Parts of the Anesthetic Machine Purpose of the




- Slides: 27
Parts of the Anesthetic Machine
Purpose of the Anesthetic Machine A liquid inhalant anesthetic is vaporized into a carrier gas, and delivered to the patient via a breathing circuit. Oxygen is delivered at a controlled rate (L/min) Isoflurane is converted to a gas and given at a specific percentage Gases exhaled from the patient are scavenged OR can be re-circulated once CO 2 has been removed *Can also be used to deliver just oxygen during recovery or in an emergency*
Components of the Anesthetic Machine 1. Compressed gas supply Gas tanks, their pressure gauges, pressure reducing valves, flow meter 2. Anesthetic vaporizer Precision, out-of-circuit vaporizer is ideal (what we use) Located near the fresh gas outlet 3. Breathing circuit Unidirectional valves, breathing tubes, reservoir bag, pop-off valve, CO 2 canister, pressure manometer, negative pressure relief valve 4. Scavenging System Disposes of excess and waste anesthetic gases

PART 1: Compressed Gas Supply
Gas Cylinders Most It commonly used carrier gas is oxygen comes compressed in a metal cylinder and held under pressure- up to 2200 psi Available in various sizes “E” tanks hold 660 L of oxygen and are attached to the anesthesia machine “H” tanks hold 6900 L of oxygen and stand separate from the machine Tanks are delivered and picked up by the oxygen supply company as needed
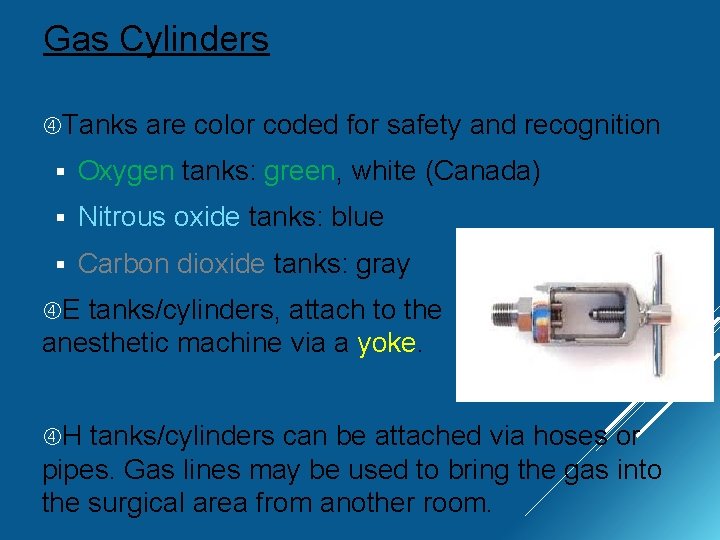
Gas Cylinders Tanks are color coded for safety and recognition § Oxygen tanks: green, white (Canada) § Nitrous oxide tanks: blue § Carbon dioxide tanks: gray E tanks/cylinders, attach to the anesthetic machine via a yoke. H tanks/cylinders can be attached via hoses or pipes. Gas lines may be used to bring the gas into the surgical area from another room.

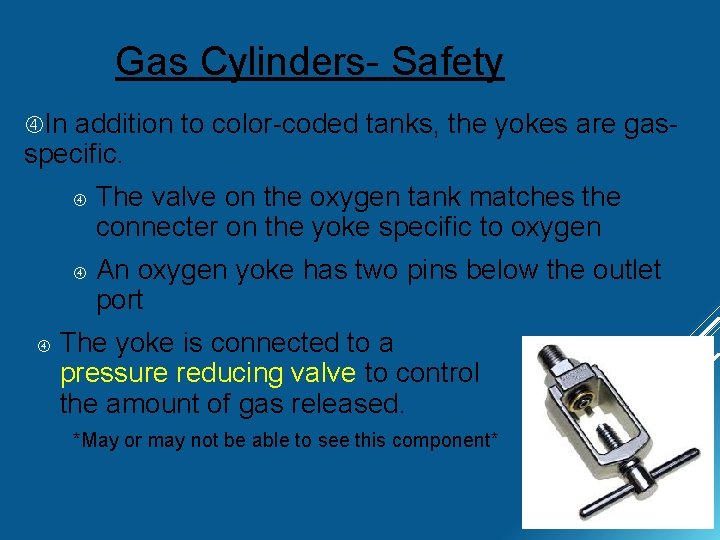
Gas Cylinders- Safety In addition to color-coded tanks, the yokes are gasspecific. The valve on the oxygen tank matches the connecter on the yoke specific to oxygen An oxygen yoke has two pins below the outlet port The yoke is connected to a pressure reducing valve to control the amount of gas released. *May or may not be able to see this component*

Gas Cylinders- Safety Combustible If gases- avoid flames and sparks! dropped, has the potential to act as a torpedo Never leave a cylinder unattended! VIDEO
Tank Pressure Gauge Display of the pressure of oxygen currently in the tank. (usually attached to yoke) Only displays when the tank is open/on To open tank: use key Only open once tank has been connected to a yoke! Gauge reads zero when tank is empty AND when tank is turned off/closed What about gas left in the machine? *Turn on O 2 and check this gauge BEFORE every anesthetic procedure
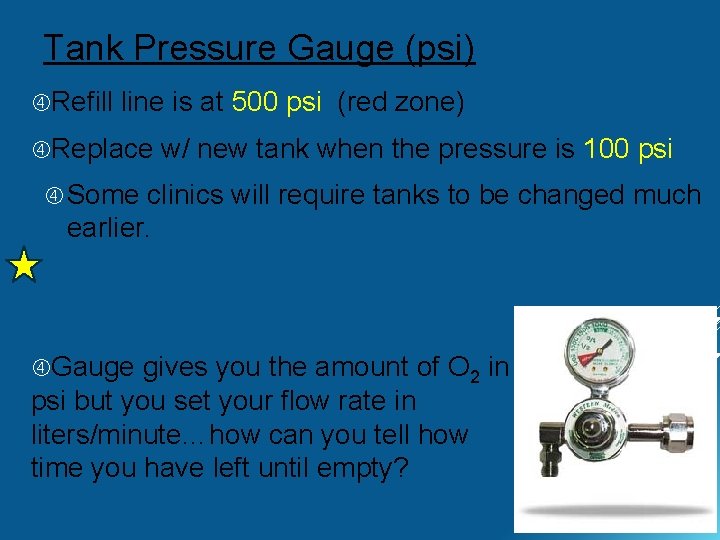
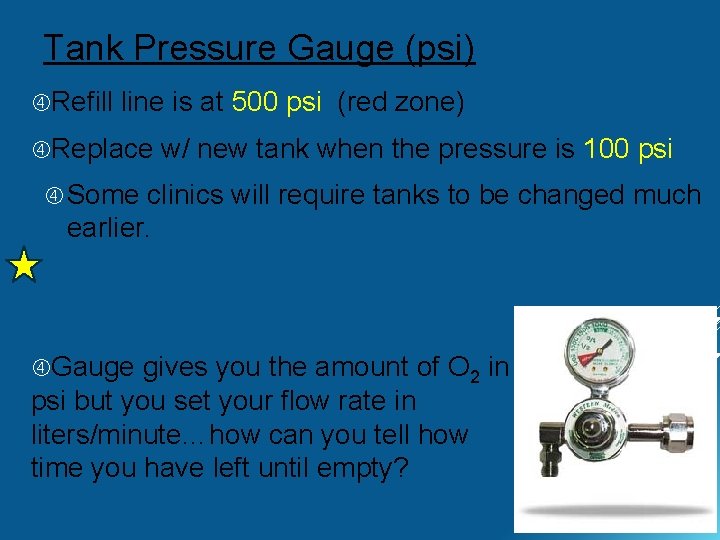
Tank Pressure Gauge (psi) Refill line is at 500 psi (red zone) Replace w/ new tank when the pressure is 100 psi Some clinics will require tanks to be changed much earlier. Gauge gives you the amount of O 2 in psi but you set your flow rate in liters/minute…how can you tell how time you have left until empty? much
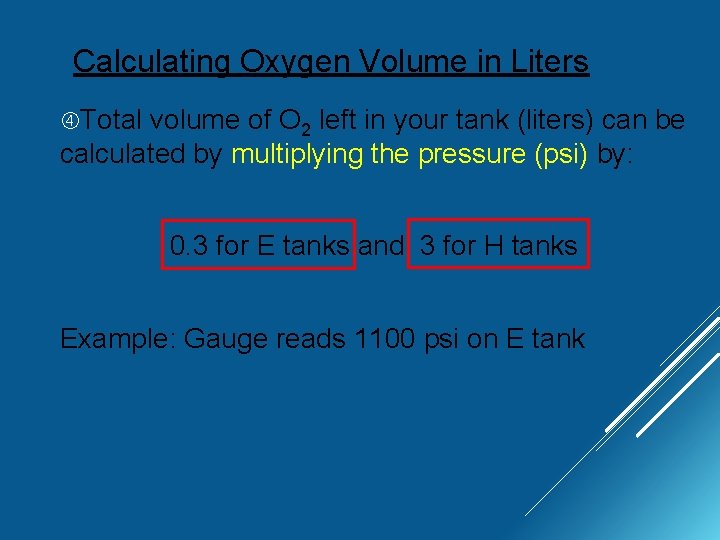
Calculating Oxygen Volume in Liters Total volume of O 2 left in your tank (liters) can be calculated by multiplying the pressure (psi) by: 0. 3 for E tanks and 3 for H tanks Example: Gauge reads 1100 psi on E tank
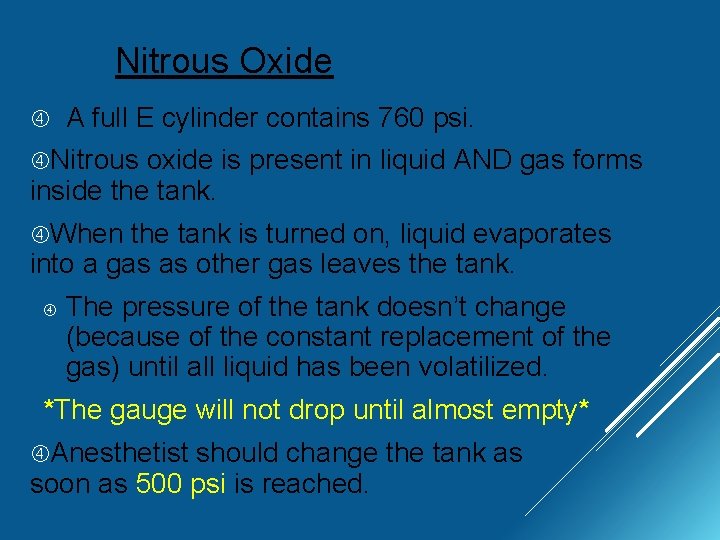
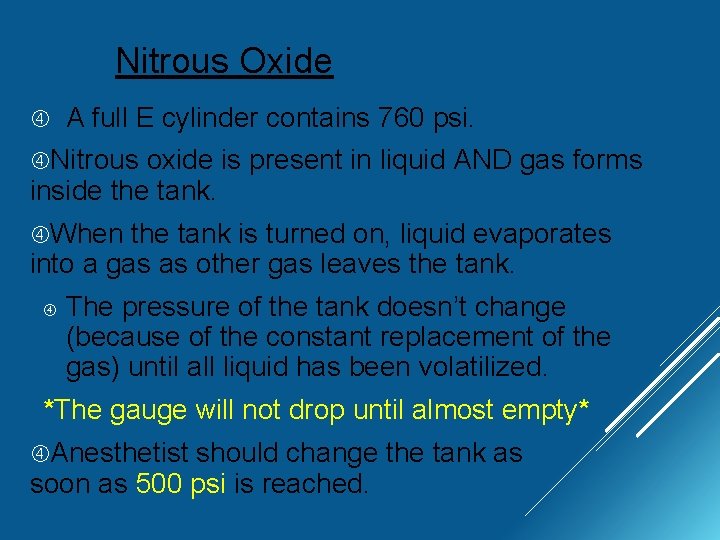
Nitrous Oxide A full E cylinder contains 760 psi. Nitrous oxide is present in liquid AND gas forms inside the tank. When the tank is turned on, liquid evaporates into a gas as other gas leaves the tank. The pressure of the tank doesn’t change (because of the constant replacement of the gas) until all liquid has been volatilized. *The gauge will not drop until almost empty* Anesthetist should change the tank as soon as 500 psi is reached.
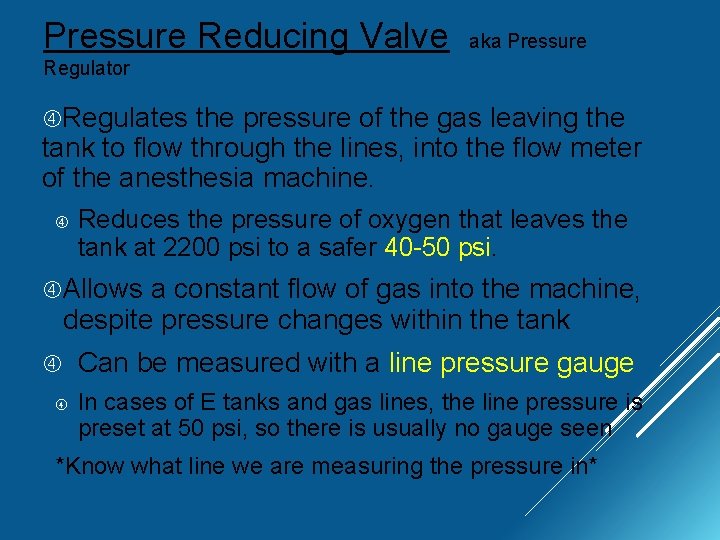
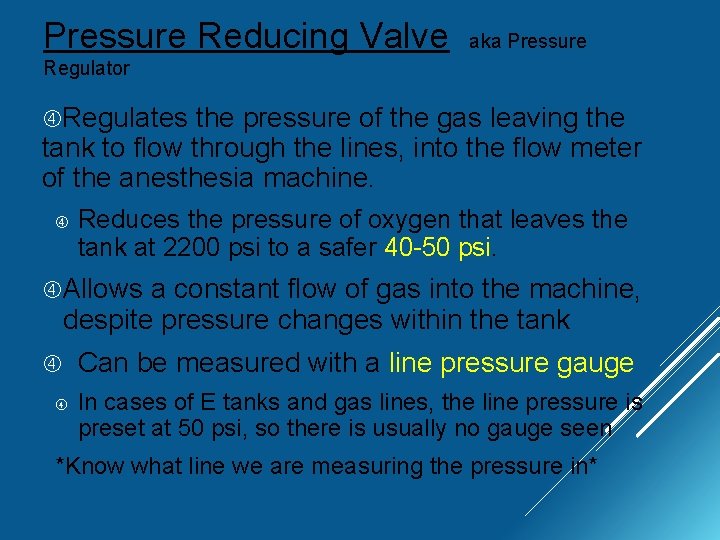
Pressure Reducing Valve aka Pressure Regulator Regulates the pressure of the gas leaving the tank to flow through the lines, into the flow meter of the anesthesia machine. Reduces the pressure of oxygen that leaves the tank at 2200 psi to a safer 40 -50 psi. Allows a constant flow of gas into the machine, despite pressure changes within the tank Can be measured with a line pressure gauge In cases of E tanks and gas lines, the line pressure is preset at 50 psi, so there is usually no gauge seen *Know what line we are measuring the pressure in*

Flow Meter Allows the flow rate of oxygen traveling through the machine to be adjusted by the anesthetist. Reduces the psi AGAIN, from 50 down to 15 psi Oxygen does not reach the patient unless this is turned on (neither does the anesthetic gas). Measured Ball in liters per minute by a ball rises in height, proportional to gas
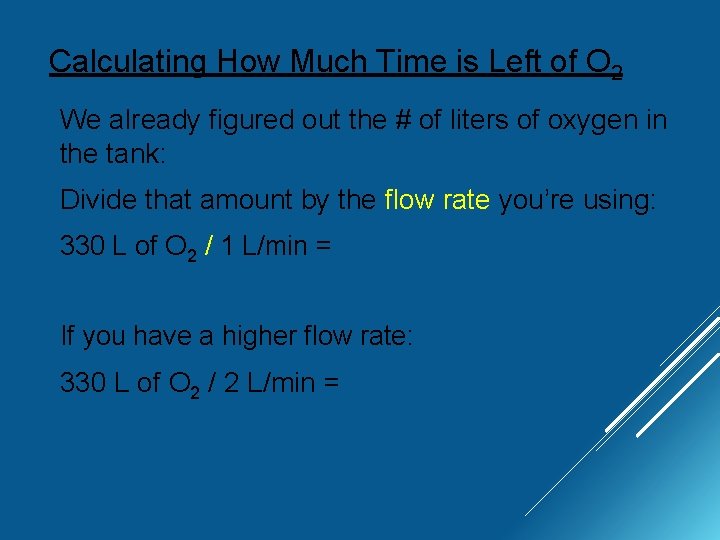
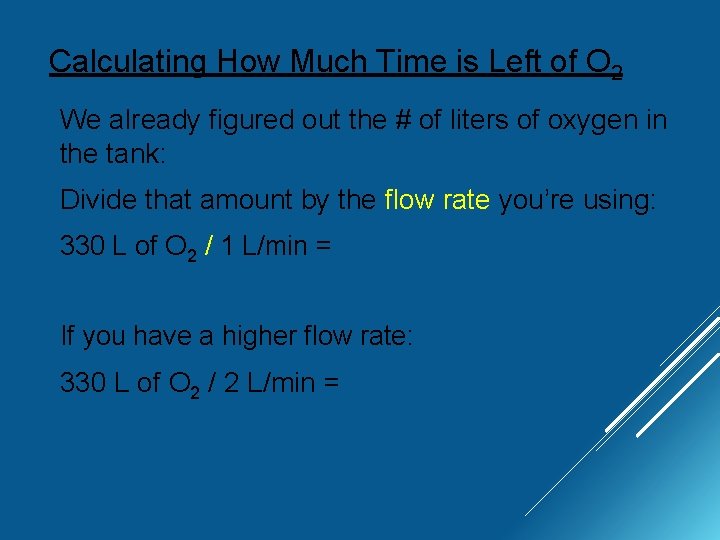
Calculating How Much Time is Left of O 2 We already figured out the # of liters of oxygen in the tank: Divide that amount by the flow rate you’re using: 330 L of O 2 / 1 L/min = If you have a higher flow rate: 330 L of O 2 / 2 L/min =
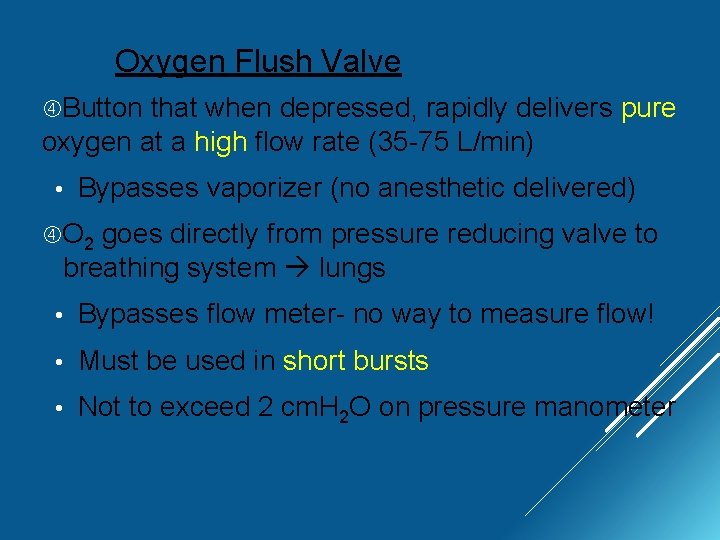
Oxygen Flush Valve Button that when depressed, rapidly delivers pure oxygen at a high flow rate (35 -75 L/min) • Bypasses vaporizer (no anesthetic delivered) O 2 goes directly from pressure reducing valve to breathing system lungs • Bypasses flow meter- no way to measure flow! • Must be used in short bursts • Not to exceed 2 cm. H 2 O on pressure manometer
Oxygen Flush Valve Seems dangerous… Ø When would we want to use this? 1. To dilute anesthetic in lines in emergency 2. To dilute anesthetic in lines on recovery 3. To fill reservoir bag (to give a breath)
PART 2: Anesthetic Vaporizer Next Now stop as oxygen travels from the flow meter that the gas is in the machine, it’s job is to mix with the liquid anesthetic and be delivered to the patient.
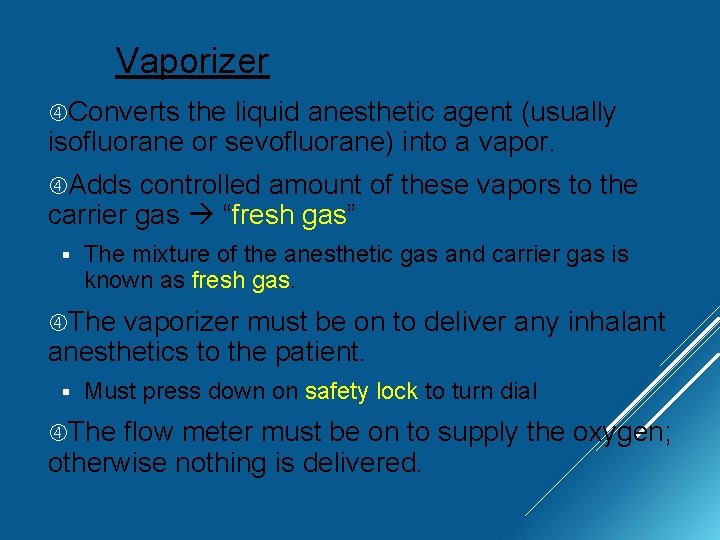
Vaporizer Converts the liquid anesthetic agent (usually isofluorane or sevofluorane) into a vapor. Adds controlled amount of these vapors to the carrier gas “fresh gas” § The mixture of the anesthetic gas and carrier gas is known as fresh gas. The vaporizer must be on to deliver any inhalant anesthetics to the patient. § Must press down on safety lock to turn dial The flow meter must be on to supply the oxygen; otherwise nothing is delivered.
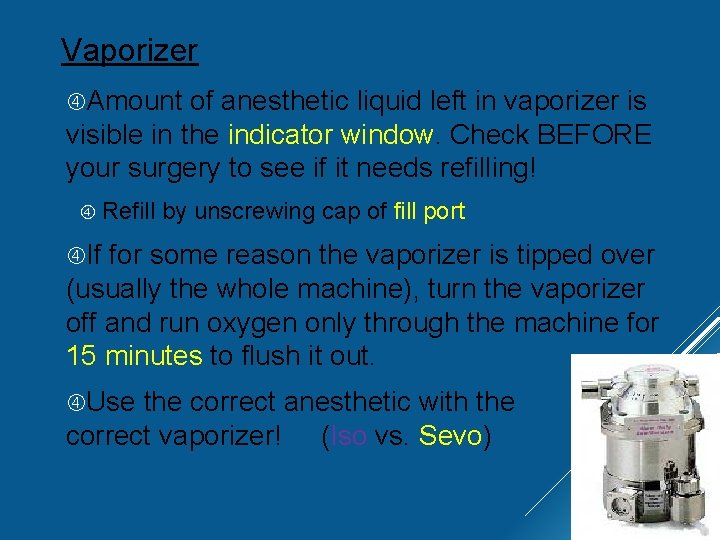
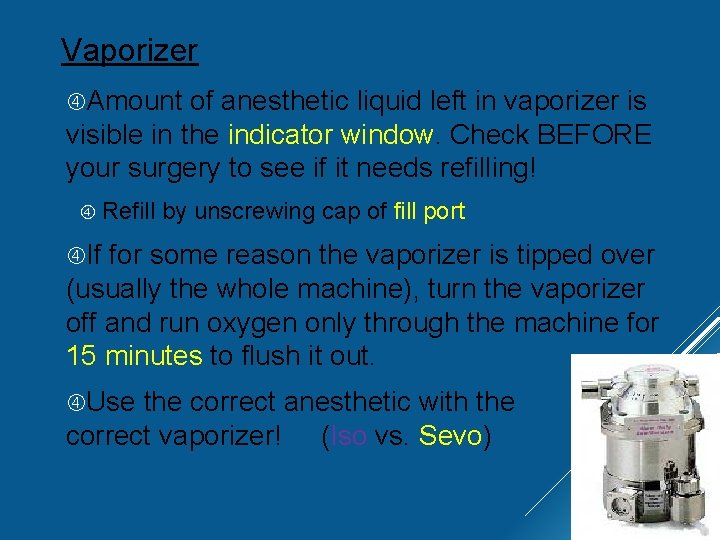
Vaporizer Amount of anesthetic liquid left in vaporizer is visible in the indicator window. Check BEFORE your surgery to see if it needs refilling! Refill by unscrewing cap of fill port If for some reason the vaporizer is tipped over (usually the whole machine), turn the vaporizer off and run oxygen only through the machine for 15 minutes to flush it out. Use the correct anesthetic with the correct vaporizer! (Iso vs. Sevo)
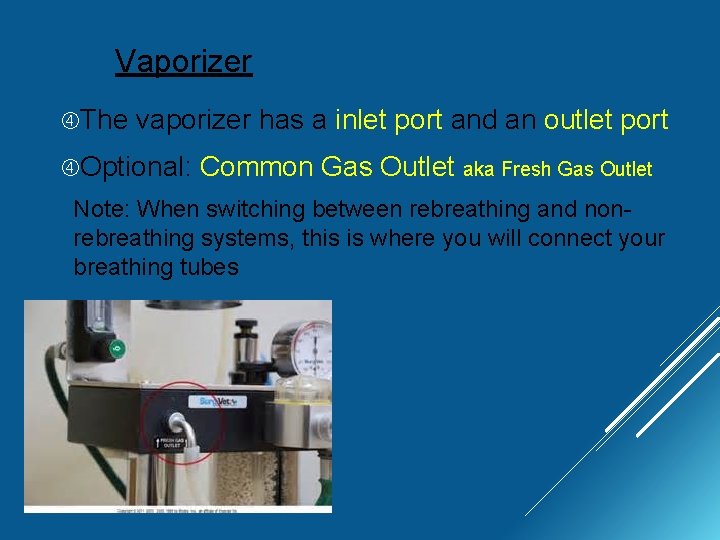
Vaporizer The vaporizer has a inlet port and an outlet port Optional: Common Gas Outlet aka Fresh Gas Outlet Note: When switching between rebreathing and nonrebreathing systems, this is where you will connect your breathing tubes
Precision vs. Non Precision Non-precision vaporizers are simple, cheaper, and are typically used for anesthetics with low vapor pressure such as methoxyfluorane Non-precision vaporizers are located within the breathing circuit (VIC) Gas flows from the flow meter into the breathing tubes, which contain the vaporizer *They are no longer commonly used; we will focus on precision vaporizers
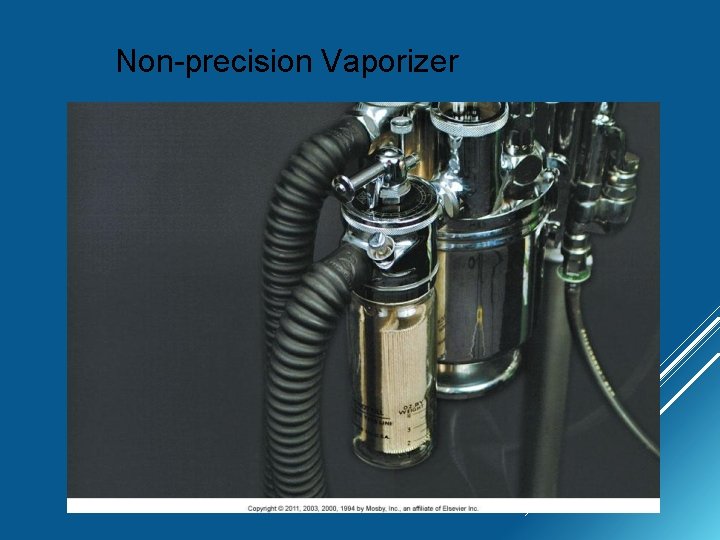
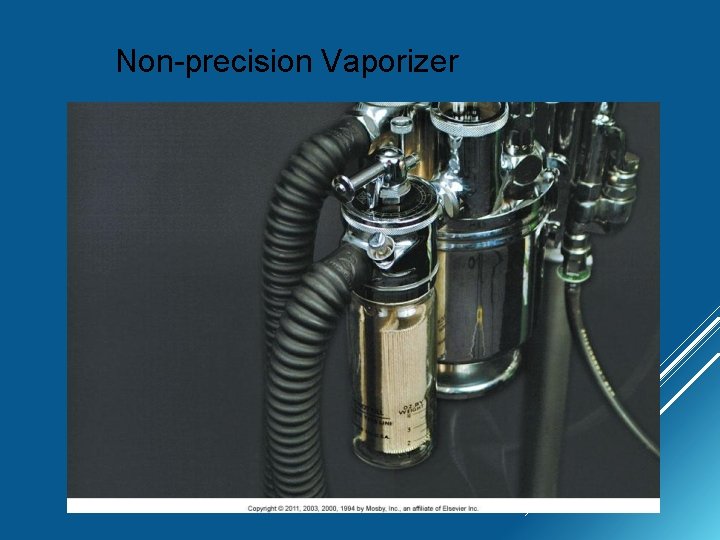
Non-precision Vaporizer
Precision vs. Non Precision vaporizers deliver a precise, controlled amount of anesthetic to the patient Expressed as a % which is chosen based on an anesthetic’s MAC and the patient’s requirements Commonly used anesthetics can reach concentrations as high as 30% + if they are not controlled (vapor pressure) Precision vaporizers are located outside of the breathing circuit (VOC) Newer models compensate for the factors that determine the concentration of anesthetic delivered (other than what you set it to). Ex. Temperature, respiratory rate, back pressure
Precision Vaporizer Compensation Made to deliver a precise concentration of anesthetic; non-precision vaporizers do not Factors that are compensated for: Temperature changes: Volatile anesthetics vaporize more rapidly at high temperatures If not compensated for: hot room = higher anesthetic output Carrier gas flow rates and respiratory rate effect amount of anesthetic delivered If not compensated: high L/min or tachypnea = higher anesthetic output
Precision Vaporizer Compensation Factors that are compensated for: Back pressure: Squeezing the reservoir bag while bagging your patient exerts pressure on the vaporizer outlet port If not compensated for: providing a breath = providing a higher anesthetic concentration
 Anesthetic machine parts
Anesthetic machine parts Anesthetic, pungent, sweet
Anesthetic, pungent, sweet Purpose sentence
Purpose sentence Specific purpose statements
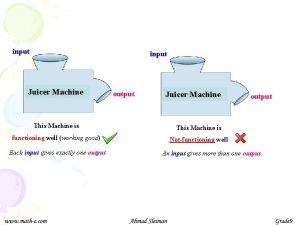
Specific purpose statements Purpose of simple machine
Purpose of simple machine Special purpose machine bir
Special purpose machine bir Finite state machine vending machine example
Finite state machine vending machine example Mealy or moore machine
Mealy or moore machine Moore machine
Moore machine Chapter 10 energy, work and simple machines answer key
Chapter 10 energy, work and simple machines answer key It is a movable plate that covers the shuttle
It is a movable plate that covers the shuttle Diathermy machine diagram
Diathermy machine diagram Foot operated suction machine use
Foot operated suction machine use Phototherapy function
Phototherapy function Isometric projection in c
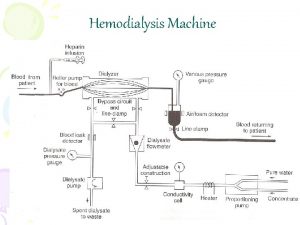
Isometric projection in c Dialysis machine parts and functions
Dialysis machine parts and functions Curapulse
Curapulse Radial drilling machine working principle
Radial drilling machine working principle Parts of portable grinder
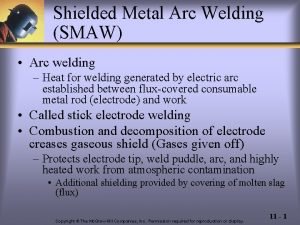
Parts of portable grinder Principle of smaw
Principle of smaw Label sewing machine parts
Label sewing machine parts In shaper the job is kept
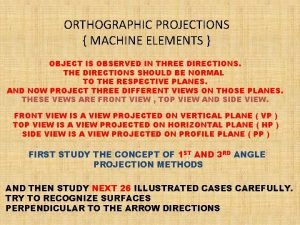
In shaper the job is kept Orthographic projection of machine parts
Orthographic projection of machine parts Hemodialysis machine parts and function
Hemodialysis machine parts and function Pressing process in garment industry
Pressing process in garment industry Iabp machine parts
Iabp machine parts Reaming process
Reaming process Scotsman ice machine parts distributor near me
Scotsman ice machine parts distributor near me