Profile of Children with Special Health Care Needs



- Slides: 27


Profile of Children with Special Health Care Needs in Ohio Anthony Goudie, Ph. D.
Acknowledgements • Project Collaborators o Gerry Fairbrother, Ph. D. o Lisa Simpson, MB, BCh. , MPH, FAAP o Keith Mandel, M. D.
Acknowledgements • OFHS Reviewers o Dr. James Bryant, ODH o Harvey Doremus, ODJFS o Karen Hughes, ODH o Dr. Lisa Raiz, OSU
Agenda • • CSHCN in Ohio - Who Are They? Level of Complexity Unmet Needs / Health Care Access Problems or Barriers Policy Implications
CSHCN in Ohio - Who Are They?
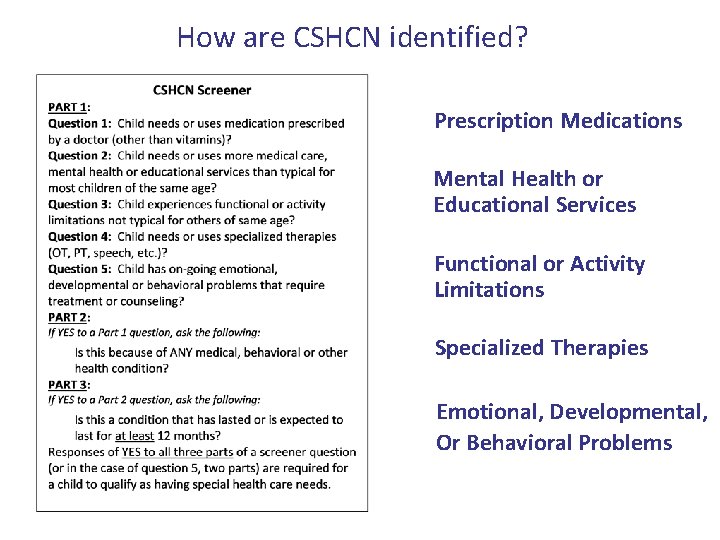
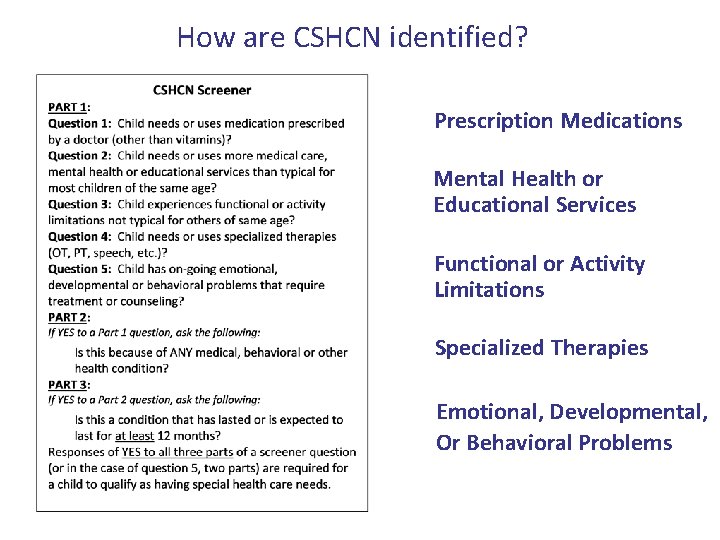
How are CSHCN identified? Prescription Medications Mental Health or Educational Services Functional or Activity Limitations Specialized Therapies Emotional, Developmental, Or Behavioral Problems
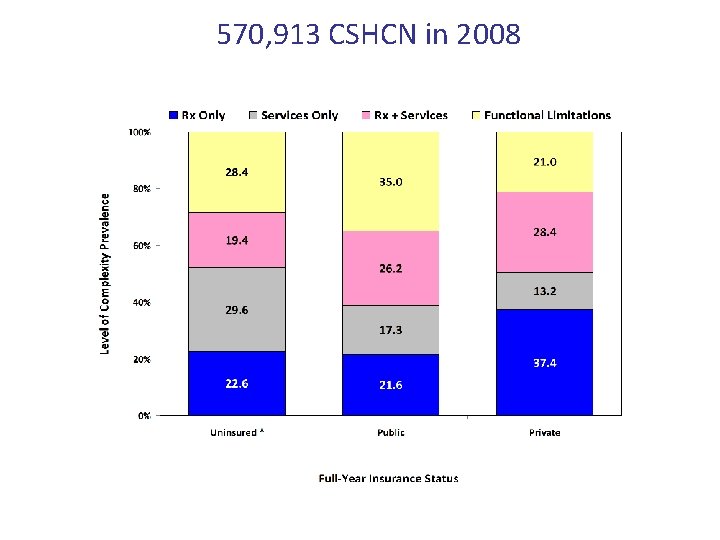
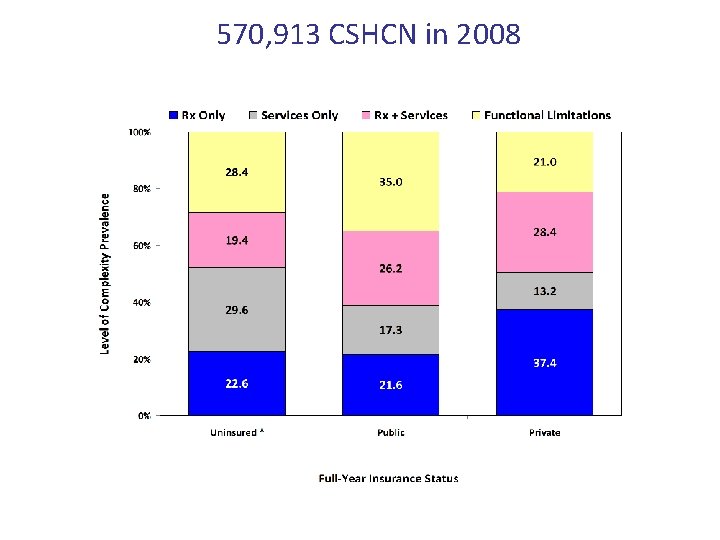
570, 913 CSHCN in 2008
CSHCN in Ohio - Demographics
CSHCN in Ohio – Health Status
CSHCN in Ohio – Insurance Status Note: Uninsured are those without insurance for all or part of the 12 months prior to the survey.
Level of Complexity
Level of Complexity Among CSHCN
CSHCN by Level of Complexity
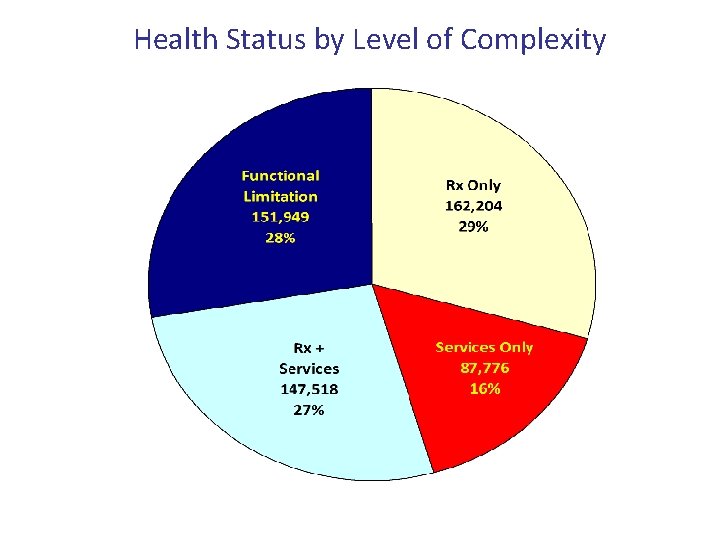
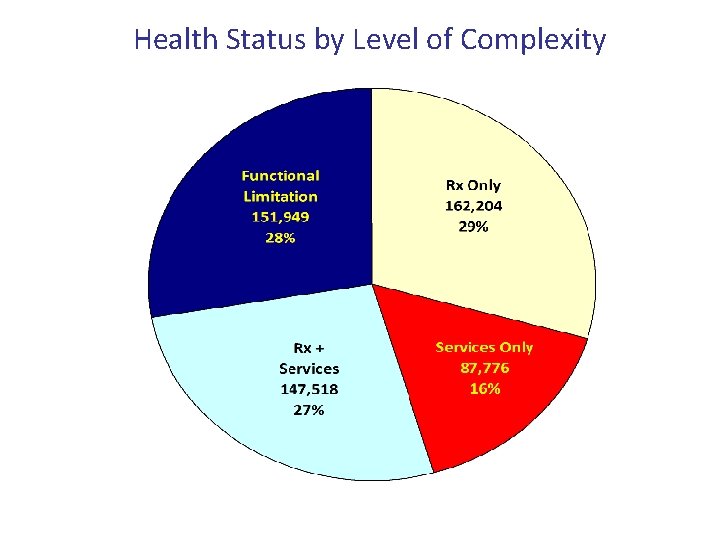
Health Status by Level of Complexity
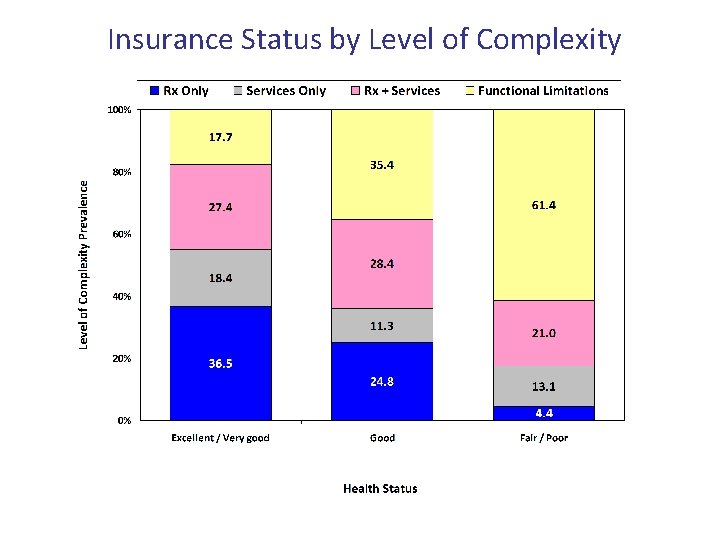
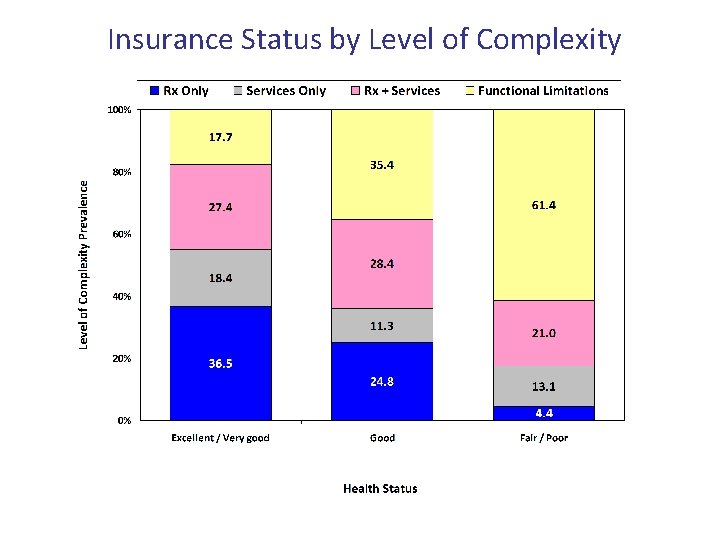
Insurance Status by Level of Complexity
Unmet Needs / Health Care Access Problems or Barriers
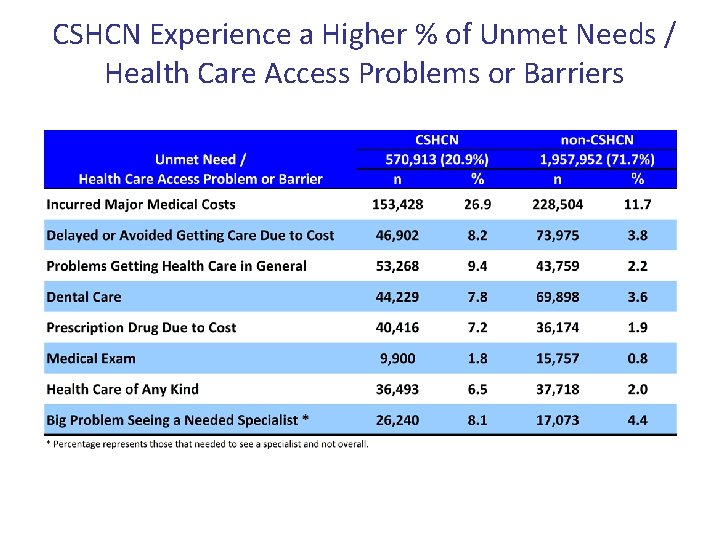
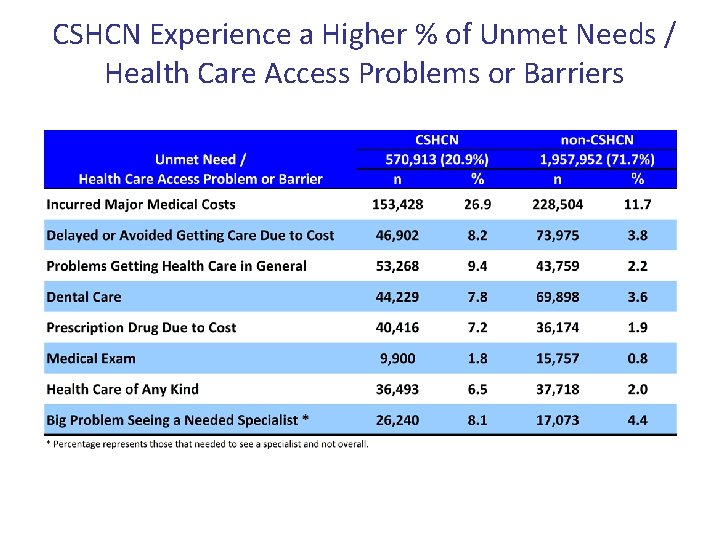
CSHCN Experience a Higher % of Unmet Needs / Health Care Access Problems or Barriers
Families of CSHCN who incur major medical costs are: • Twice as likely to be covered by private than public insurance • Almost 3 times as likely to have poor, fair, or good than very good or excellent health status
CSHCN who delay or avoid getting needed health care are: • 10 times more likely to be uninsured than privately insured • Twice as likely to be older (ages 13 -17) than younger • Twice as likely to have poor, fair, or good than very good or excellent health status • 4 times as likely to live in a rural (non-Appalachian) region compared to Hamilton county
CSHCN who do not get needed prescription medications due to cost are: • Greater than 10 times more likely to be uninsured than privately insured • Twice as likely to be under 6 than between 13 -17 years of age • Twice as likely to have poor, fair, or good than very good or excellent health status • 4 times as likely to live in a rural (non-Appalachian) region compared to Hamilton county
Families of CSHCN who have an unmet need for health care of any kind are: • Greater than 6 times as likely to be uninsured than covered by private insurance • Almost twice as likely to have poor, fair, or good than very good or excellent health status
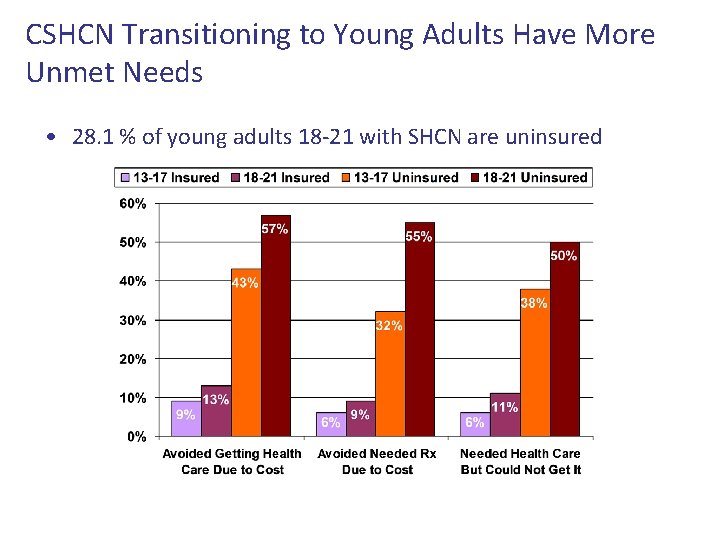
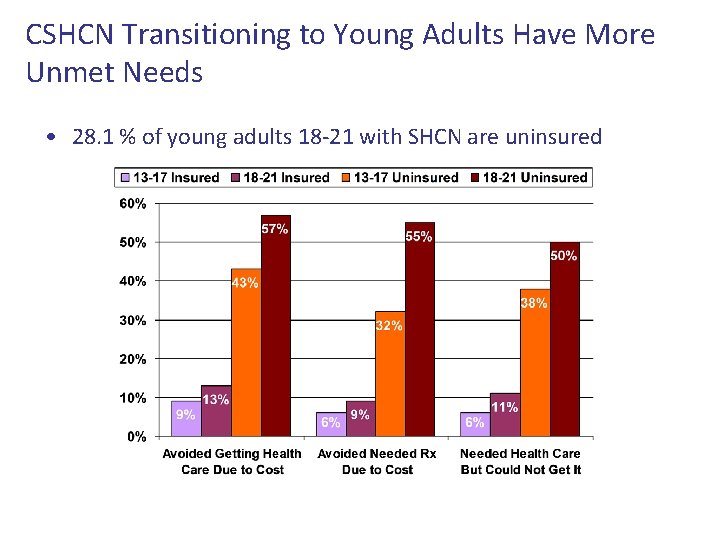
CSHCN Transitioning to Young Adults Have More Unmet Needs • 28. 1 % of young adults 18 -21 with SHCN are uninsured

Policy Implications
Policy Implications • Stable and adequate health care insurance is vital for this vulnerable pediatric population • Early screening for diagnoses of chronic conditions if they manifest at an early age • Focus on CSHCN transitioning to adulthood to avoid high levels of unmet needs
Policy Implications • Entire families are impacted by caring for a child with SHCN • The health care system is but one of many that CSHCN interact with, and coordination between all is important for quality of life and well-being (e. g. behavior in school may be due to poor adherence taking medications)
Thank You Anthony. Goudie@cchmc. org
 Friends of children with special needs
Friends of children with special needs Elderplan plan materials
Elderplan plan materials Primary secondary and tertiary care
Primary secondary and tertiary care Unit 18 assessing children's development support needs p1
Unit 18 assessing children's development support needs p1 Personal needs profile definition
Personal needs profile definition Primary needs and secondary needs
Primary needs and secondary needs Primary needs and secondary needs
Primary needs and secondary needs Alpha press murray
Alpha press murray Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Types of needs analysis in esp
Types of needs analysis in esp Unit 2 equality diversity and rights
Unit 2 equality diversity and rights Health and social care component 3
Health and social care component 3 Exceptional children 11th edition
Exceptional children 11th edition Exceptional children an introduction to special education
Exceptional children an introduction to special education Project based learning for special education
Project based learning for special education Teachwise app
Teachwise app Special educational needs and disability act 2001
Special educational needs and disability act 2001 Special needs trust virginia
Special needs trust virginia Colorado special needs trust
Colorado special needs trust Instructional adaptations for special needs students
Instructional adaptations for special needs students Special needs summer cmap
Special needs summer cmap How can an sna help a child with autism
How can an sna help a child with autism European agency for development in special needs education
European agency for development in special needs education Safpf special needs
Safpf special needs Safeguarding special needs
Safeguarding special needs Safeguarding children care certificate
Safeguarding children care certificate Nj children's system of care
Nj children's system of care Care and protection of children act
Care and protection of children act