Rhode Island Nursing Facility Payment Methodology Status Update
- Slides: 13
Rhode Island Nursing Facility Payment Methodology: Status Update March 15, 2012
Agenda n Overview of Base Methodology n Options for Transition n Recognition of Quality and Dementia
EOHHS Nursing Home Rate Method Objectives n Budget Neutrality n Pay Higher Rates for Higher Acuity q q Implementation of an Acuity Adjustment for Nursing Homes, July 2010 reimburse homes based on each patient's specific RUG category n Payment method that ensures ease of administration and predictability n Transition from a facility specific cost based system to a price based model similar to Medicare PPS
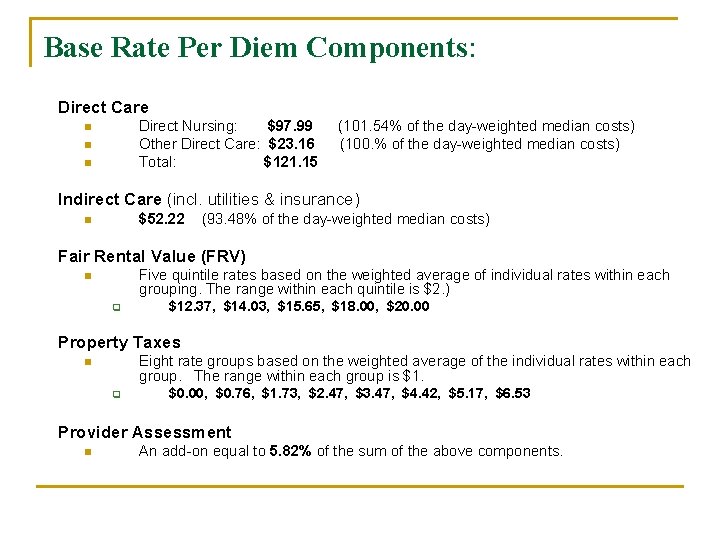
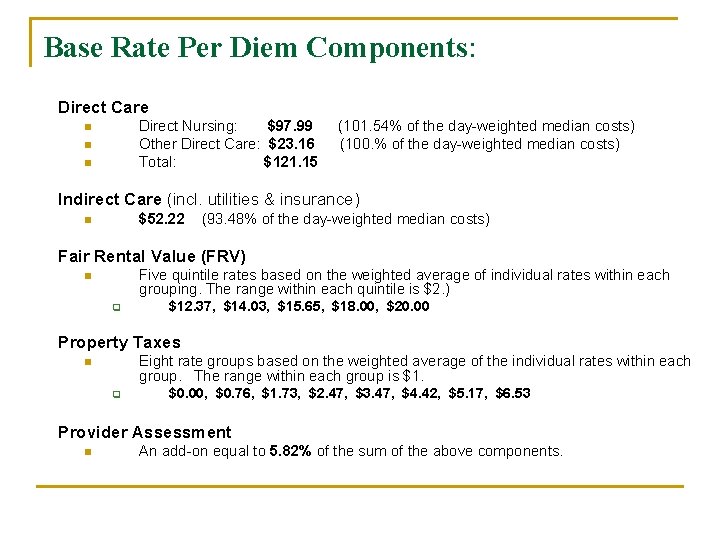
Base Rate Per Diem Components: Direct Care Direct Nursing: $97. 99 Other Direct Care: $23. 16 Total: $121. 15 n n n (101. 54% of the day-weighted median costs) (100. % of the day-weighted median costs) Indirect Care (incl. utilities & insurance) $52. 22 n (93. 48% of the day-weighted median costs) Fair Rental Value (FRV) Five quintile rates based on the weighted average of individual rates within each grouping. The range within each quintile is $2. ) n q $12. 37, $14. 03, $15. 65, $18. 00, $20. 00 Property Taxes Eight rate groups based on the weighted average of the individual rates within each group. The range within each group is $1. n q $0. 00, $0. 76, $1. 73, $2. 47, $3. 47, $4. 42, $5. 17, $6. 53 Provider Assessment n An add-on equal to 5. 82% of the sum of the above components.
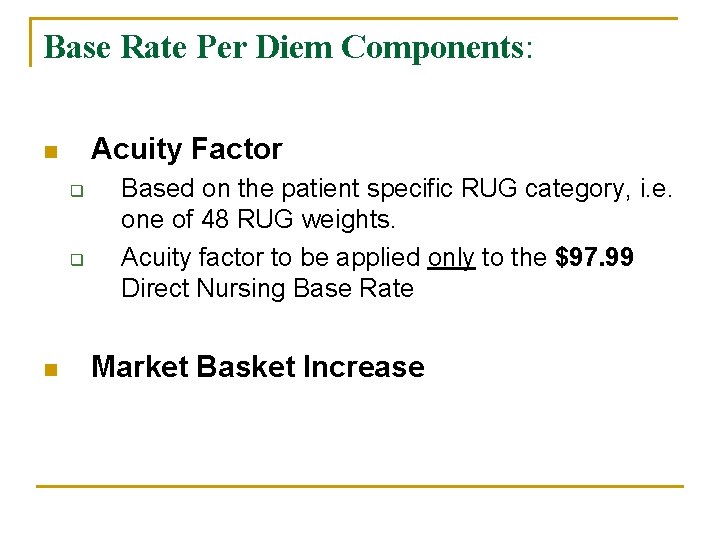
Base Rate Per Diem Components: Acuity Factor n q q n Based on the patient specific RUG category, i. e. one of 48 RUG weights. Acuity factor to be applied only to the $97. 99 Direct Nursing Base Rate Market Basket Increase
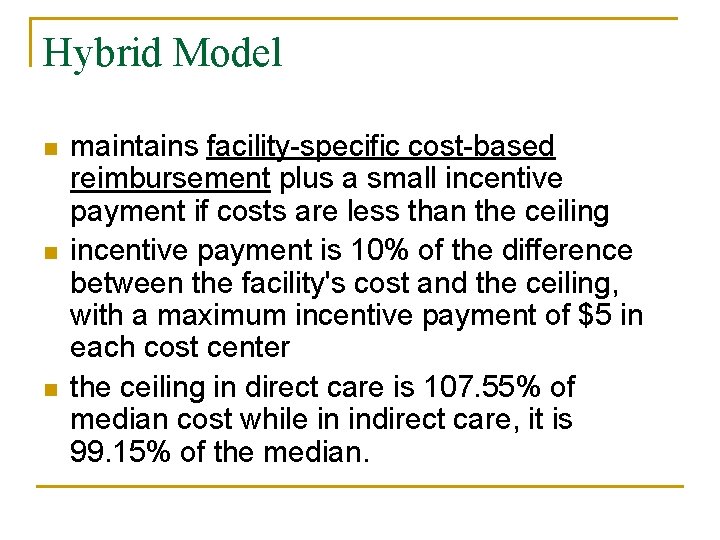
Hybrid Model n n n maintains facility-specific cost-based reimbursement plus a small incentive payment if costs are less than the ceiling incentive payment is 10% of the difference between the facility's cost and the ceiling, with a maximum incentive payment of $5 in each cost center the ceiling in direct care is 107. 55% of median cost while in indirect care, it is 99. 15% of the median.
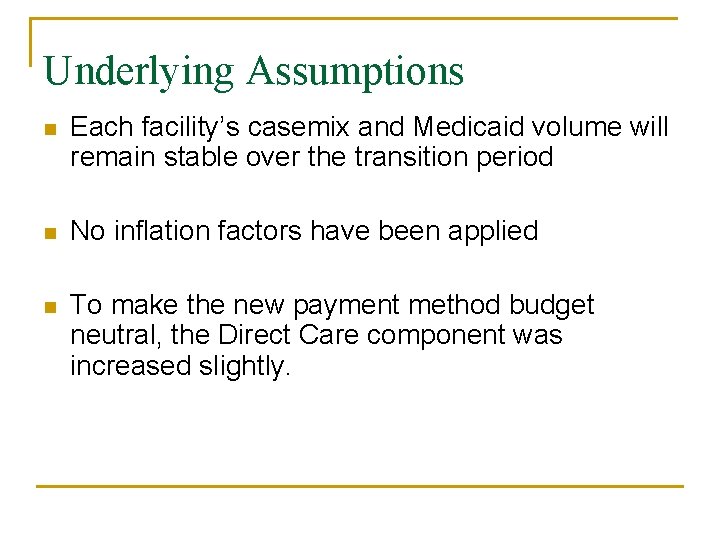
Underlying Assumptions n Each facility’s casemix and Medicaid volume will remain stable over the transition period n No inflation factors have been applied n To make the new payment method budget neutral, the Direct Care component was increased slightly.
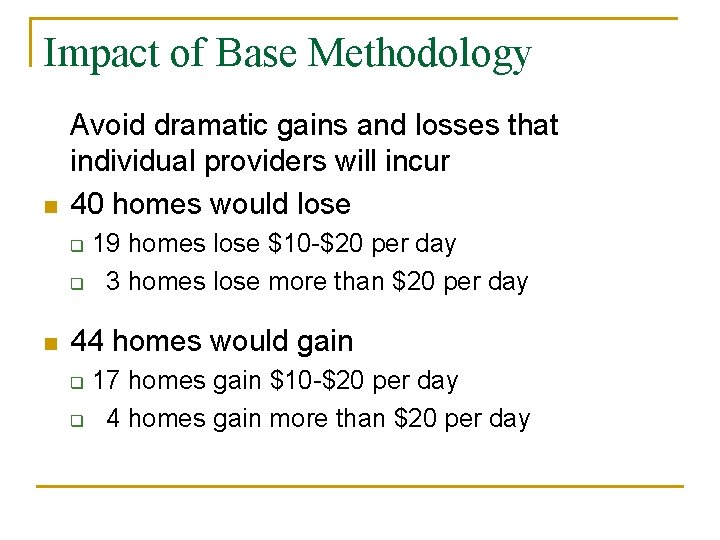
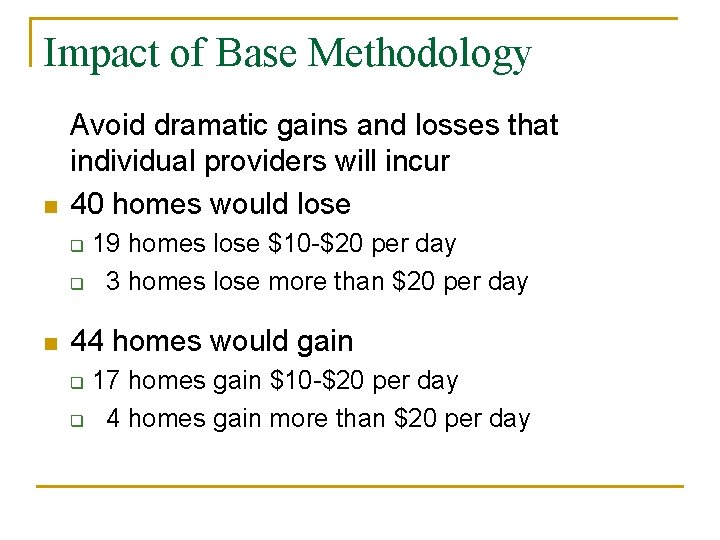
Impact of Base Methodology n Avoid dramatic gains and losses that individual providers will incur 40 homes would lose 19 homes lose $10 -$20 per day q 3 homes lose more than $20 per day q n 44 homes would gain 17 homes gain $10 -$20 per day q 4 homes gain more than $20 per day q
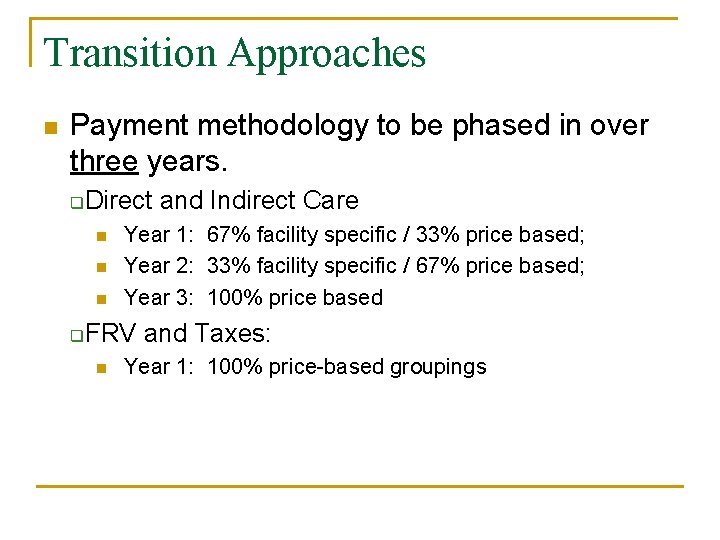
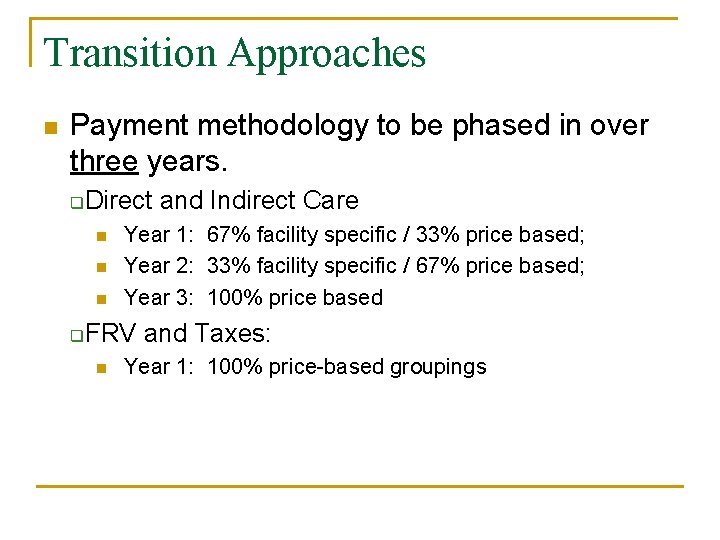
Transition Approaches n Payment methodology to be phased in over three years. q Direct and Indirect Care n n n q Year 1: 67% facility specific / 33% price based; Year 2: 33% facility specific / 67% price based; Year 3: 100% price based FRV and Taxes: n Year 1: 100% price-based groupings
Transition Approaches Policy Adjustor - No home loses more than $5. 00 - No home gains more than $5. 00 - Maintains existing direct care costs
Transition Approaches
Recognition of Quality and Dementia n Need to agree on basic approach first n 2 -3 meetings in April – early May
Discussion n Next steps