Regional Citrate Anticoagulation during CVVH in the Pediatric
- Slides: 13
Regional Citrate Anticoagulation during CVVH in the Pediatric Intensive Care Unit T Gaillot, V Phan, P Jouvet, F Gauvin, C Litalien
Introduction • CVVH is being increasingly utilized for the care of PICU patients • Imperative need : Effective anticoagulation to prevent recurrent clotting of the extracorporeal circuit and to achieve efficient and uninterrupted therapy • Historically, systemic anticoagulation with heparin mainstay of anticoagulation for CVVH • Limits/contraindications : • High risk for bleeding • Active bleeding • Heparin-induced thrombocytopenia • Use of activated Protein C
Introduction Regional citrate anticoagulation (RCA): • Attractive alternative to systemic heparinization with less risk of bleeding • Citrate chelates ionized Ca 2+, an essential cofactor in the clotting cascade • Anticoagulation is limited to the extracorporeal circuit by infusing citrate solution into the arterial limb of the circuit • Systemic anticoagulation is avoided by restoring ionized Ca 2+ in the systemic circulation by infusing Ca 2+ solution through a separate central line
Introduction RCA and mean circuit lifetime: • Adult studies Monchi et al, 2004: RCA vs heparin: 70 h vs 40 h Dorval et al, 2003: 44 24 h • Pediatric studies Chadha et al, 2002: 51 8 h Elhanan et al, 2004: 56 22 h Bunchman et al, 2002: 71 7 h
Introduction RCA and complications: • Citrate is metabolized in the liver and produces HCO 3 and citric acid can result in metabolic alkalosis • Accumulation of citrate may occur if liver metabolism is impaired can result in citrate toxicity or "citrate gap"
Objective To evaluate the mean circuit lifetime and metabolic complications of RCA in critically ill children after the introduction of this anticoagulation technique in our PICU
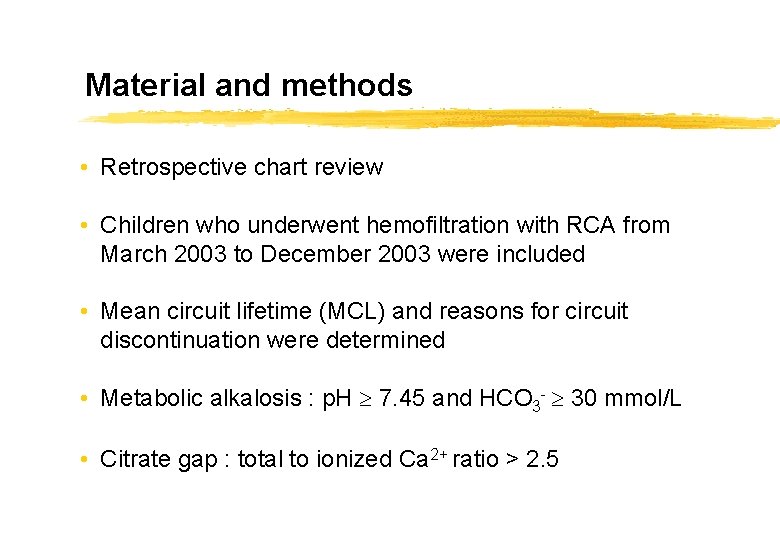
Material and methods • Retrospective chart review • Children who underwent hemofiltration with RCA from March 2003 to December 2003 were included • Mean circuit lifetime (MCL) and reasons for circuit discontinuation were determined • Metabolic alkalosis : p. H 7. 45 and HCO 3 - 30 mmol/L • Citrate gap : total to ionized Ca 2+ ratio > 2. 5
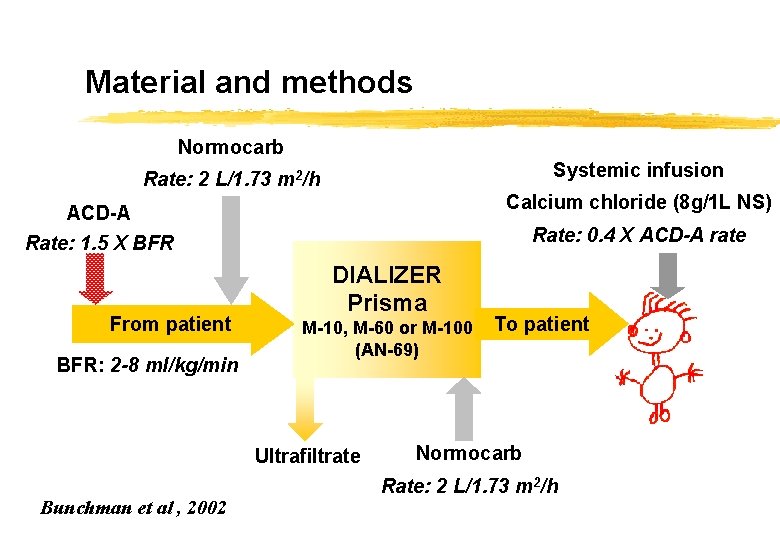
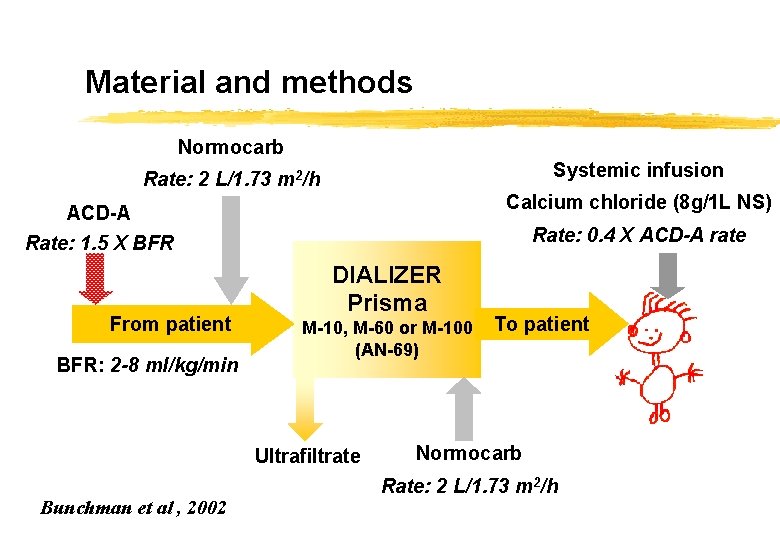
Material and methods Normocarb Systemic infusion Rate: 2 L/1. 73 m 2/h Calcium chloride (8 g/1 L NS) ACD-A Rate: 1. 5 X BFR From patient BFR: 2 -8 ml/kg/min Rate: 0. 4 X ACD-A rate DIALIZER Prisma M-10, M-60 or M-100 (AN-69) Ultrafiltrate Bunchman et al , 2002 To patient Normocarb Rate: 2 L/1. 73 m 2/h
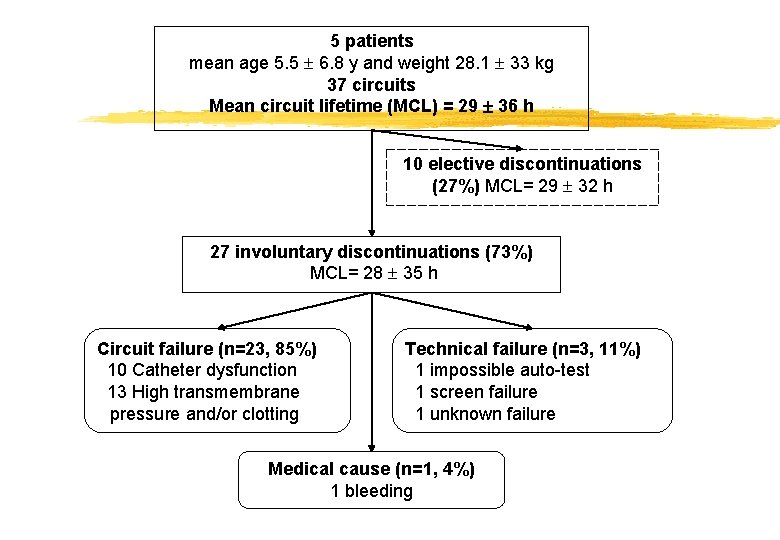
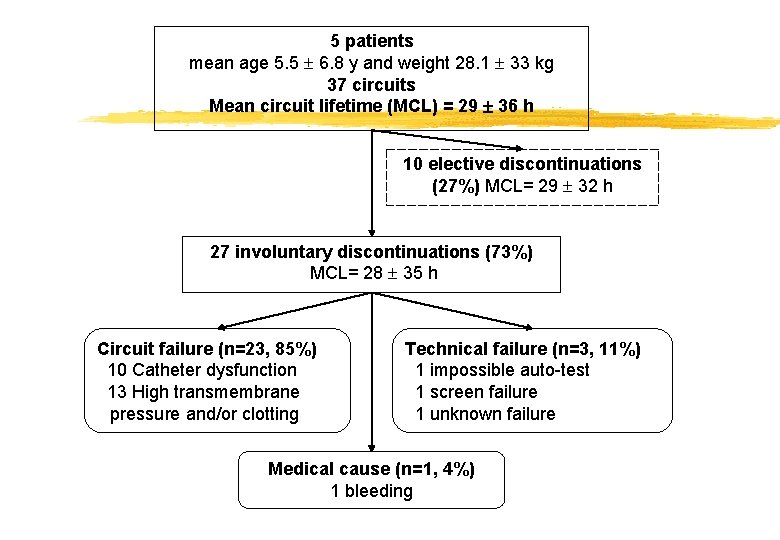
5 patients mean age 5. 5 6. 8 y and weight 28. 1 33 kg 37 circuits Mean circuit lifetime (MCL) = 29 36 h 10 elective discontinuations (27%) MCL= 29 32 h 27 involuntary discontinuations (73%) MCL= 28 35 h Circuit failure (n=23, 85%) 10 Catheter dysfunction 13 High transmembrane pressure and/or clotting Technical failure (n=3, 11%) 1 impossible auto-test 1 screen failure 1 unknown failure Medical cause (n=1, 4%) 1 bleeding
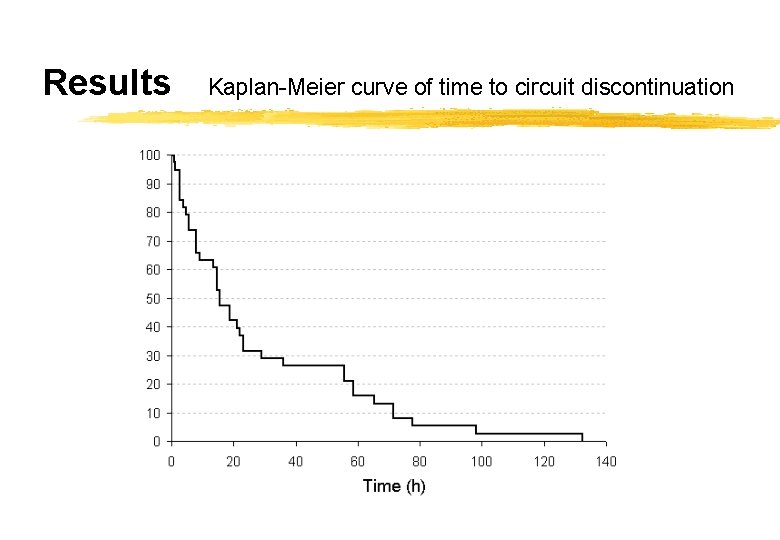
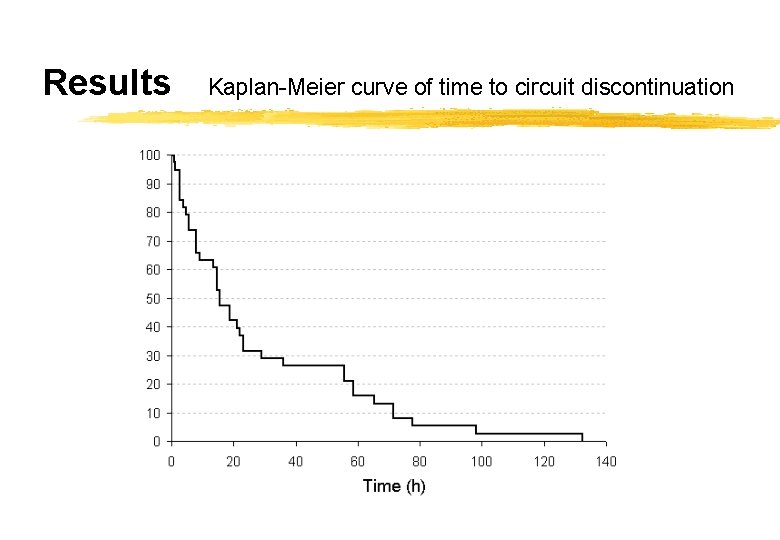
Results Kaplan-Meier curve of time to circuit discontinuation
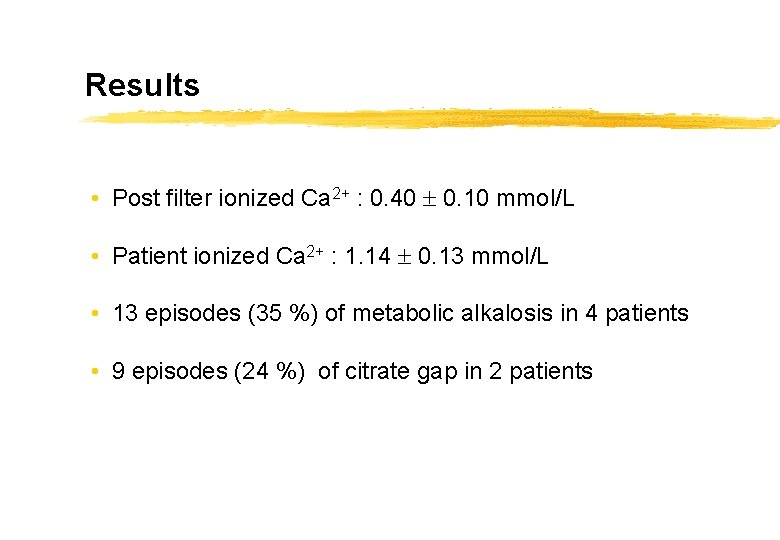
Results • Post filter ionized Ca 2+ : 0. 40 0. 10 mmol/L • Patient ionized Ca 2+ : 1. 14 0. 13 mmol/L • 13 episodes (35 %) of metabolic alkalosis in 4 patients • 9 episodes (24 %) of citrate gap in 2 patients
Conclusion • In our PICU, the mean circuit lifetime using RCA was much shorter than those reported despite post-filter ionized Ca 2+ within the optimum range • Metabolic alkalosis was frequently encountered • Citrate toxicity occurred in 2 patients out of 5 • The use of RCA may be somewhat problematic in some critically ill children
Perspectives • RCA remains an attractive option to provide anticoagulation in those patients with heparin contraindications • Prospective, randomized controlled trials comparing RCA and systemic heparinization are needed before RCA replaces heparin in all critically ill children