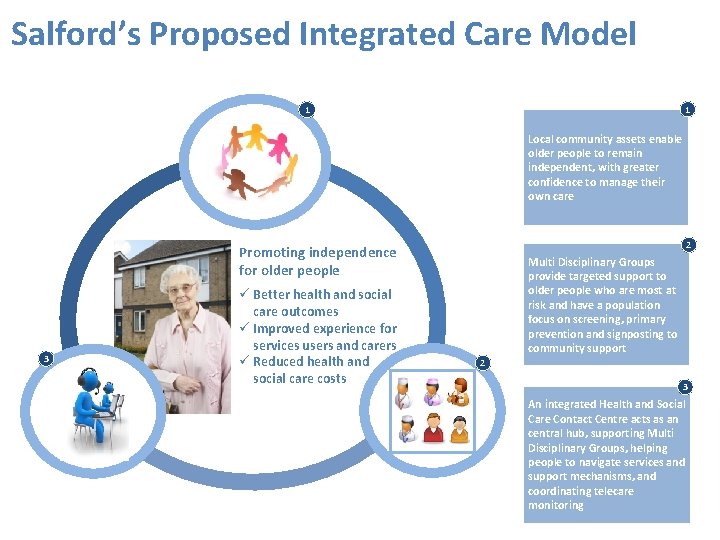
Salford’s Proposed Integrated Care Model 1 1 Local community assets enable older people to remain independent, with greater confidence to manage their own care 2 Promoting independence for older people 3 Better health and social care outcomes Improved experience for services users and carers Reduced health and social care costs Multi Disciplinary Groups provide targeted support to older people who are most at risk and have a population focus on screening, primary prevention and signposting to community support 2 3 An integrated Health and Social Care Contact Centre acts as an central hub, supporting Multi Disciplinary Groups, helping people to navigate services and support mechanisms, and coordinating telecare monitoring