Military Family Physician Attitudes Toward Running Gait Retraining



- Slides: 22

Military Family Physician Attitudes Toward Running Gait Retraining Alex Knobloch, MD, CAQSM Capt, USAF, MC Faculty Physician, DGMC Family Medicine Residency
Disclosures The information presented in this activity represents the opinions of the author and not those of the Department of Defense, U. S. Air Force, or the Uniformed Services University. I have no financial interests or relationships to disclose


Methods • Cross-Sectional Survey • Study Population: – 532 military family medicine physicians and residents • Main Outcomes: 1) Frequency of… 2) Confidence in… 3) Value of… …discussions of running gait retraining with patients with running-related injuries 4) Obstacles to gait retraining discussions
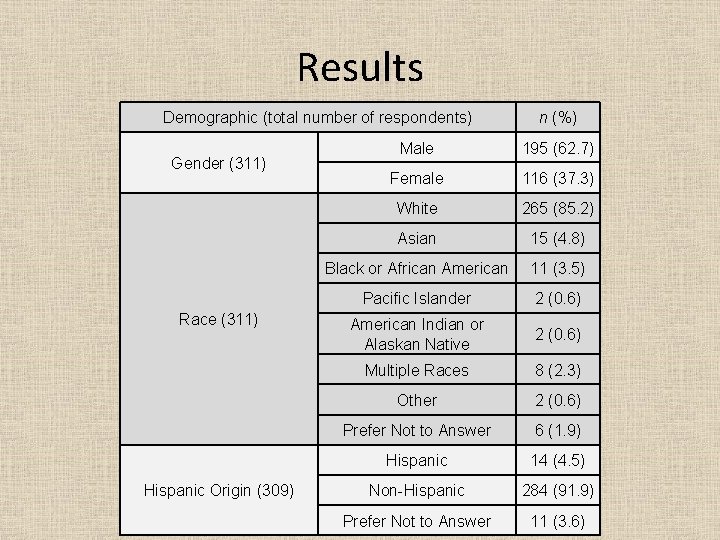
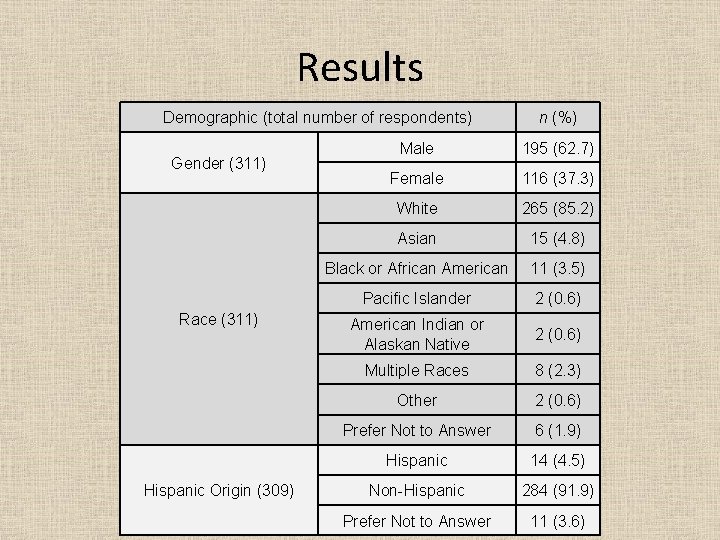
Results Demographic (total number of respondents) Gender (311) Race (311) Hispanic Origin (309) n (%) Male 195 (62. 7) Female 116 (37. 3) White 265 (85. 2) Asian 15 (4. 8) Black or African American 11 (3. 5) Pacific Islander 2 (0. 6) American Indian or Alaskan Native 2 (0. 6) Multiple Races 8 (2. 3) Other 2 (0. 6) Prefer Not to Answer 6 (1. 9) Hispanic 14 (4. 5) Non-Hispanic 284 (91. 9) Prefer Not to Answer 11 (3. 6)
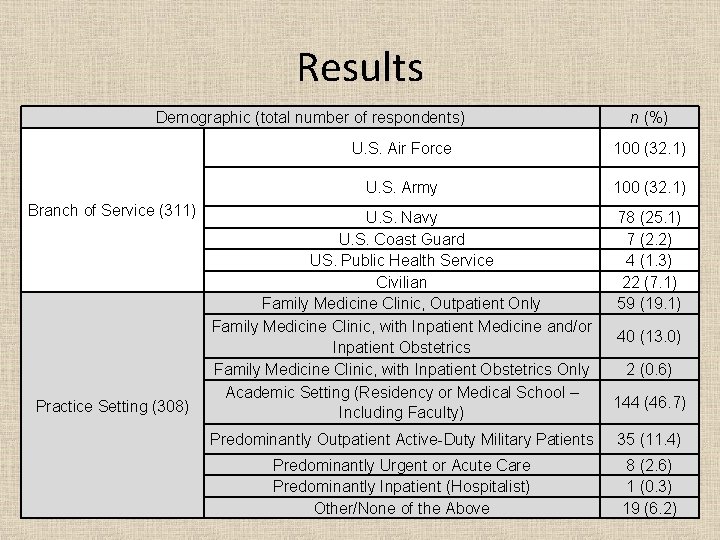
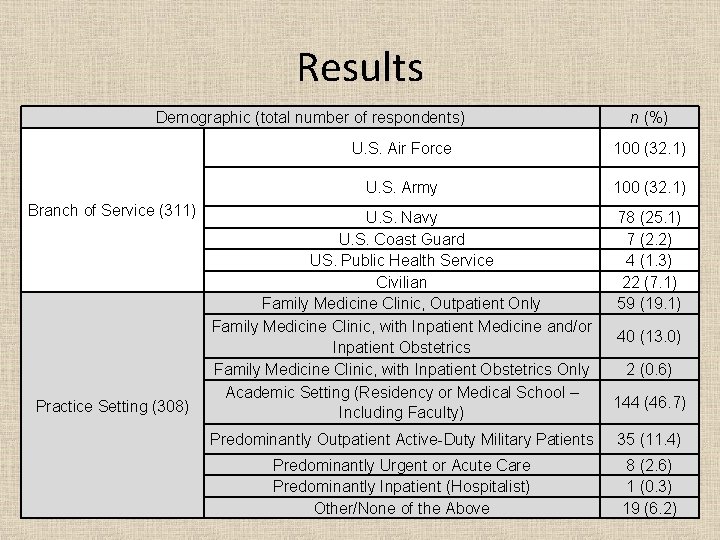
Results Demographic (total number of respondents) Branch of Service (311) Practice Setting (308) n (%) U. S. Air Force 100 (32. 1) U. S. Army 100 (32. 1) U. S. Navy U. S. Coast Guard US. Public Health Service Civilian Family Medicine Clinic, Outpatient Only Family Medicine Clinic, with Inpatient Medicine and/or Inpatient Obstetrics Family Medicine Clinic, with Inpatient Obstetrics Only Academic Setting (Residency or Medical School – Including Faculty) 78 (25. 1) 7 (2. 2) 4 (1. 3) 22 (7. 1) 59 (19. 1) 40 (13. 0) 2 (0. 6) 144 (46. 7) Predominantly Outpatient Active-Duty Military Patients 35 (11. 4) Predominantly Urgent or Acute Care Predominantly Inpatient (Hospitalist) Other/None of the Above 8 (2. 6) 1 (0. 3) 19 (6. 2)
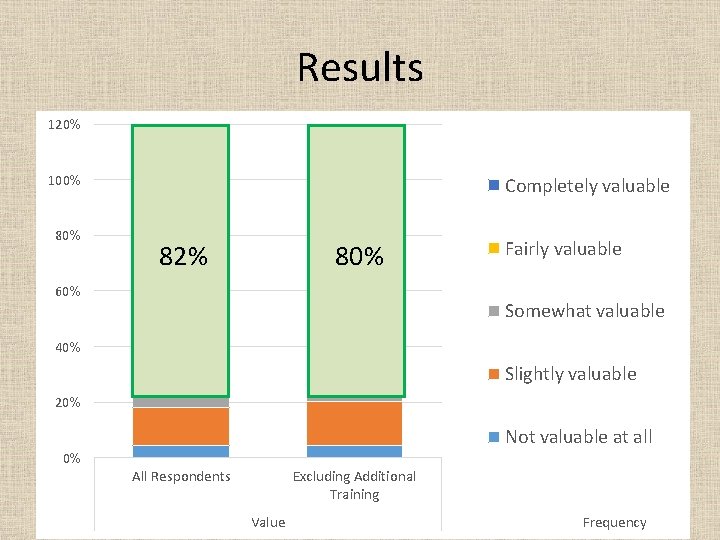
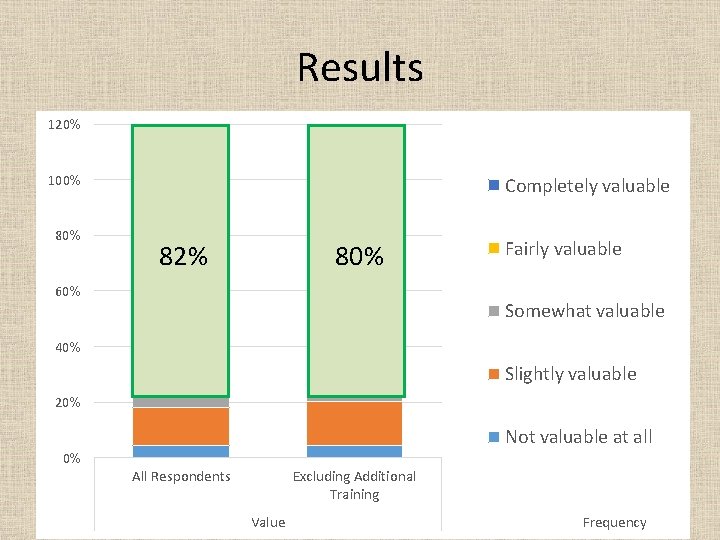
Results 120% 100% 80% Completely valuable 82% 80% 60% Fairly valuable Somewhat valuable 40% Slightly valuable 20% Not valuable at all 0% All Respondents Excluding Additional Training Value Frequency
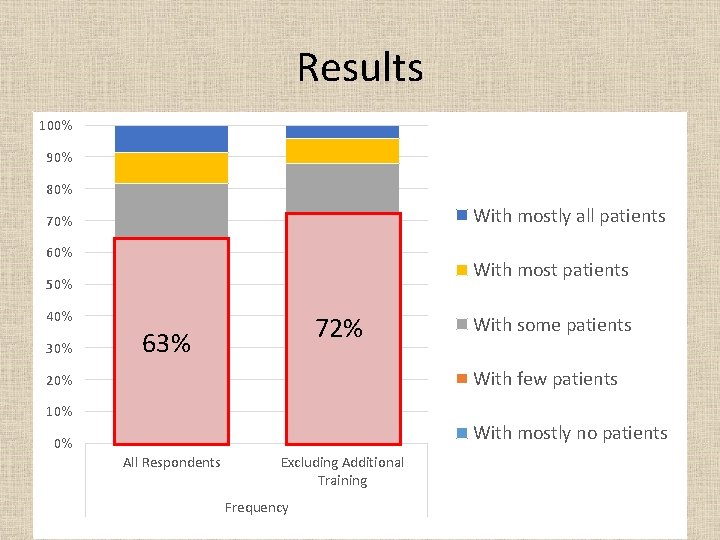
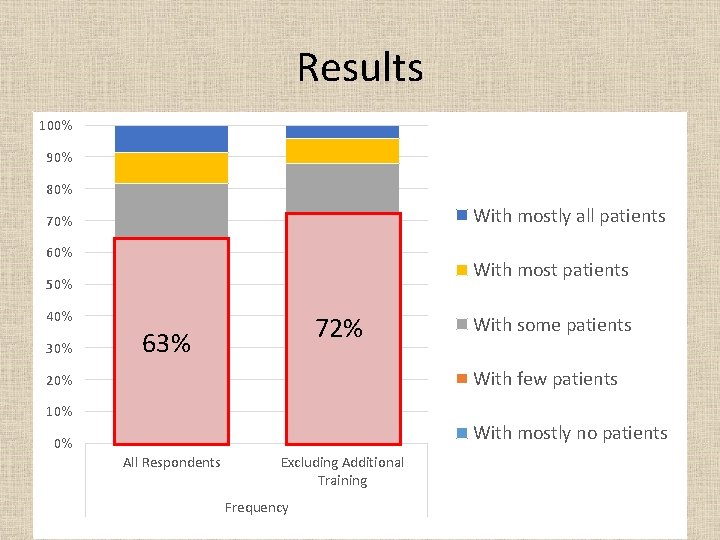
Results 100% 90% 80% With mostly all patients 70% 60% With most patients 50% 40% 30% 72% 63% With some patients With few patients 20% 10% With mostly no patients 0% All Respondents Excluding Additional Training Frequency
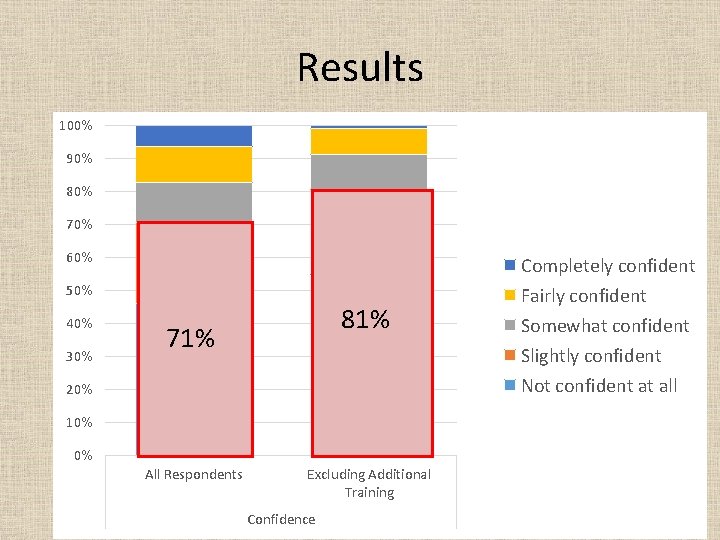
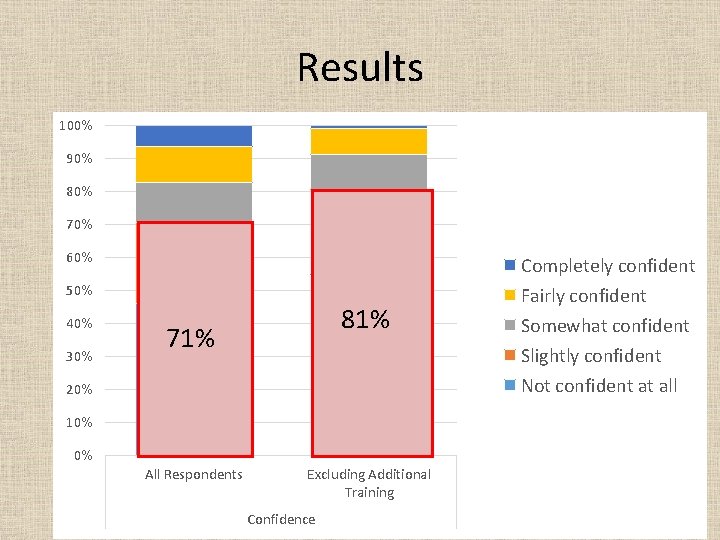
Results 100% 90% 80% 70% 60% 50% 40% 30% 81% 71% 20% 10% 0% All Respondents Excluding Additional Training Confidence Completely confident Fairly confident Somewhat confident Slightly confident Not confident at all
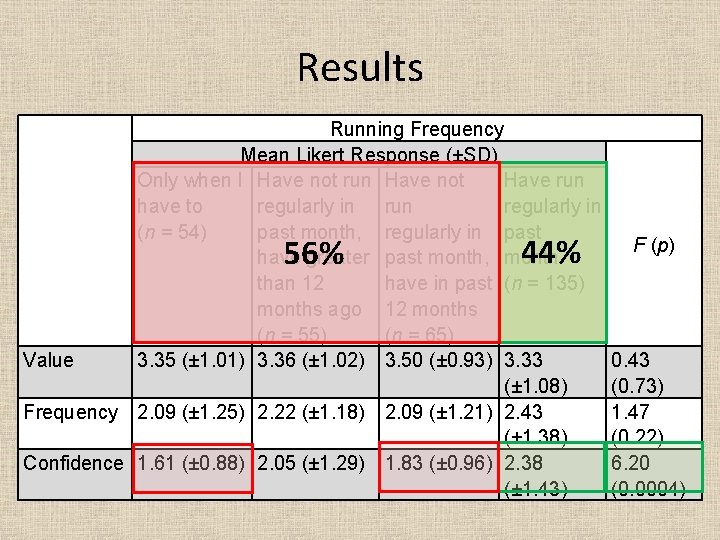
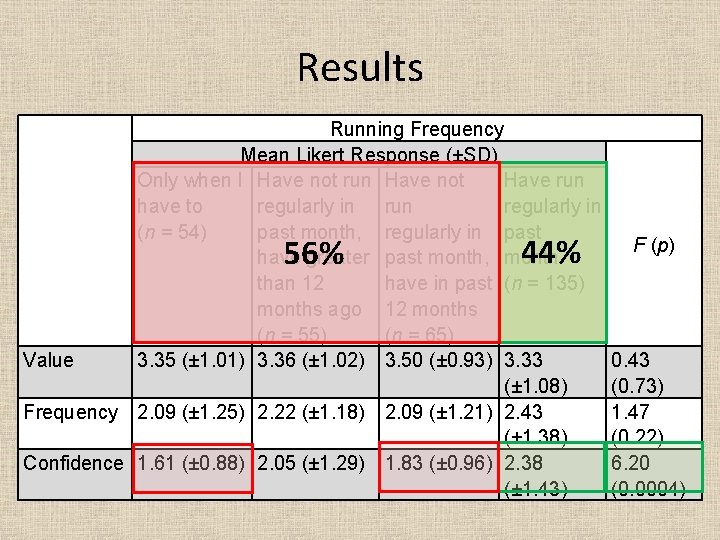
Results Running Frequency Mean Likert Response (±SD) Only when I Have not run Have not Have run have to regularly in run regularly in (n = 54) past month, regularly in past have greater past month, month than 12 have in past (n = 135) months ago 12 months (n = 55) (n = 65) Value 3. 35 (± 1. 01) 3. 36 (± 1. 02) 3. 50 (± 0. 93) 3. 33 (± 1. 08) Frequency 2. 09 (± 1. 25) 2. 22 (± 1. 18) 2. 09 (± 1. 21) 2. 43 (± 1. 38) Confidence 1. 61 (± 0. 88) 2. 05 (± 1. 29) 1. 83 (± 0. 96) 2. 38 (± 1. 43) 56% 44% F (p) 0. 43 (0. 73) 1. 47 (0. 22) 6. 20 (0. 0004)
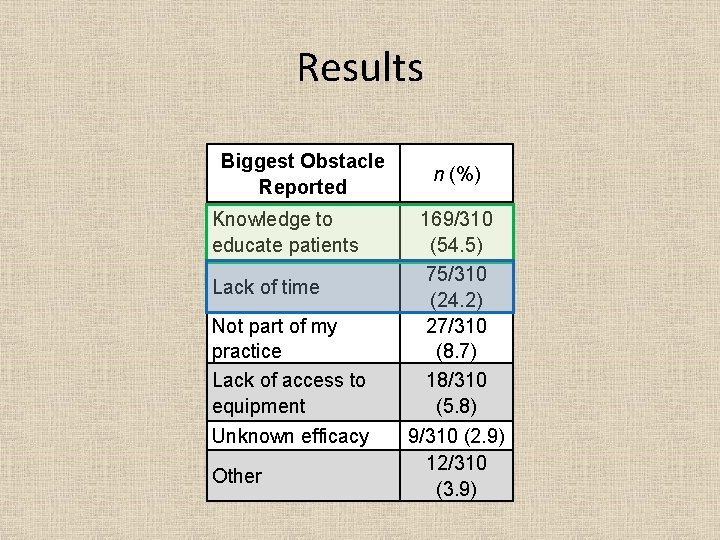
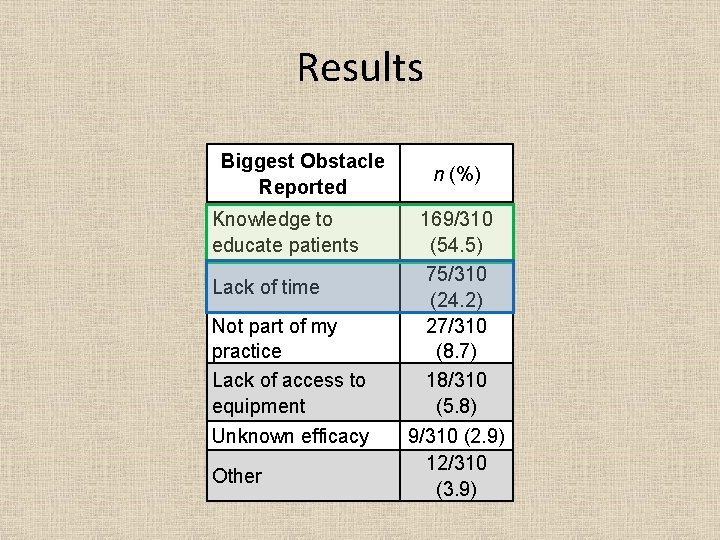
Results Biggest Obstacle Reported Knowledge to educate patients Lack of time Not part of my practice Lack of access to equipment Unknown efficacy Other n (%) 169/310 (54. 5) 75/310 (24. 2) 27/310 (8. 7) 18/310 (5. 8) 9/310 (2. 9) 12/310 (3. 9)
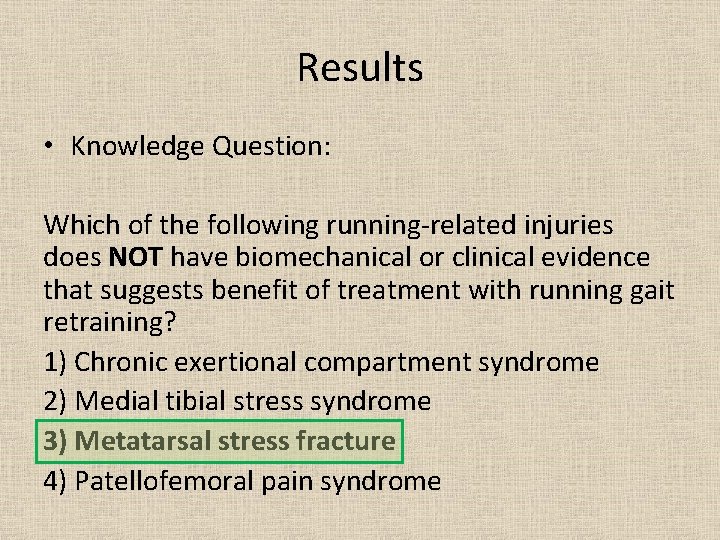
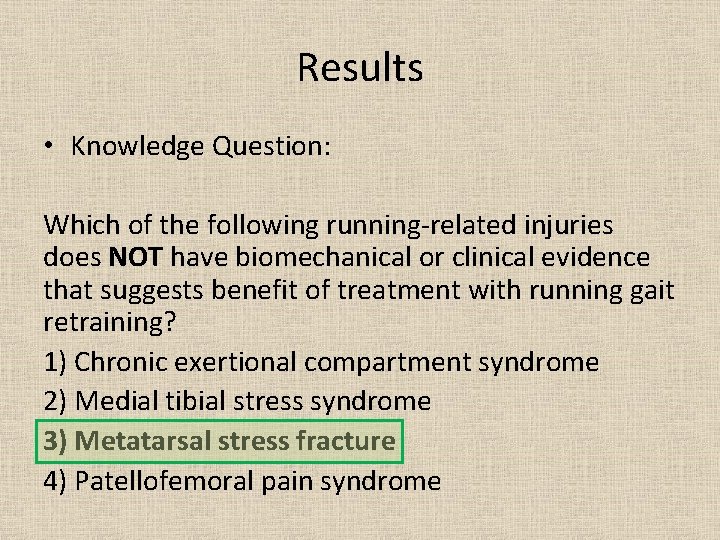
Results • Knowledge Question: Which of the following running-related injuries does NOT have biomechanical or clinical evidence that suggests benefit of treatment with running gait retraining? 1) Chronic exertional compartment syndrome 2) Medial tibial stress syndrome 3) Metatarsal stress fracture 4) Patellofemoral pain syndrome
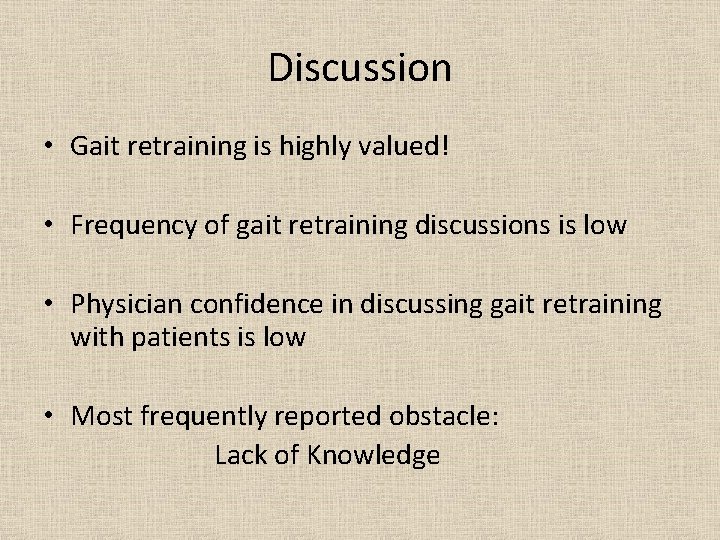
Discussion • Gait retraining is highly valued! • Frequency of gait retraining discussions is low • Physician confidence in discussing gait retraining with patients is low • Most frequently reported obstacle: Lack of Knowledge
Discussion • Limitations: – Unable to make causal inferences – Social desirability bias? – Generalizability?
Next Steps • Studies designed to increase knowledge – Online CME curriculum? – Teaching at the GME level? • Studies designed to decrease knowledge needed and decrease time commitment – Simplified gait retraining approaches (i. e. recommendation to solely increase gait cadence)
Acknowledgements • Dr. Robert Oh • Dr. Jennifer Thornton • MPCRN and their Fall 2019 Writing Rounds participants • Dr. Glynnis Knobloch
E-mail questions to: alexander. c. knobloch. mil@mail. mil
References • • • Lun V, Meeuwisse WH, Stergiou P, Stefanyshyn D. Relation between running injury and static lower limb alignment in recreational runners. British journal of sports medicine. 2004; 38(5): 576 -580. van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SM, Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. British journal of sports medicine. 2007; 41(8): 469 -480; discussion 480. Bullock SH, Jones BH, Gilchrist J, Marshall SW. Prevention of physical training-related injuries recommendations for the military and other active populations based on expedited systematic reviews. Am J Prev Med. 2010; 38(1 Suppl): S 156 -181. Napier C, Cochrane CK, Taunton JE, Hunt MA. Gait modifications to change lower extremity gait biomechanics in runners: a systematic review. British journal of sports medicine. 2015; 49(21): 1382 -1388. Heiderscheit BC, Chumanov ES, Michalski MP, Wille CM, Ryan MB. Effects of step rate manipulation on joint mechanics during running. Medicine and science in sports and exercise. 2011; 43(2): 296 -302. Schubert AG, Kempf J, Heiderscheit BC. Influence of stride frequency and length on running mechanics: a systematic review. Sports Health. 2014; 6(3): 210 -217. Barton CJ, Bonanno DR, Carr J, et al. Running retraining to treat lower limb injuries: a mixed-methods study of current evidence synthesised with expert opinion. British journal of sports medicine. 2016; 50(9): 513 -526. Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. British journal of sports medicine. 2011; 45(9): 691 -696. Diebal AR GR, Alitz C, Gerber JP. Forefoot running improves pain and disability associated with chronic exertional compartment syndrome. The American journal of sports medicine. 2012; 40(5): 1060 -1067. Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech (Bristol, Avon). 2012; 27(10): 1045 -1051.
References • • • Allen DJ. Treatment of distal iliotibial band syndrome in a long distance runner with gait re-training emphasizing step rate manipulation. International journal of sports physical therapy. 2014; 9(2): 222 -231. Breen DT, Foster J, Falvey E, Franklyn-Miller A. Gait re-training to alleviate the symptoms of anterior exertional lower leg pain: a case series. International journal of sports physical therapy. 2015; 10(1): 85 -94. Roper JL, Harding EM, Doerfler D, et al. The effects of gait retraining in runners with patellofemoral pain: A randomized trial. Clin Biomech (Bristol, Avon). 2016; 35: 14 -22. Zimmermann WO LC, Beutler A. Gait retraining as part of the treatment programme for soldiers with exercise-related leg pain: preliminary clinical experiences and retention. S Afr J Sports Med. 2017; 29: 1 -6. Bonacci J, Hall M, Saunders N, Vicenzino B. Gait retraining versus foot orthoses for patellofemoral pain: a pilot randomised clinical trial. J Sci Med Sport. 2018; 21(5): 457 -461. Chan ZYS, Zhang JH, Au IPH, et al. Gait Retraining for the Reduction of Injury Occurrence in Novice Distance Runners: 1 -Year Follow-up of a Randomized Controlled Trial. The American journal of sports medicine. 2018; 46(2): 388 -395. Bramah C PS, Gill N, Herrington L. A 10% increase in step rate improves running kinematics and clinical outcomes in runners with patellofemoral pain at 4 weeks and 3 months. The American journal of sports medicine. 2019. Rendall EO, Mohtadi NG. Survey of competitive distance runners in Alberta: satisfaction with health care services with respect to running injuries. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 1997; 7(2): 104 -112. Smits DW, Huisstede B, Verhagen E, et al. Short-Term Absenteeism and Health Care Utilization Due to Lower Extremity Injuries Among Novice Runners: A Prospective Cohort Study. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2016; 26(6): 502 -509.
References • • Davis IS, Futrell E. Gait Retraining: Altering the Fingerprint of Gait. Phys Med Rehabil Clin N Am. 2016; 27(1): 339 -355. Zimmermann WO VVN, Linschoten CW, Beutler A, Hoencamp R, Bakker EWP. Gait retraining reduces vertical ground reaction forces in running shoes and military boots. Transl Sports Med. 2019; 2: 90 -97. Cameron KL OB. The burden and management of sports-related musculoskeletal injuies and conditions within the US military. Clin Sports Med. 2014; 33: 573 -589. Grimm P MT, Potter BK. Combat and noncombat musculoskeletal injuries in the US military. Sports Med Arthrosc Rev. 2019; 27: 84 -91.
 Once upon a time there lived a girl
Once upon a time there lived a girl Running running running
Running running running What is attribution retraining in sport
What is attribution retraining in sport Operator retraining program
Operator retraining program Who was babur
Who was babur Family medicine fellowships
Family medicine fellowships Jeannie watkins
Jeannie watkins Physician wellness academic consortium
Physician wellness academic consortium Computerized physician order entry definition
Computerized physician order entry definition A physician claims that joggers maximum volume
A physician claims that joggers maximum volume Physician employment models
Physician employment models The good physician treats the disease
The good physician treats the disease Hcp segmentation
Hcp segmentation Pricewaterhouse
Pricewaterhouse Physician personas
Physician personas Elisha goodman prayer points for breakthrough
Elisha goodman prayer points for breakthrough Mohh physician
Mohh physician Safer sign out
Safer sign out Physician reentry program
Physician reentry program Oklahoma board of nursing lpn scope of practice
Oklahoma board of nursing lpn scope of practice Popliteal artery
Popliteal artery Physician competency reference set
Physician competency reference set Pa ieb physician certification form
Pa ieb physician certification form