Nurses role in injury prevention Prevention strategies Education


- Slides: 22
Nurse’s role in injury prevention • • • Prevention strategies Education Alert to safety hazards Evaluating safety risks Implementing safety programs
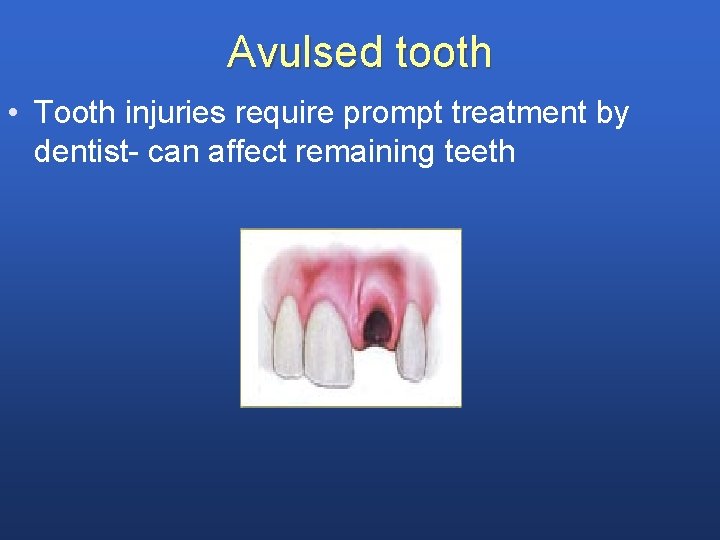
Avulsed tooth • Tooth injuries require prompt treatment by dentist- can affect remaining teeth
• • Recover tooth Hold tooth by crown avoiding root If dirty rinse in water Insert tooth back in socket – have child hold in place -70% chance for reattachment if within 30 mins • Transport to dentist immediately • If unable to reimplant – -place tooth in cold milk – In saliva or parent’s mouth under tongue
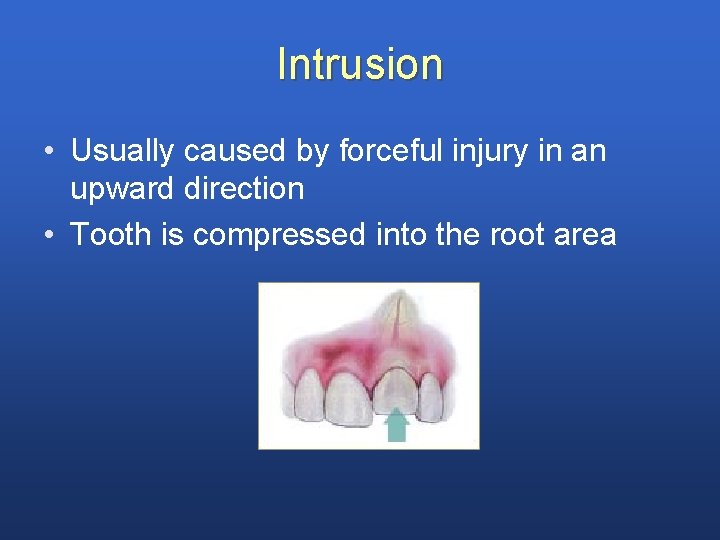
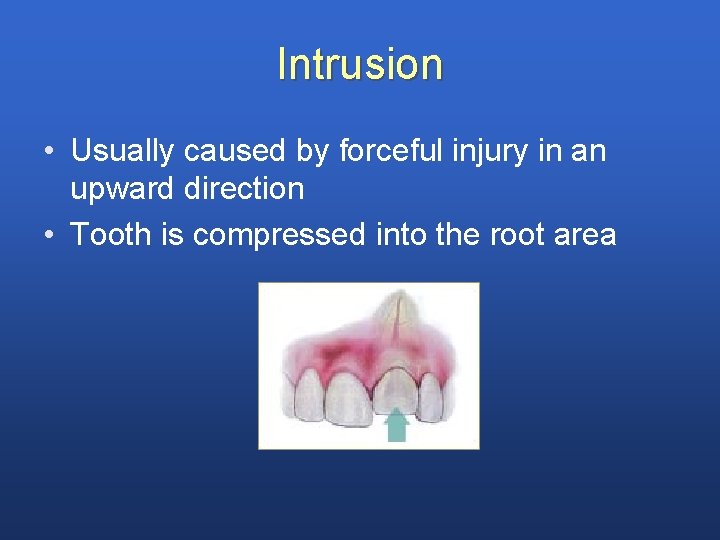
Intrusion • Usually caused by forceful injury in an upward direction • Tooth is compressed into the root area
Eye injury • • • Foreign object. Chemical burns Ultraviolet burns – Hematoma – Penetrating injuries – (see p 1011)
Foreign Body in Nose
Foreign Bodies Nasal • Food, beans, crayon pieces, paper, etc. • Leads to irritation, infection, obstruction • Foul-smelling nasal discharge, difficulty breathing, discomfort • Do NOT probe nose or try to remove if not visible • Have child blow gently through affected nostril
Foreign Body Aspiration • Choking = implementation of i)back blows ii) heimlick maneuver (CPR certification. Also refer to figs 31 -25 & 31. 26) • S&S of distress – Cannot speak – Becomes cyanoic – Collapses child is truly choking STAT intervention can die within 4 min • Follow-up care after foreign body removed: includes monitoring for resp distress, HT parents

Ear • Do NOT attempt to remove by probing with swab • Do NOT reach into ear with tweezers Prevention • Keep small objects out of reach of infants and toddlers • Discourage children from putting things in body openings
Bites/Stings • Prevention – protective clothing – DEET (diethyltoluamide) –best repellent – Follow label instructions -> reapply after swimming, sweating, throughout day – NB – side effects have been reported in young children. ˙. long term effects of DEET are unknown caution agains use of high concentrations of DEET and excessive application –. ˙. Apply DEET (concentration) < 10% to infants clothing – Do not apply DEET to childrens’ hands d/t risk of contact with eyes – Remove DEET with soap & water when child is brought indoors • Snake bites – tourniquet, suction – Transport snake with victim • Animal Bites – Risk for infection, (see p 786 →)
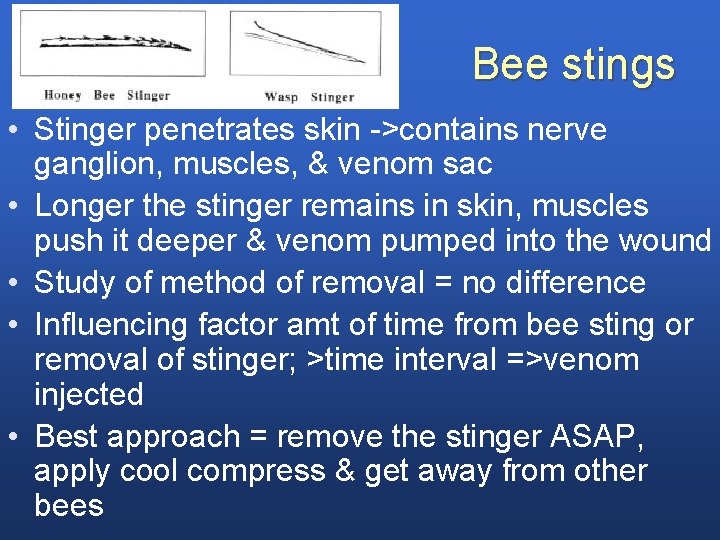
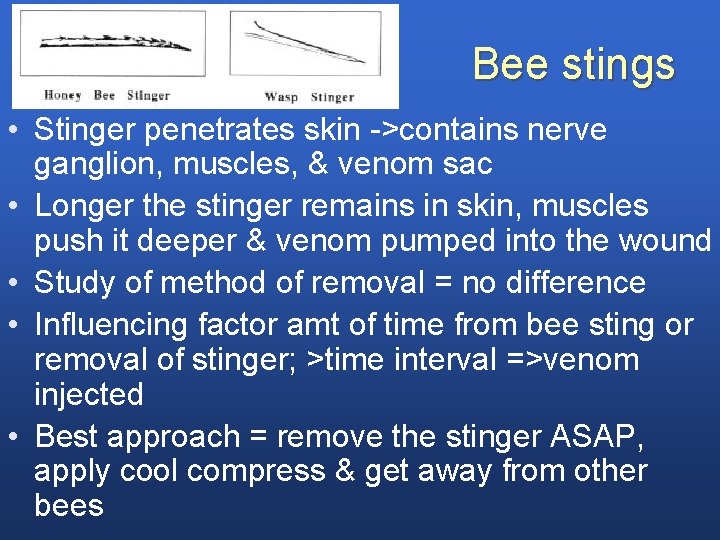
Bee stings • Stinger penetrates skin ->contains nerve ganglion, muscles, & venom sac • Longer the stinger remains in skin, muscles push it deeper & venom pumped into the wound • Study of method of removal = no difference • Influencing factor amt of time from bee sting or removal of stinger; >time interval =>venom injected • Best approach = remove the stinger ASAP, apply cool compress & get away from other bees
• Children taught to avoid bees • Those sensitized & demonstrate life-threatening systemic response, SQ admin epinephrine STAT • Hypersensitive children; kit with epinephrine, syringe, & antihistamine preparation. • Wear medic alert bracelet • Someone at school, if not nse, should be designated to administer if need be • Parents responsible to ensure expiration date current & replace an outdated one
• Etiology – – West Nile Virus By arbovirus First case in US in NY 1999 Cases now in over 40 states Mortality is 50% -mainly in older persons • Transmission – Bite of mosquito that has fed on infected bird or animal – through bld transfusions & organ transplant – Not person to person; no isolation other than Standard Precautions • Clinical Manifestations – Febrile illness with rash, arthritis, myalgias, weakness, lymphadenopathy, meningoencephalitis • Nursing Considerations – Prevention of mosquito bites: proper clothing, insect repellent, removal of standing water – Inform parents to place mosquito netting over buggy/playpen – Be alert for acute febrile illness & deteriorating condition
Deet – bug repellents • • • Effective for variety of insects Protection from 1 - several hours Reapply if wet Adverse effects See recommendations for use from Health Canada
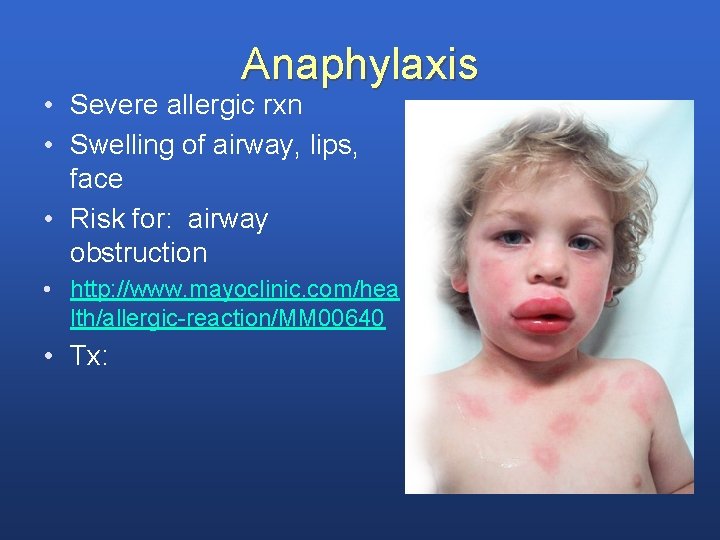
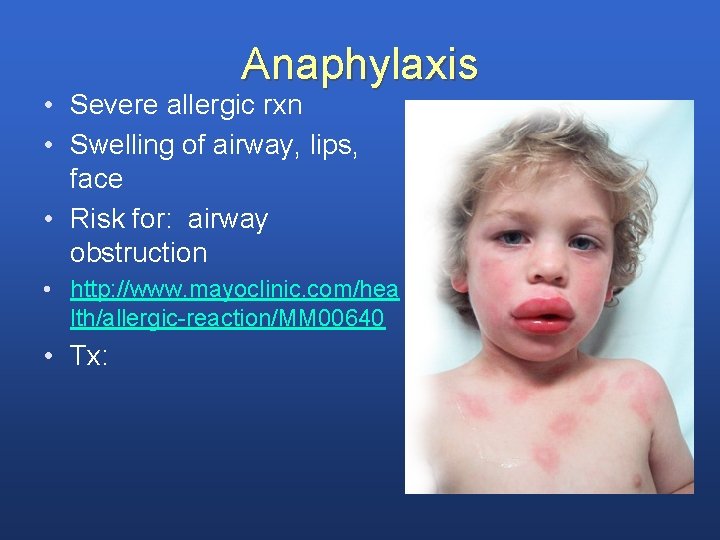
Anaphylaxis • Severe allergic rxn • Swelling of airway, lips, face • Risk for: airway obstruction • http: //www. mayoclinic. com/hea lth/allergic-reaction/MM 00640 • Tx:
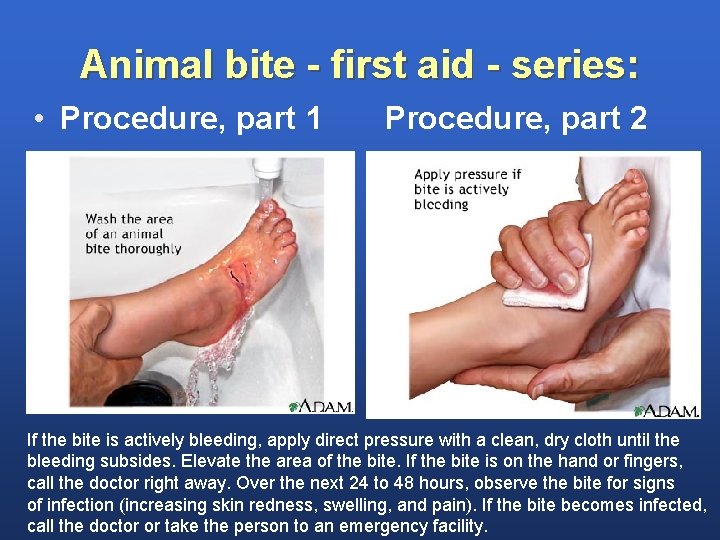
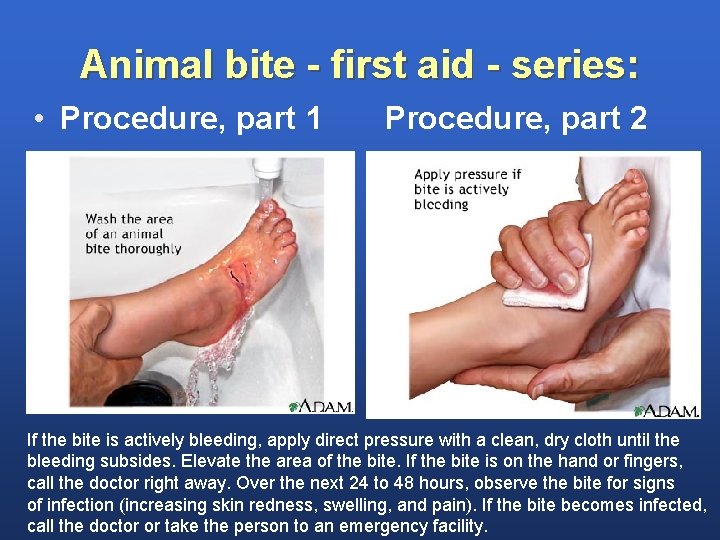
Animal bite - first aid - series: • Procedure, part 1 Procedure, part 2 If the bite is actively bleeding, apply direct pressure with a clean, dry cloth until the bleeding subsides. Elevate the area of the bite. If the bite is on the hand or fingers, call the doctor right away. Over the next 24 to 48 hours, observe the bite for signs of infection (increasing skin redness, swelling, and pain). If the bite becomes infected, call the doctor or take the person to an emergency facility.
• Did you know. . • Rabies is 100% preventable, yet results in over 55, 000 human deaths each year. • Rabies is present throughout the world. • The greatest number of human deaths occur in Asia and Africa where canine (dog) rabies is common.
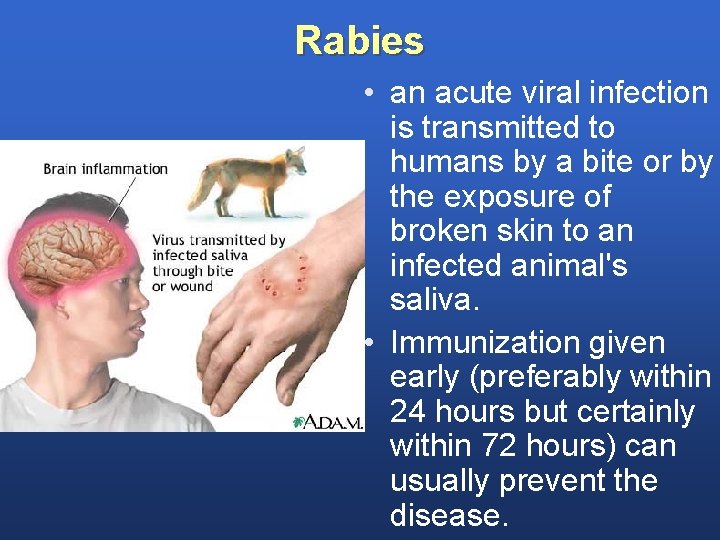
Rabies • An acute infection of the CNS • Caused by virus transmitted by saliva of infected animal • Virus multiplies in muscles and fatal if untreated • Highest incidence in humans is in children younger than 15 years
Rabies (cont. ) • 12% of cases come from domestic animals, especially cats • Infected wild animals are most commonly raccoons, skunks, foxes, and bats • Unprovoked attack is more likely to indicate a rabid animal than a provoked attack • Antirabies protocol/shots started immediately
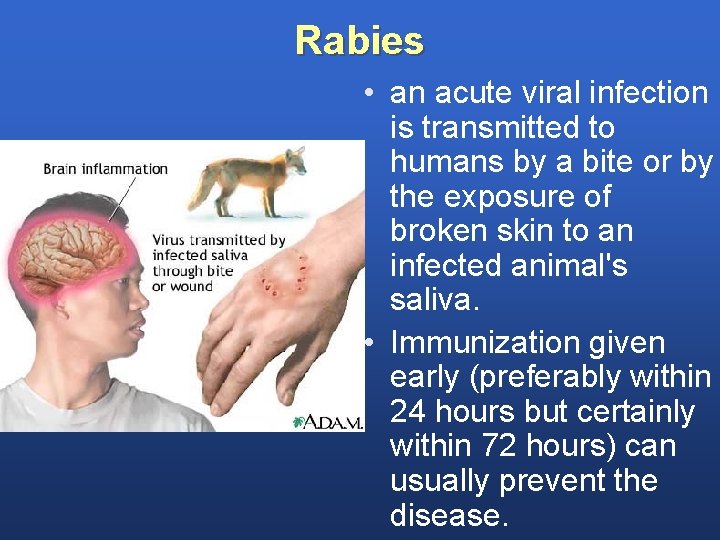
Rabies • an acute viral infection is transmitted to humans by a bite or by the exposure of broken skin to an infected animal's saliva. • Immunization given early (preferably within 24 hours but certainly within 72 hours) can usually prevent the disease.

 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Battering intentional or unintentional
Battering intentional or unintentional Fall prevention quiz for nurses
Fall prevention quiz for nurses Objectives of community health nursing
Objectives of community health nursing Mileu therapy
Mileu therapy Injury prevention, safety and first aid
Injury prevention, safety and first aid Workplace fatality prevention
Workplace fatality prevention Needle stick injury prevention images
Needle stick injury prevention images Back injury prevention quiz answers
Back injury prevention quiz answers Hand injury prevention
Hand injury prevention Sharps injury prevention program
Sharps injury prevention program Atlas injury prevention
Atlas injury prevention Serious injury and fatality prevention
Serious injury and fatality prevention Quality and safety education for nurses
Quality and safety education for nurses Quality and safety education for nurses
Quality and safety education for nurses Qsen phases
Qsen phases Quality safety education for nurses
Quality safety education for nurses Azure web role worker role example
Azure web role worker role example Soziale identität krappmann
Soziale identität krappmann Statuses and their related roles determine
Statuses and their related roles determine Role of ssa in universalisation of elementary education
Role of ssa in universalisation of elementary education Role of rmsa in universalisation of secondary education ppt
Role of rmsa in universalisation of secondary education ppt Higher education role analysis
Higher education role analysis