Prediction of maternal nearmiss in placenta previa a

- Slides: 10
Prediction of maternal nearmiss in placenta previa: a retrospective analysis from a tertiary center in Ankara, Turkey. Bora Coskun, Iltac Akkurt, Riza Dur, Mehmet Ozgur Akkurt, Seval Yilmaz Ergani, Bugra Coskun
Aim Placenta previa (PP) poses both maternal and fetal risks and its incidence has been increasing in parallel with the cesarean delivery (CD) rates. In the present study we aimed to determine the risk factors for complicated CD in placenta previa.
Methods This retrospective study was performed at Etlik Zubeyde Hanim Maternity and Women’s Health Teaching and Research Hospital during 6 -year study period. Women with total and partial PP were included. Complicated CD was identified according to modified World Health Organization (WHO) maternal near-miss criteria.
WHO near-miss criteria Coagulation and hematological dysfunction defined as transfusion of 4 and more units of red blood cells, a rapid drop in hemoglobin levels (>4 g/dl) and acute thrombocytopenia <75. 000/ml Reoperation, hysterectomy, balloon placement and uterine artery and/or hypogastric artery ligation for hemorrhage, Prolonged postoperative hospitalization (>4 days), Intra-and/or post-operative complications such as bladder, ureter, bowel injury, Renal dysfunction (creatinine >3. 5 mg/dl), Admission to intensive care unit.
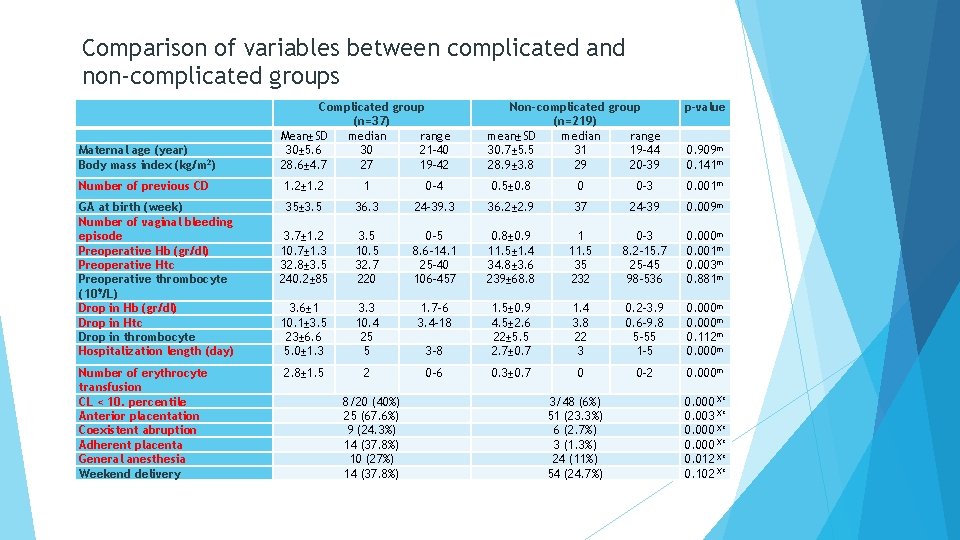
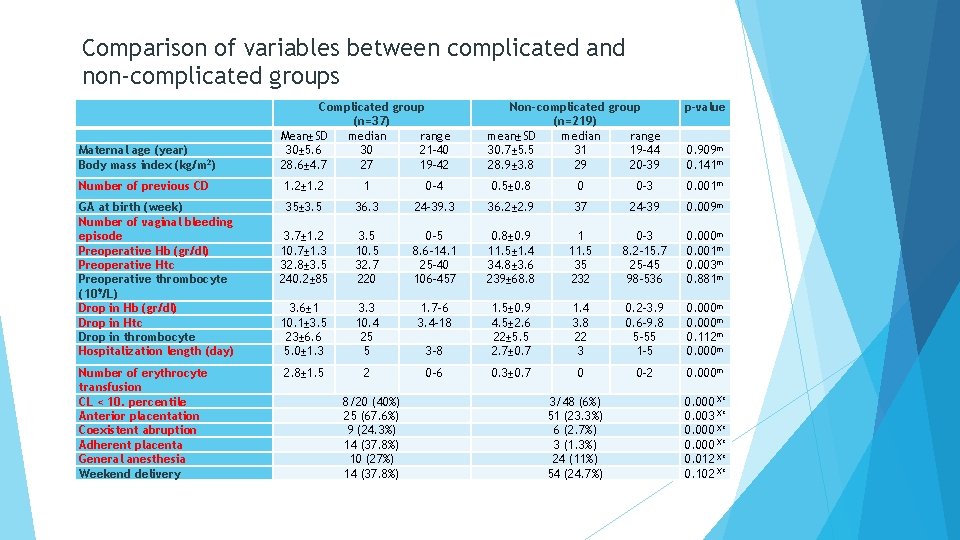
Comparison of variables between complicated and non-complicated groups Maternal age (year) Body mass index (kg/m 2) Complicated group (n=37) Mean±SD median range 30± 5. 6 30 21 -40 28. 6± 4. 7 27 19 -42 Number of previous CD 1. 2± 1. 2 1 0 -4 0. 5± 0. 8 0 0 -3 0. 001 m 35± 3. 5 3. 7± 1. 2 10. 7± 1. 3 32. 8± 3. 5 240. 2± 85 36. 3 3. 5 10. 5 32. 7 220 24 -39. 3 0 -5 8. 6 -14. 1 25 -40 106 -457 36. 2± 2. 9 0. 8± 0. 9 11. 5± 1. 4 34. 8± 3. 6 239± 68. 8 37 1 11. 5 35 232 24 -39 0 -3 8. 2 -15. 7 25 -45 98 -536 0. 009 m 0. 000 m 0. 001 m 0. 003 m 0. 881 m 3. 6± 1 10. 1± 3. 5 23± 6. 6 5. 0± 1. 3 3. 3 10. 4 25 5 1. 7 -6 3. 4 -18 3 -8 1. 5± 0. 9 4. 5± 2. 6 22± 5. 5 2. 7± 0. 7 1. 4 3. 8 22 3 0. 2 -3. 9 0. 6 -9. 8 5 -55 1 -5 0. 000 m 0. 112 m 0. 000 m 2. 8± 1. 5 2 0 -6 0. 3± 0. 7 0 0 -2 0. 000 m GA at birth (week) Number of vaginal bleeding episode Preoperative Hb (gr/dl) Preoperative Htc Preoperative thrombocyte (109/L) Drop in Hb (gr/dl) Drop in Htc Drop in thrombocyte Hospitalization length (day) Number of erythrocyte transfusion CL < 10. percentile Anterior placentation Coexistent abruption Adherent placenta General anesthesia Weekend delivery 8/20 (40%) 25 (67. 6%) 9 (24. 3%) 14 (37. 8%) 10 (27%) 14 (37. 8%) Non-complicated group (n=219) mean±SD median range 30. 7± 5. 5 31 19 -44 28. 9± 3. 8 29 20 -39 3/48 (6%) 51 (23. 3%) 6 (2. 7%) 3 (1. 3%) 24 (11%) 54 (24. 7%) p-value 0. 909 m 0. 141 m 0. 000 X² 0. 003 X² 0. 000 X² 0. 012 X² 0. 102 X²
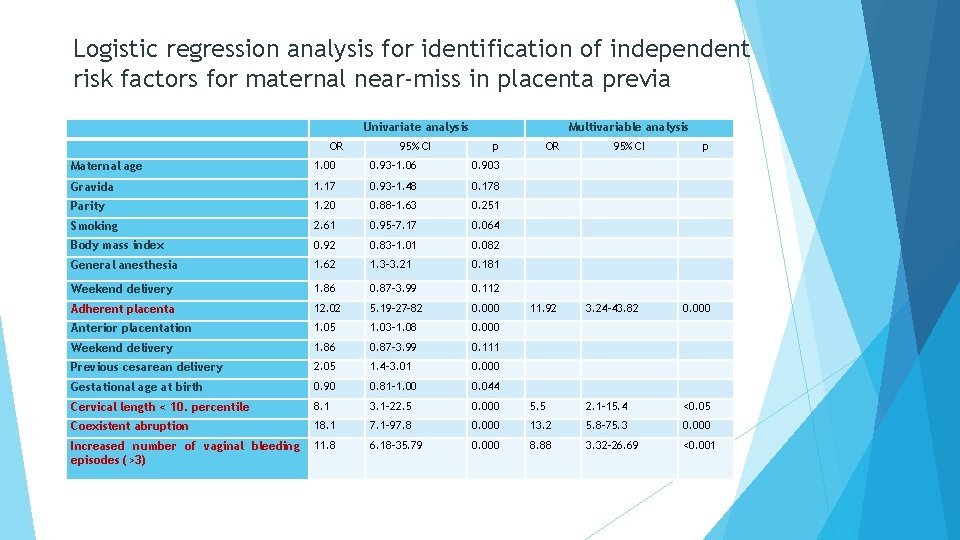
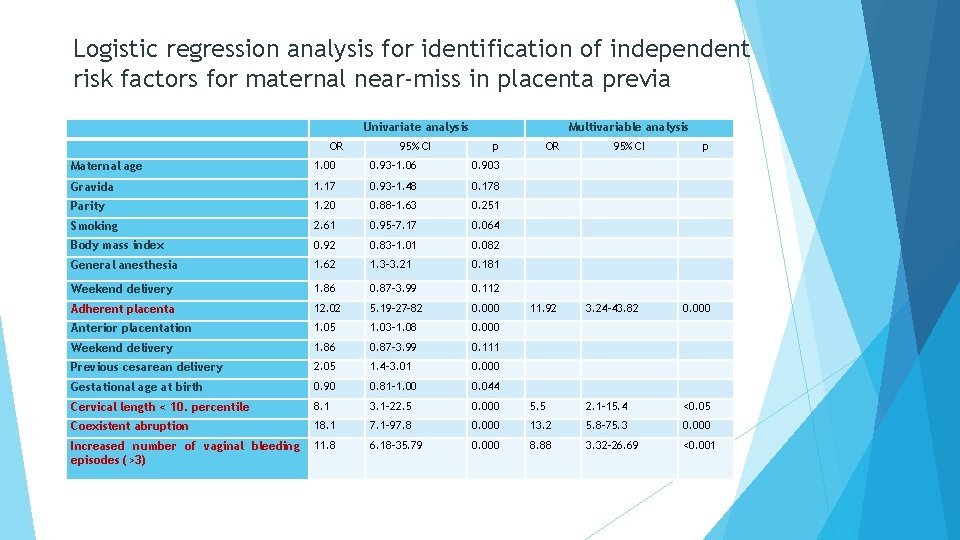
Logistic regression analysis for identification of independent risk factors for maternal near-miss in placenta previa Univariate analysis OR 95% CI Multivariable analysis p OR 95% CI p Maternal age 1. 00 0. 93 -1. 06 0. 903 Gravida 1. 17 0. 93 -1. 48 0. 178 Parity 1. 20 0. 88 -1. 63 0. 251 Smoking 2. 61 0. 95 -7. 17 0. 064 Body mass index 0. 92 0. 83 -1. 01 0. 082 General anesthesia 1. 62 1. 3 -3. 21 0. 181 Weekend delivery 1. 86 0. 87 -3. 99 0. 112 Adherent placenta 12. 02 5. 19 -27 -82 0. 000 11. 92 3. 24 -43. 82 0. 000 Anterior placentation 1. 05 1. 03 -1. 08 0. 000 Weekend delivery 1. 86 0. 87 -3. 99 0. 111 Previous cesarean delivery 2. 05 1. 4 -3. 01 0. 000 Gestational age at birth 0. 90 0. 81 -1. 00 0. 044 Cervical length < 10. percentile 8. 1 3. 1 -22. 5 0. 000 5. 5 2. 1 -15. 4 <0. 05 Coexistent abruption 18. 1 7. 1 -97. 8 0. 000 13. 2 5. 8 -75. 3 0. 000 Increased number of vaginal bleeding episodes (>3) 11. 8 6. 18 -35. 79 0. 000 8. 88 3. 32 -26. 69 <0. 001
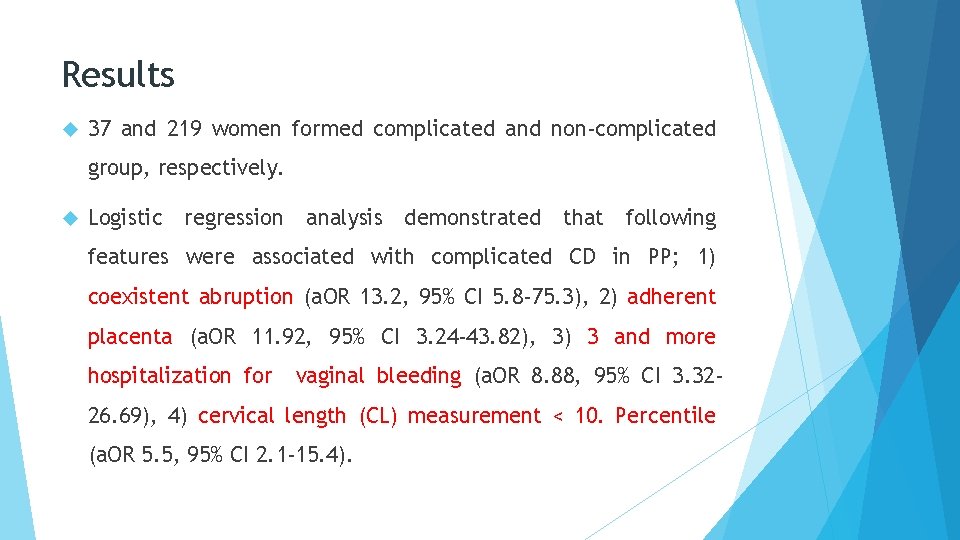
Results 37 and 219 women formed complicated and non-complicated group, respectively. Logistic regression analysis demonstrated that following features were associated with complicated CD in PP; 1) coexistent abruption (a. OR 13. 2, 95% CI 5. 8 -75. 3), 2) adherent placenta (a. OR 11. 92, 95% CI 3. 24 -43. 82), 3) 3 and more hospitalization for vaginal bleeding (a. OR 8. 88, 95% CI 3. 32 - 26. 69), 4) cervical length (CL) measurement < 10. Percentile (a. OR 5. 5, 95% CI 2. 1 -15. 4).
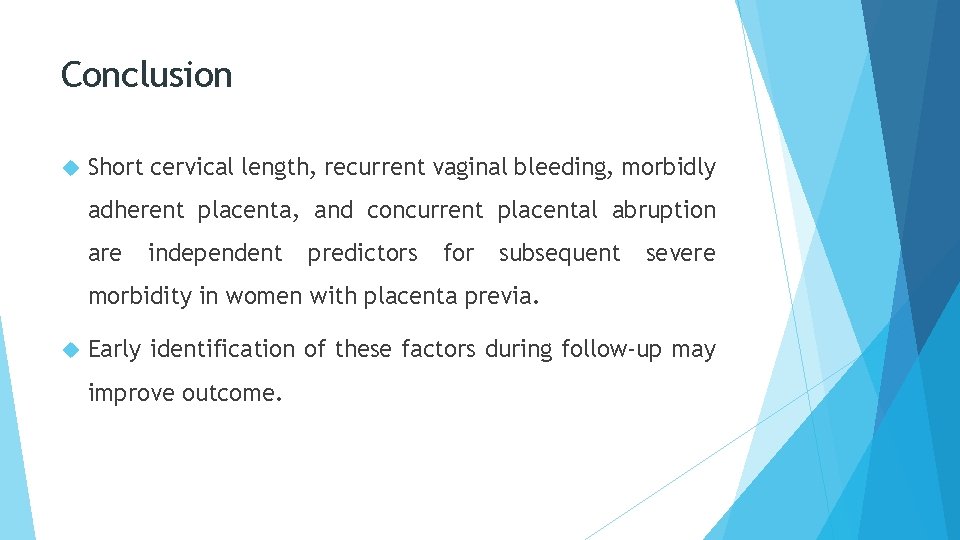
Conclusion Short cervical length, recurrent vaginal bleeding, morbidly adherent placenta, and concurrent placental abruption are independent predictors for subsequent severe morbidity in women with placenta previa. Early identification of these factors during follow-up may improve outcome.
Teşekkürler…