Living Dying Well in Prison Jayne Miller Service
- Slides: 18
Living & Dying Well in Prison Jayne Miller – Service Manager Jacqueline Carrigan – Clinical Manager Prison Healthcare
There are currently 3 prisons within the NHS Greater Glasgow & Clyde area: • HMP Barlinnie • HMP Low Moss • HMP Greenock In 2008/2009 Scotland Prison Act (1989) was repealed allowing NHS Boards to become sole healthcare providers for patients held in prisons in their catchment areas and transfer formally took place on 1 st November 2011.
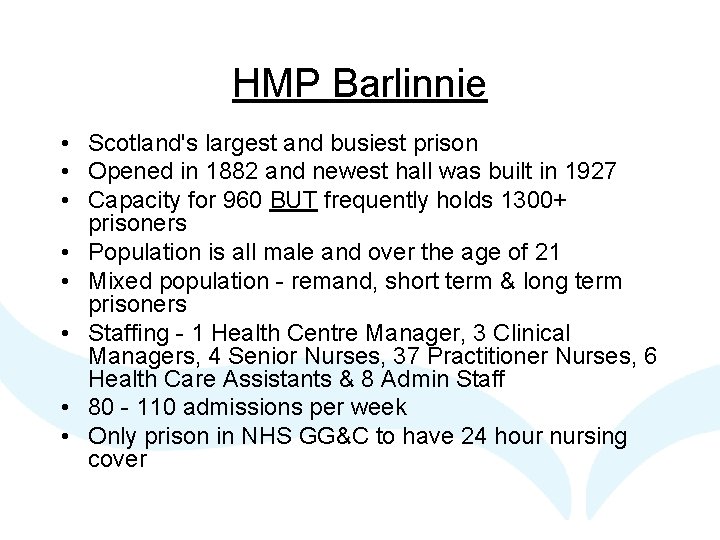
HMP Barlinnie • Scotland's largest and busiest prison • Opened in 1882 and newest hall was built in 1927 • Capacity for 960 BUT frequently holds 1300+ prisoners • Population is all male and over the age of 21 • Mixed population - remand, short term & long term prisoners • Staffing - 1 Health Centre Manager, 3 Clinical Managers, 4 Senior Nurses, 37 Practitioner Nurses, 6 Health Care Assistants & 8 Admin Staff • 80 - 110 admissions per week • Only prison in NHS GG&C to have 24 hour nursing cover
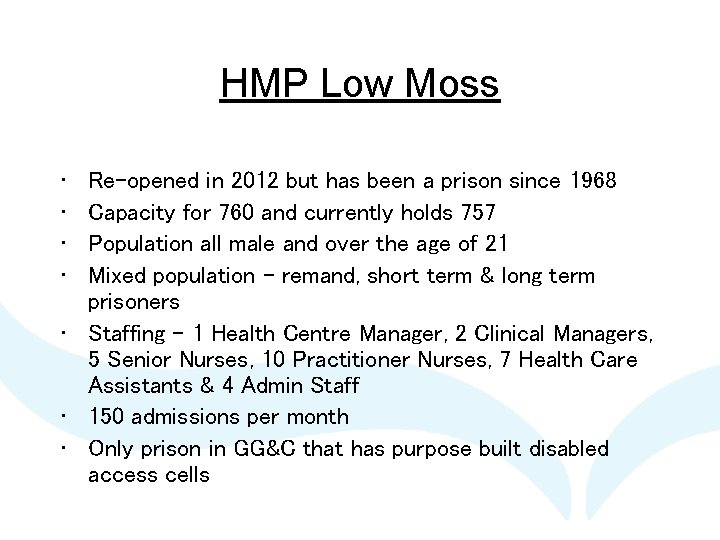
HMP Low Moss • • Re-opened in 2012 but has been a prison since 1968 Capacity for 760 and currently holds 757 Population all male and over the age of 21 Mixed population - remand, short term & long term prisoners • Staffing - 1 Health Centre Manager, 2 Clinical Managers, 5 Senior Nurses, 10 Practitioner Nurses, 7 Health Care Assistants & 4 Admin Staff • 150 admissions per month • Only prison in GG&C that has purpose built disabled access cells
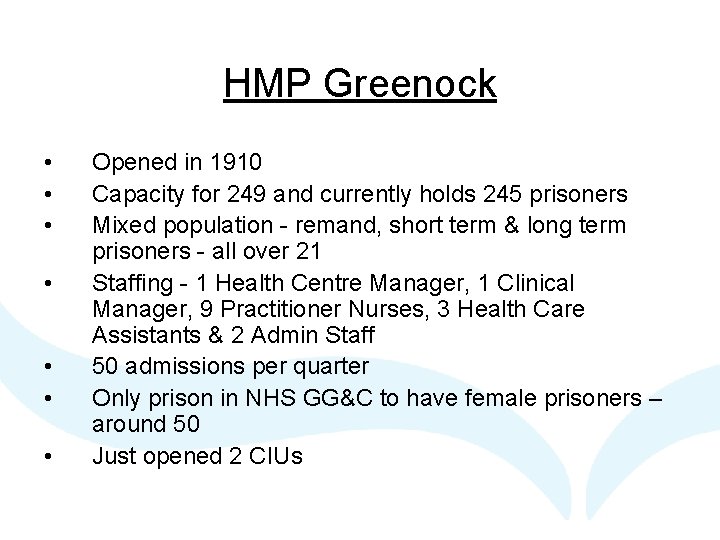
HMP Greenock • • Opened in 1910 Capacity for 249 and currently holds 245 prisoners Mixed population - remand, short term & long term prisoners - all over 21 Staffing - 1 Health Centre Manager, 1 Clinical Manager, 9 Practitioner Nurses, 3 Health Care Assistants & 2 Admin Staff 50 admissions per quarter Only prison in NHS GG&C to have female prisoners – around 50 Just opened 2 CIUs
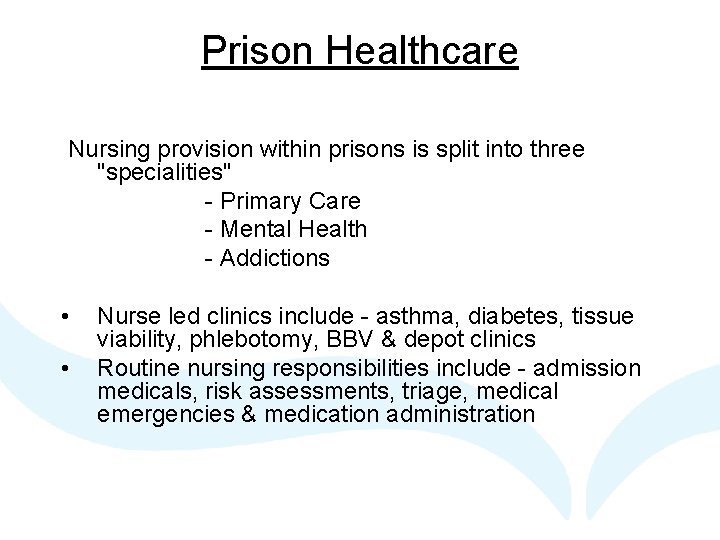
Prison Healthcare Nursing provision within prisons is split into three "specialities" - Primary Care - Mental Health - Addictions • • Nurse led clinics include - asthma, diabetes, tissue viability, phlebotomy, BBV & depot clinics Routine nursing responsibilities include - admission medicals, risk assessments, triage, medical emergencies & medication administration
Prison Healthcare • Keep Well Services - Sexual Health, Smoking Cessation, Medicine Management • Medical input is via GP's - Mon - Fri, 9 am - 5 pm, preset slots • External services include - Psychiatry, Pharmacy, Dentist, Podiatrist & Optician • Out of hours medical cover is provided via Forensic Medical Examiners (FME's) linked with Police Custody Suite Service • Bid currently in for Psychology
Barriers to providing Healthcare in a Prison setting • • Lack of appropriate accommodation Access to Personal Care Access to Palliative Care Family pressures Prison regime Stigma when attending OP Clinics SPS Compassionate Release Policy
Prison Healthcare A Case Study
Case Study Mr Q • Mr Q is a 52 year old male who was serving a 24 month sentence within the protection hall of HMP Barlinnie • He self referred to Prison Healthcare as he had concerns regarding sudden weight loss and difficulty swallowing • After an initial assessment by the hall nurse Mr Q’s case was discussed with the G. P, he was further reviewed and referred for an Endoscopy
Pathophysiology • Following the Endoscopy, Mr Q was referred to a Specialist Oncologist (Beatson) where he was further assessed (chest x-ray, CT scan and routine bloods). • He was diagnosed with Squamous Cell Carcinoma Oesophageal Cancer with no metastasis • After consideration of the treatment options Mr Q refused all treatment
Past Medical History • Mr Q had no chronic diseases or significant past medical history • He had not been seen by medical staff since his admission to the establishment (12 weeks ago) • He had a history of chronic alcohol dependence, he had received an alcohol withdrawal since admission but had refused any further support from addiction services. • He was a cigarette smoker of approximately 15 -20 roll ups per day and refused referral to smoke cessation services • This was his first custodial sentence
Nursing Assessment • After further consideration and discussions with both nursing and medical staff Mr Q agreed to treatment • Complex case discussion including Mr Q, nursing, medical and the keep well nurse • Formulation of a nursing care plan which involved, planned daily assessment and intervention by healthcare staff • Discussion with wider nursing team and the outpatient nurse from The Beatson
Nursing Interventions • Mr Q attended The Beatson for Radiation Therapy on a daily basis for 14 days • Due to Mucositis / swallowing difficulties Mr Q had a nasogastric tube passed. This was to enable the administration of medication • Mr Q was able to manage a liquid diet and meal supplement drinks • Mr Q was shown how to manage his own NG tube but had challenges with this
Nursing Interventions • Whilst in the establishment, Mr Q received intensive nursing interventions, weekly weights, assessment of NG tube, oral assessment and ongoing emotional support • Administration of prescribed medications • Regular liaison and meetings with relatives and SPS staff • Regular liaison with the outpatient specialist nurse
Liaison with SPS Staff • Mr Q gave us consent to discuss his care with SPS staff to ensure we could request specific medical markers • Liaison with SPS catering, Residential Officers and Escorting Agencies • Liaison with security staff re clinical equipment which was required (glass products) • Planning of appointments and the need for these to be on specific days • SPS considering an application to the Scottish Government for Early Release on Licence on Compassionate Grounds
Outcome • Mr Q completed his treatment and is currently in remission • Mr Q was advised re. positive lifestyle changes and engaged with the Keep Well Service. He had lengthy periods of time with nursing staff which also had a positive effect on his mental state • Mr Q did report symptoms of stress and coping strategies were put in place to enable him to deal with these symptoms • Mr Q continued to smoke during his treatment and when the treatment was completed • Mr Q was transferred to another SPS establishment nearer his home once his treatment was finished
Conclusion • Communication between SPS and NHS can be challenging as we are both considering the healthcare of patients from very different angles • HMP Barlinnie is not an ideal place to provide complex medical care/palliative care. There is a lack of space in the cells, poor light, ventilation issues and the patients regularly find the environment cold. • Despite the challenges we work collaboratively with patients, relatives and wider members of the healthcare team and receive positive feedback
 Janet childs center for living with dying
Janet childs center for living with dying Jayne van bramer
Jayne van bramer Disney company hierarchy
Disney company hierarchy Jayne grandes
Jayne grandes Christopher jayne
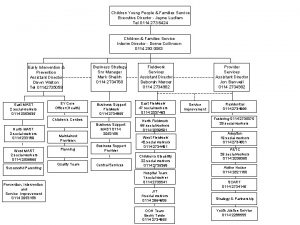
Christopher jayne Jayne ludlam
Jayne ludlam Jayne brookman
Jayne brookman Jayne masters
Jayne masters Jayne reuben
Jayne reuben Jayne todd
Jayne todd Jayne phillips
Jayne phillips Miller index examples
Miller index examples Dbu writing center
Dbu writing center Medical plaza miller 131 miller street
Medical plaza miller 131 miller street Sanitary well definition
Sanitary well definition Eat well stay well
Eat well stay well Eat well live well
Eat well live well The part can never be well unless the whole is well
The part can never be well unless the whole is well Is a collection of well-defined objects.
Is a collection of well-defined objects.