Prenatal development is divided into three main Periods
















- Slides: 24
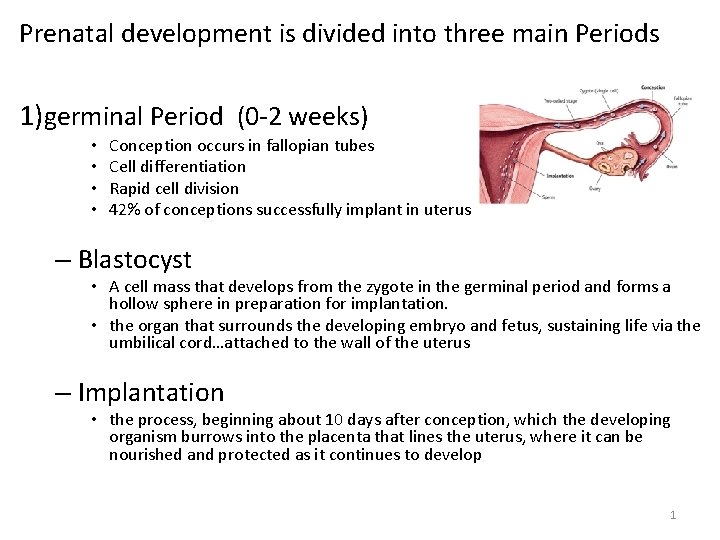
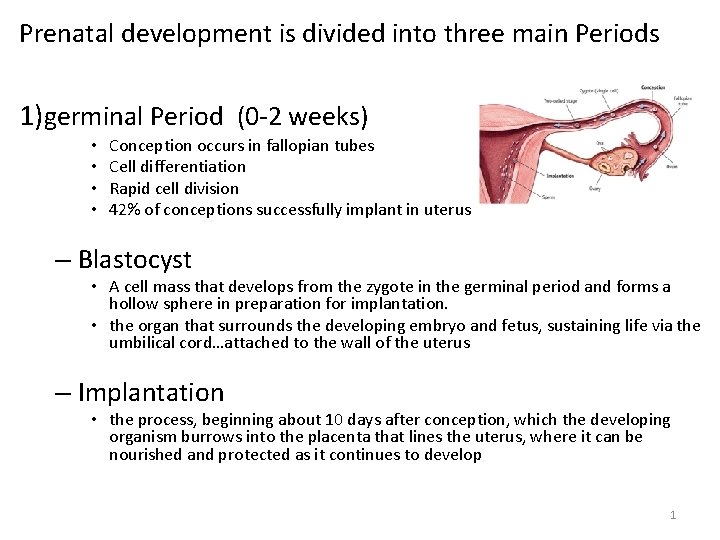
Prenatal development is divided into three main Periods 1)germinal Period (0 -2 weeks) • • Conception occurs in fallopian tubes Cell differentiation Rapid cell division 42% of conceptions successfully implant in uterus – Blastocyst • A cell mass that develops from the zygote in the germinal period and forms a hollow sphere in preparation for implantation. • the organ that surrounds the developing embryo and fetus, sustaining life via the umbilical cord…attached to the wall of the uterus – Implantation • the process, beginning about 10 days after conception, which the developing organism burrows into the placenta that lines the uterus, where it can be nourished and protected as it continues to develop 1
2) Embryo: from the third through the eighth week • major organs develop • at eight weeks, organism is less than 2˝ long 3) Fetus: From the Ninth Week Until Birth • Sex organs develop • Brain development is significant • Age of viability occurs around 22 weeks – The Third Month • • the fetus has all its body parts weighs approximately 3 ounces, about 3 inches long growth is rapid fetus is too small survive outside of the womb 2

• The Middle Three Months: Preparing to Survive – in the fourth, fifth and sixth months the heartbeat becomes stronger – the cardiovascular system more active – the brain increases about six times in size – Digestive and excretory systems develop • age of viability – twenty-two weeks after conception a fetus can survive outside the mother’s uterus if specialized medical care is available 3

• The Final Three Months: From Viability to Full Term – Viability • life outside the womb is possible • born in the seventh month requires intensive hospital care and life-support systems • difference between preterm and newborn is the maturation of neurological, respiratory, cardiovascular systems • Brain development in the cortex 4

Risk Reduction • toxins, illnesses and experiences can harm a developing person before birth – teratology • a science of risk analysis, the study of birth defects – teratogens • Agents and conditions that can impair prenatal development and result in birth defects and death. – behavioral teratogens • Agents and conditions that can harm the prenatal brain, impairing the future child’s intellectual and emotional functioning 5

Risk Reduction • Determining Risk – risk analysis • the science of weighing the potential effects of a particular event, substance, or experience to determine the likelihood of harm • Timing of Exposure – critical period • In prenatal development, the time when a particular organ or other body part of the embryo or fetus is most susceptible to damage by teratogens 6

Risk Reduction • Amount of Exposure – Threshold effect • a situation in which a certain teratogen is relatively harmless in small doses but becomes harmful once exposure reaches a certain level (the threshold) – Interaction effect • the result of a combination of teratogens. Sometimes risk is greatly magnified when an embryo or fetus is exposed to more than one teratogen at the same time 7

8
Genetic Vulnerability • Developing organisms genes determine if a teratogen will have an effect. • Dizygotic twins experience different effects. • Some nations have increased rates of some defects and decreased rates of others. • Males are at greater risk 9

Risk Reduction • Protective Measures • Benefits of Prenatal Care 10

Method used to make Prenatal Genetic Diagnoses • • • Ultrasound Chorionic Villus Sampling Alpha Fetoprotein Screen Amniocentesis Genetic Counseling

Ultrasound • Sound wave echoes are used to form a live video image of a fetus • Can be used for diagnosis of birth defects • Very safe Tim Brown/Getty Images

Chorionic Villus Sampling (CVS) • Conducted at 9 -12 weeks gestation • Needle is inserted • Fetal cells are removed and tested for various genetic disorders

Alpha Fetoprotein Detection • Conducted at 16 -18 weeks gestation • Mother’s blood is assayed for AFP levels – high levels indicate possible neural tube defects – low levels indicate possible chromosomal abnormalities

Amniocentesis • Conducted at 15 -19 weeks gestation • Needle is inserted into abdomen • Fetal skin cells are removed and assayed for genetic abnormalities • Low risk

Genetic Counseling • Birth defects – Occur in 1/33 births – Are the leading cause of infant death • Genetic counselors – Help determine risk – Provide counseling for families with an infant born with genetic problems
Genetic Counseling • Recommended for – Parents of children with genetic disorders – Parents with a known genetic disorder – Women who have repeatedly miscarried – Older pregnant women – Couples of certain ancestry/ethnicities – Couples who are related to each other

Normal Uncomplicated Birth • The Newborn’s First Minutes 18
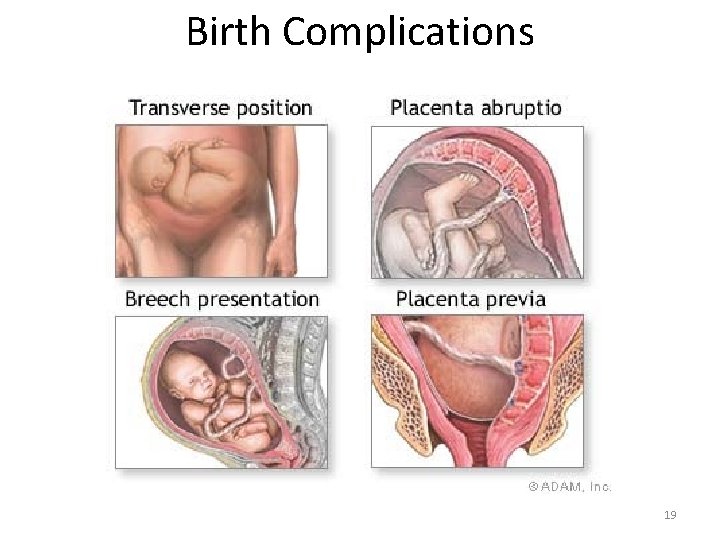
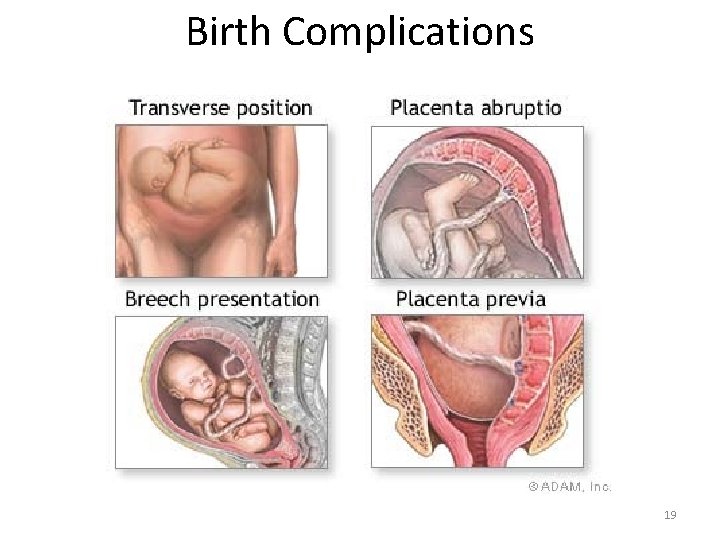
Birth Complications 19

The Birth Process • The Newborn’s First Minutes – Apgar scale • a quick assessment of a newborn’s body functioning. – – – color heart rate reflexes muscle tone respiratory effort 20
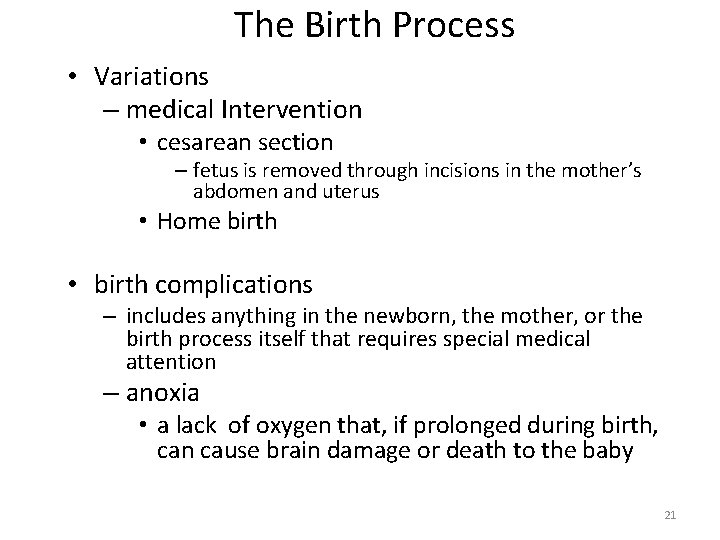
The Birth Process • Variations – medical Intervention • cesarean section – fetus is removed through incisions in the mother’s abdomen and uterus • Home birth • birth complications – includes anything in the newborn, the mother, or the birth process itself that requires special medical attention – anoxia • a lack of oxygen that, if prolonged during birth, can cause brain damage or death to the baby 21

The Birth Process • Birthweight – the average weight of a newborn is 7½ lbs. (normal range is 5 ½ to 9 pounds) • • LBW is considered less than 5½ lbs. VLBW is considered less than 3 lbs. 5 oz. ELBW is considered less than 2 lbs. 3 oz. preterm is less than 35 weeks (usually LBW, but not always) – lifestyle choices • e. g. , cigarette smoking accounts for 25% of LBW births worldwide! – maternal malnutrition – multiple births – prescription drugs – maternal obesity 22
The Birth Process • Some babies are born small for their gestational age (SGA) – Ex. 5 lb. Newborn – These babies gained weight too slowly during the prenatal period – More concerning than a underweight pre-term baby – Failure to thrive – Causes (problems with placenta and umbilical cord, maternal illness and maternal drug use) 23
The Birth Process • Social Support • Mother’s Role • Help from fathers • Postpartum Depression – 8 -15% of women experience postpartum depression, a sense of inadequacy and sadness after birth. – includes irritability, sleep and eating disruptions, sadness, feeling overwhelmed and inadequate as a mom, no interest or overly worried about baby. 24