Overview of OHICs Care Transformation Payment Reform Initiatives
- Slides: 7
Overview of OHIC’s Care Transformation & Payment Reform Initiatives KATHLEEN C. HITTNER, MD. HEALTH INSURANCE COMMISSIONER NOVEMBER 12 T H , 2015
Agenda §Policy Objectives of the Affordability Standards §Strategy 1: Care Transformation §Strategy 2: Payment Reform §Questions
Policy Objectives The key objective of OHIC’s Affordability Standards is to make health insurance coverage more affordable for Rhode Islanders by driving increased efficiency and quality in medical care delivery. Two mutually reinforcing strategies to achieve this objective are to transform the way care is delivered and reform how care is reimbursed.
Care Transformation Transforming the Delivery System Initiatives to foster a delivery system capable of managing population health and total cost of care. • Strengthen primary care. • Expand PCMH to reach 80% of primary care providers by 2019. • Reduce barriers to practice transformation. • Build connections between primary care, specialists, hospitals and post-acute care providers. • Make data and analytics accessible and actionable.
Payment Reform Paying for Value, Not Volume Initiatives to align health care payment with incentives for efficiency and quality of care. • Drive health care payment to alternative payment models that evaluate provider performance on cost and quality. • Convene stakeholders to plan strategies and develop recommendations around expansion of alternative payment models.
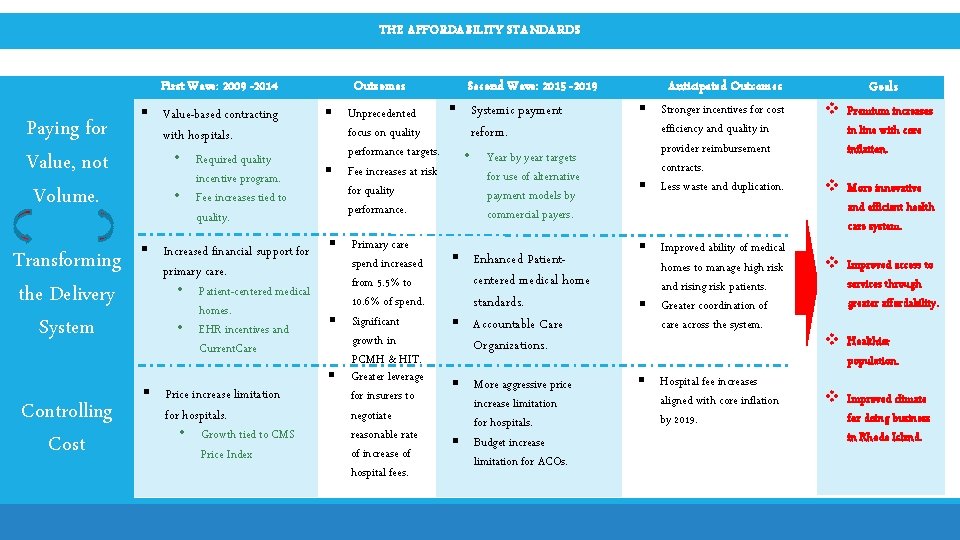
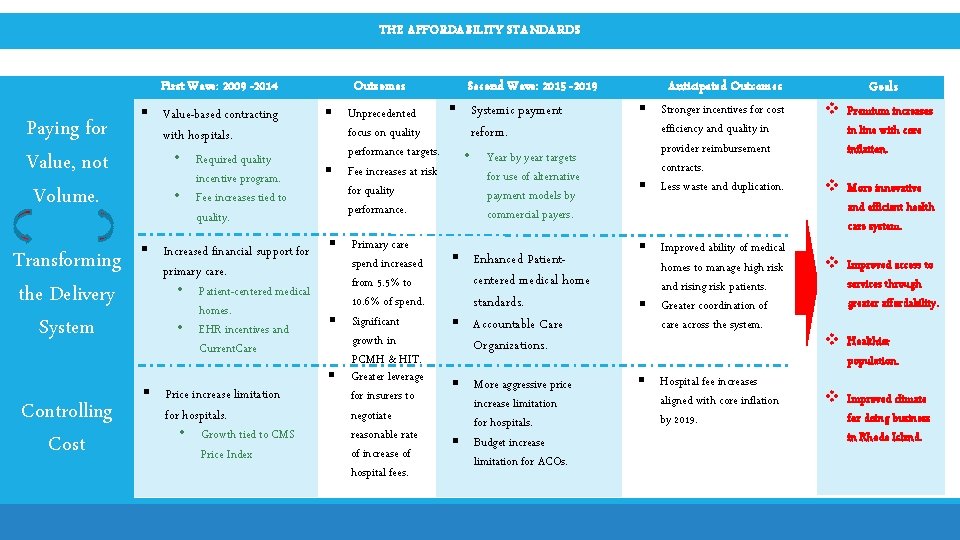
THE AFFORDABILITY STANDARDS First Wave: 2009 -2014 Paying for Value, not Volume. Transforming the Delivery System Controlling Cost § Value-based contracting with hospitals. • • Required quality incentive program. Fee increases tied to quality. § Increased financial support for primary care. • • Patient-centered medical homes. EHR incentives and Current. Care § Price increase limitation for hospitals. • Growth tied to CMS Price Index Outcomes § Unprecedented focus on quality performance targets. § Fee increases at risk for quality performance. § Primary care spend increased from 5. 5% to 10. 6% of spend. § Significant growth in PCMH & HIT. § Greater leverage for insurers to negotiate reasonable rate of increase of hospital fees. Second Wave: 2015 -2019 § Systemic payment reform. • Year by year targets for use of alternative payment models by commercial payers. § Enhanced Patientcentered medical home standards. § Accountable Care Organizations. § More aggressive price increase limitation for hospitals. § Budget increase limitation for ACOs. Anticipated Outcomes § Stronger incentives for cost efficiency and quality in provider reimbursement contracts. § Less waste and duplication. § Improved ability of medical homes to manage high risk and rising risk patients. § Greater coordination of care across the system. § Hospital fee increases aligned with core inflation by 2019. Goals v Premium increases in line with core inflation. v More innovative and efficient health care system. v Improved access to services through greater affordability. v Healthier population. v Improved climate for doing business in Rhode Island.
Questions?