Presentation EPR 2083 Impact of an Employerprovided Migraine

- Slides: 8
Presentation #EPR 2083 Impact of an Employer-provided Migraine Coaching Program on Patient Burden and Engagement Scan to download a copy of this presentation Leonhard Schaetz 1, Timo Rimner 2, Purnima Pathak 3, Juanzhi Fang 4, Francois Cadiou 5, Deepak Chandrasekhar 5, Lawrence Vandervoort 5, Jelena Mueller 1, Andreas R. Gantenbein 6* 1 Novartis Pharma AG, Basel, Switzerland; 2 Medgate, Basel, Switzerland; 3 Novartis Ireland Limited, Dublin, Ireland; 4 Novartis Pharma US, East Hanover, USA; 5 Healint Pte. Ltd, Singapore; 6 Bad Zurzach, Switzerland 6 th Congress of the European Academy of Neurology, Paris, 23 – 26 May, 2020 Background Methods Results Conclusions
Schaetz et al. | EPR 2083 | Headache and Pain 4 Background • With an aim to raise awareness of migraine in the workplace and provide coaching on migraine management to employees and their family members living with migraine, Novartis launched the Migraine Care program in collaboration with patient groups and leading experts in neurology, telemedicine and digital • The program was provided as a complimentary service to all Swiss-based Novartis associates and their family members to empower them in the management of the disease and improve their quality of life • The objective of this study was to assess the impact of Migraine Care program among its participants (Swiss-based Novartis associates and their family members) 3
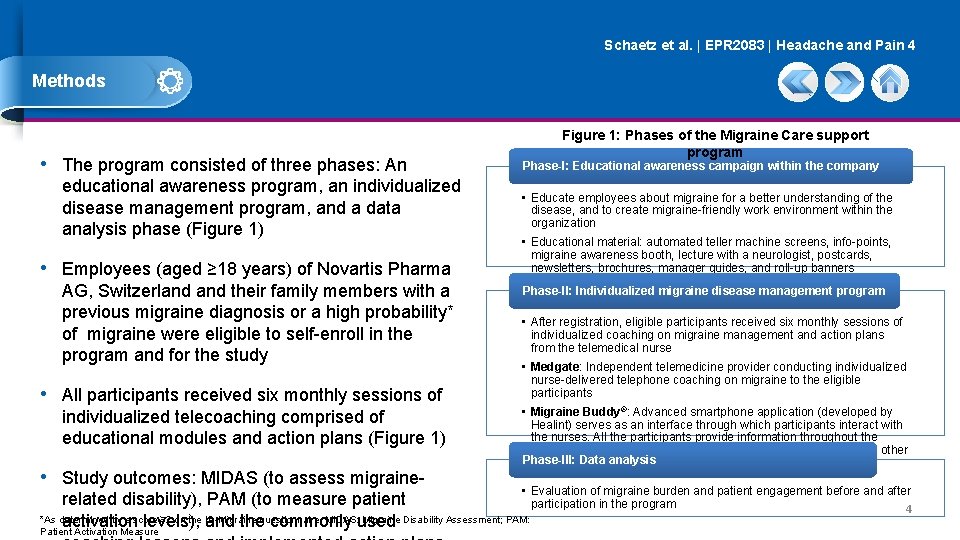
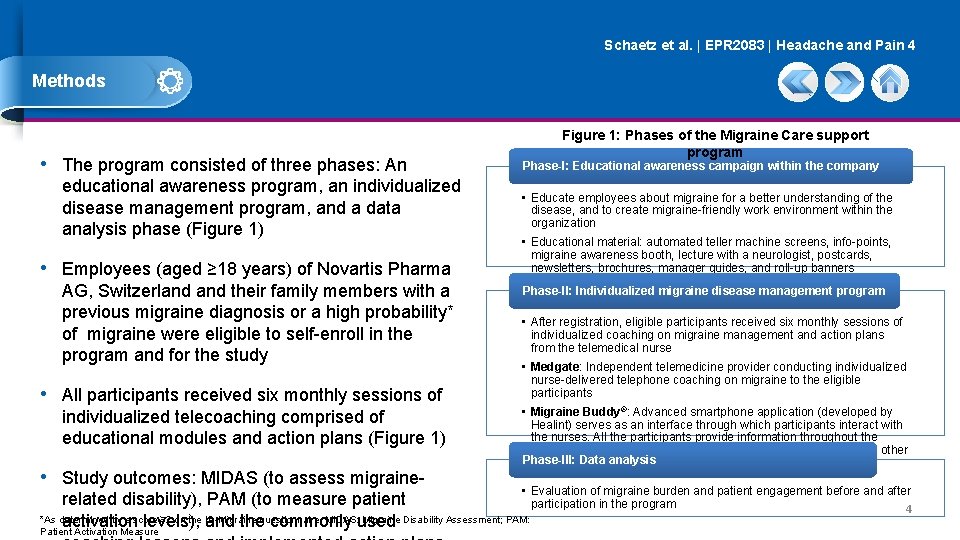
Schaetz et al. | EPR 2083 | Headache and Pain 4 Methods • The program consisted of three phases: An educational awareness program, an individualized disease management program, and a data analysis phase (Figure 1) • Employees (aged ≥ 18 years) of Novartis Pharma AG, Switzerland their family members with a previous migraine diagnosis or a high probability* of migraine were eligible to self-enroll in the program and for the study • All participants received six monthly sessions of individualized telecoaching comprised of educational modules and action plans (Figure 1) • Study outcomes: MIDAS (to assess migraine- Figure 1: Phases of the Migraine Care support program Phase-I: Educational awareness campaign within the company • Educate employees about migraine for a better understanding of the disease, and to create migraine-friendly work environment within the organization • Educational material: automated teller machine screens, info-points, migraine awareness booth, lecture with a neurologist, postcards, newsletters, brochures, manager guides, and roll-up banners Phase-II: Individualized migraine disease management program • After registration, eligible participants received six monthly sessions of individualized coaching on migraine management and action plans from the telemedical nurse • Medgate: Independent telemedicine provider conducting individualized nurse-delivered telephone coaching on migraine to the eligible participants • Migraine Buddy®: Advanced smartphone application (developed by Healint) serves as an interface through which participants interact with the nurses. All the participants provide information throughout the program in conjunction with nurses’ assessment, action plan, and other Phase-III: Data analysis educational material • Evaluation of migraine burden and patient engagement before and after related disability), PAM (to measure patient participation in the program *As determined by a score ≥ 2 on the ID-Migraine MIDAS: used Migraine Disability Assessment; PAM: activation levels), and thequestionnaire. commonly Patient Activation Measure 4
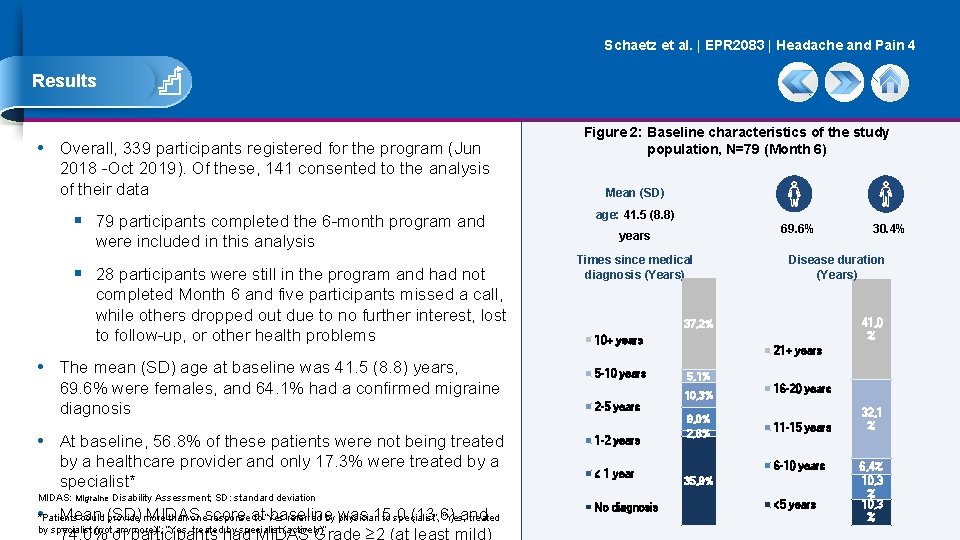
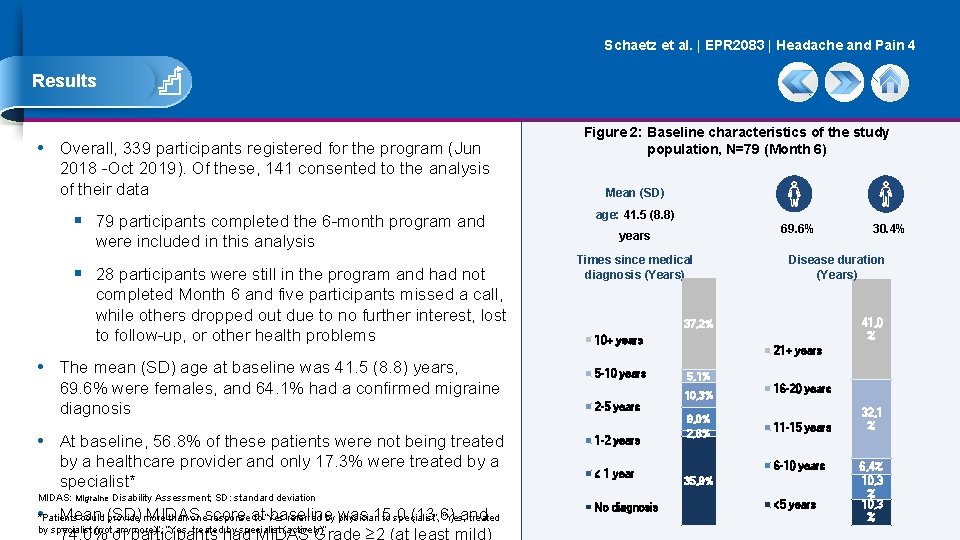
Schaetz et al. | EPR 2083 | Headache and Pain 4 Results • Overall, 339 participants registered for the program (Jun 2018 -Oct 2019). Of these, 141 consented to the analysis of their data § 79 participants completed the 6 -month program and were included in this analysis § 28 participants were still in the program and had not completed Month 6 and five participants missed a call, while others dropped out due to no further interest, lost to follow-up, or other health problems • The mean (SD) age at baseline was 41. 5 (8. 8) years, 69. 6% were females, and 64. 1% had a confirmed migraine diagnosis • At baseline, 56. 8% of these patients were not being treated by a healthcare provider and only 17. 3% were treated by a specialist* MIDAS: Migraine Disability Assessment; SD: standard deviation • *Patients Mean MIDAS baseline was 15. 0 (13. 6) and could (SD) provide more than onescore responseat to “Yes referred by physician to specialist”, “Yes, treated by specialist (not anymore)”, “Yes, treated by specialist (actively)” Figure 2: Baseline characteristics of the study population, N=79 (Month 6) Mean (SD) age: 41. 5 (8. 8) 69. 6% years Times since medical diagnosis (Years) Disease duration (Years) 41, 0 % 37, 2% 10+ years 5 -10 years 2 -5 years 1 -2 years ≤ 1 year No diagnosis 30. 4% 21+ years 5, 1% 10, 3% 9, 0% 2, 6% 16 -20 years 11 -15 years 6 -10 years 35, 9% <5 years 32, 1 % 6, 4% 10, 3 %
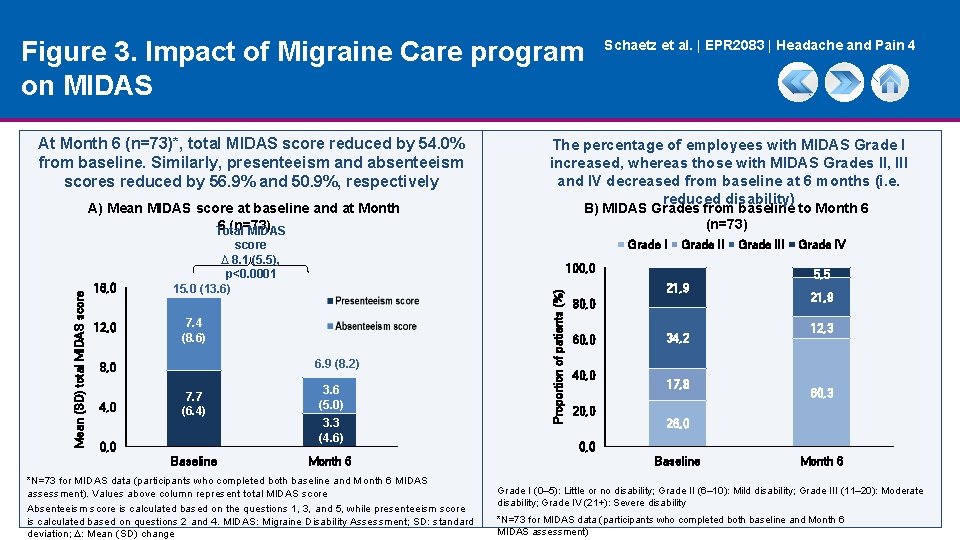
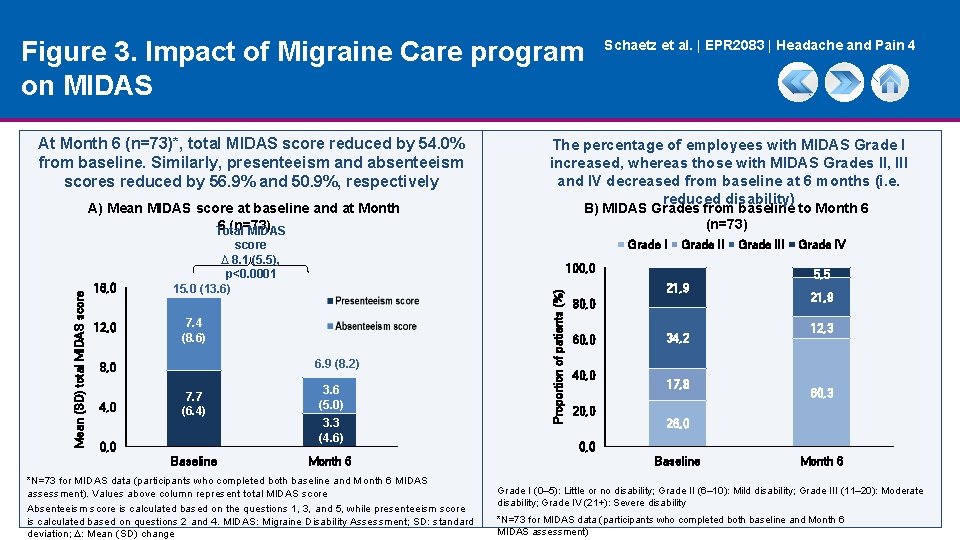
Figure 3. Impact of Migraine Care program on MIDAS At Month 6 (n=73)*, total MIDAS score reduced by 54. 0% from baseline. Similarly, presenteeism and absenteeism scores reduced by 56. 9% and 50. 9%, respectively 16, 0 12, 0 4, 0 6. 9 (8. 2) 0, 0 Baseline Grade II 100, 0 7. 4 (8. 6) 7. 7 (6. 4) B) MIDAS Grades from baseline to Month 6 (n=73) Grade I score ∆ 8. 1 (5. 5), p<0. 0001 15. 0 (13. 6) 8, 0 The percentage of employees with MIDAS Grade I increased, whereas those with MIDAS Grades II, III and IV decreased from baseline at 6 months (i. e. reduced disability) 3. 6 (5. 0) 3. 3 (4. 6) Month 6 *N=73 for MIDAS data (participants who completed both baseline and Month 6 MIDAS assessment). Values above column represent total MIDAS score Absenteeism score is calculated based on the questions 1, 3, and 5, while presenteeism score is calculated based on questions 2 and 4. MIDAS: Migraine Disability Assessment; SD: standard deviation; ∆: Mean (SD) change Proportion of patients (%) Mean (SD) total MIDAS score A) Mean MIDAS score at baseline and at Month 6 (n=73) Total MIDAS Schaetz et al. | EPR 2083 | Headache and Pain 4 80, 0 40, 0 20, 0 Grade IV 5, 5 21, 9 60, 0 Grade III 34, 2 17, 8 21, 9 12, 3 60, 3 26, 0 0, 0 Baseline Month 6 Grade I (0– 5): Little or no disability; Grade II (6– 10): Mild disability; Grade III (11– 20): Moderate disability; Grade IV (21+): Severe disability *N=73 for MIDAS data (participants who completed both baseline and Month 6 MIDAS assessment)

Figure 4. Impact of Migraine Care program on PAM Schaetz et al. | EPR 2083 | Headache and Pain 4 At Month 6 (n=78), the mean (SD) PAM score significantly improved by 5. 8 (1. 9) points, p=0∙ 0027 vs. baseline At Month 6, more than 90% of participants were activated# (PAM levels 3 and 4), while none had poor activation (PAM level 1) A) Mean PAM score at baseline through Month 6 (n=78) B) PAM levels from baseline to Month 6 (n=78) ∆ 5. 8 (1. 9), p=0. 0027 Level 1 60 40 63. 8 (10. 9) 69. 6 (12. 8) 20 90 Level 3 Level 4 0 PAM: Patient Activation Measure; SD: standard deviation; ∆: Mean (SD) change *N=78 for PAM (participants who completed both baseline and Month 6 PAM assessment) 33, 3 70 60 50 66, 7 40 59, 0 30 20 0 Month 6 15, 4 80 10 Baseline Level 2 100 Proportion of patients (%) Mean (SD) PAM scores 80 11, 5 6, 4 7, 7 Baseline Month 6 PAM Levels: Level 1 (0∙ 0– 47∙ 0): Person does not yet understand their role in healthcare; Level 2 (47∙ 1– 55∙ 1): Person does not yet have the knowledge and confidence to take action; Level 3 (55∙ 2– 72∙ 4): Person is beginning to engage in positive health behaviors; Level 4 (72∙ 5– 100): Person is proactive and engaged in recommended health behaviors. #Patient activation refers to patient’s comprehension of their role in managing their own health
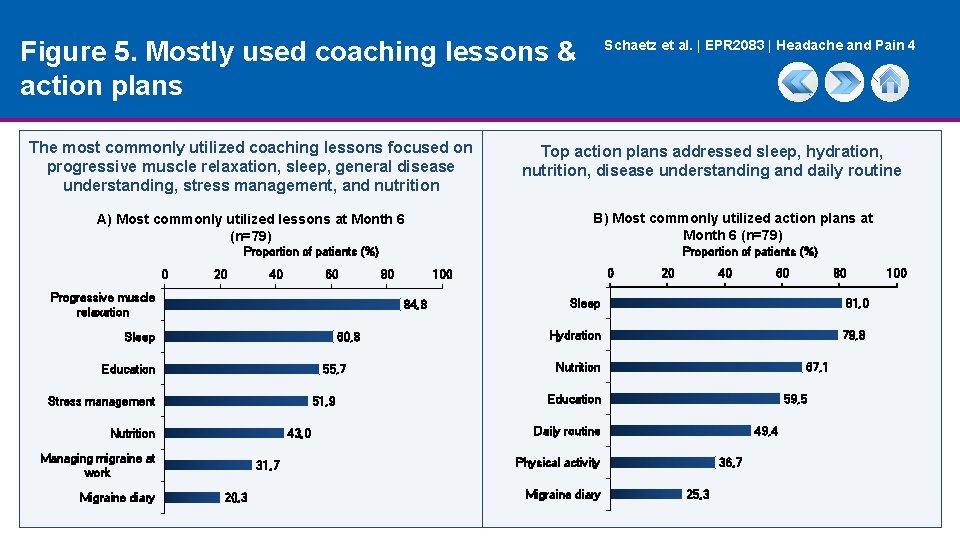
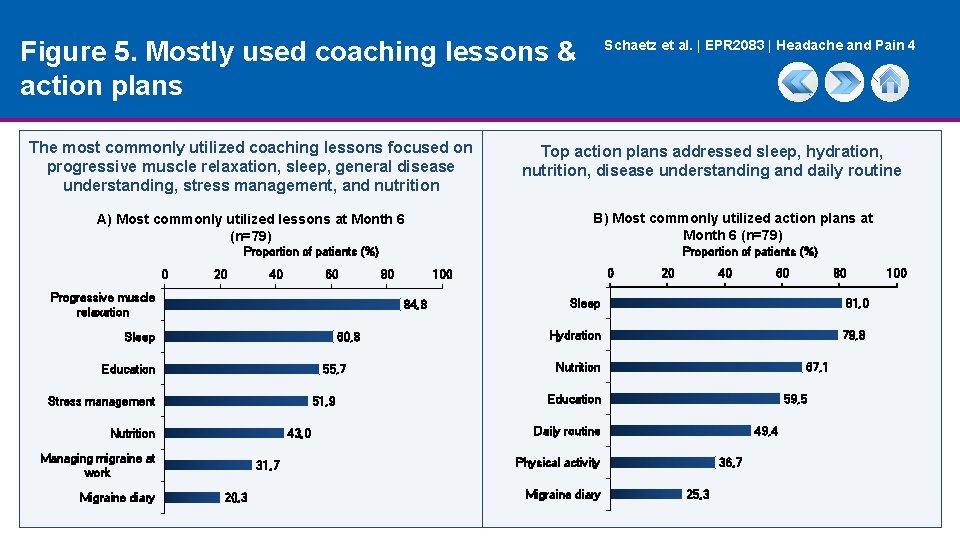
Figure 5. Mostly used coaching lessons & action plans The most commonly utilized coaching lessons focused on progressive muscle relaxation, sleep, general disease understanding, stress management, and nutrition Schaetz et al. | EPR 2083 | Headache and Pain 4 Top action plans addressed sleep, hydration, nutrition, disease understanding and daily routine B) Most commonly utilized action plans at Month 6 (n=79) A) Most commonly utilized lessons at Month 6 (n=79) Proportion of patients (%) 0 20 40 60 Progressive muscle relaxation 80 60, 8 Education 55, 7 Stress management 51, 9 Nutrition 43, 0 Managing migraine at work 31, 7 20, 3 0 100 84, 8 Sleep Migraine diary Proportion of patients (%) 20 40 60 80 Sleep 81, 0 Hydration 79, 8 Nutrition 67, 1 Education 59, 5 Daily routine 49, 4 Physical activity Migraine diary 36, 7 25, 3 100
Schaetz et al. | EPR 2083 | Headache and Pain 4 Conclusions • The results demonstrate that an employer-sponsored disease education and management program which empowers the individual to leverage all medical and lifestyle options can significantly decrease migraine-related disability, increase productivity, and promote patient activation measures • In addition, the systematic inclusion of migraine management to corporate well-being programs would be of significant benefit to the impacted individuals, companies and ultimately societies 9