IR and Hyperinsulinemia Insulin Resistance A Survival Mechanism




- Slides: 12
IR and Hyperinsulinemia Insulin Resistance: A Survival Mechanism, Gone Awry Part 1 Stan Schwartz MD, FACP Affiliate, Main Line Health System Emeritus, Clinical Associate Professor of Medicine, U of Pa. stschwar@gmail. com
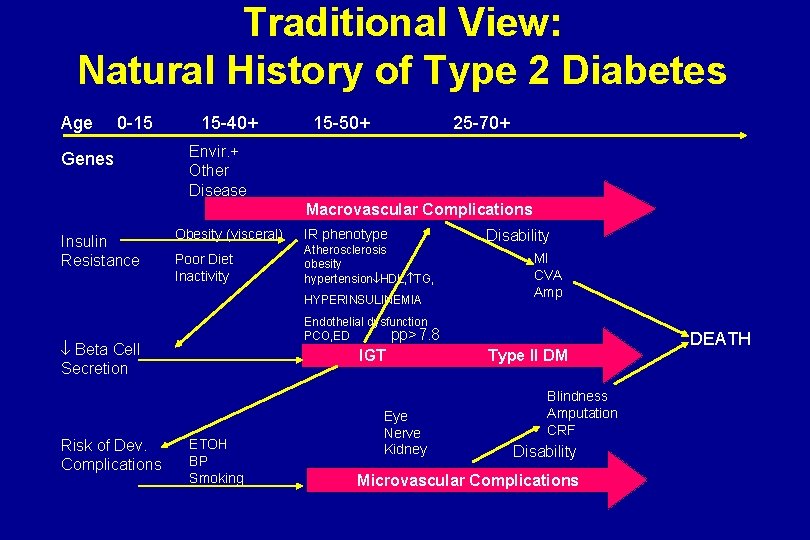
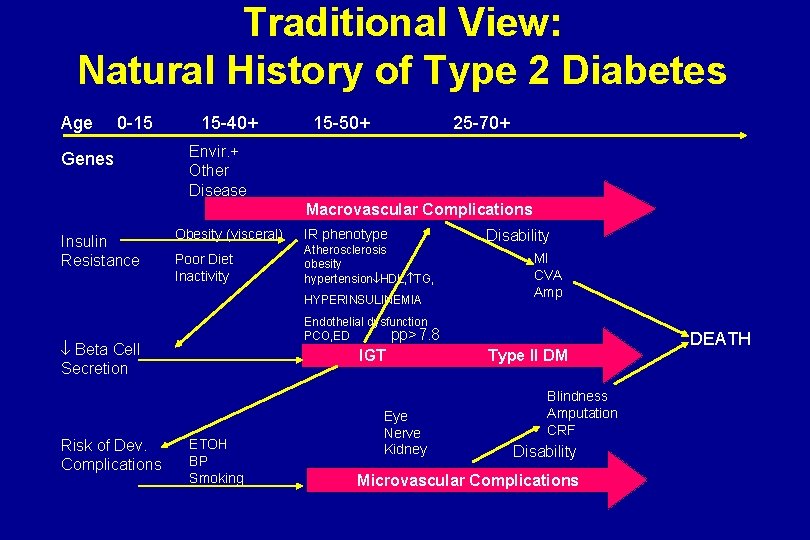
Traditional View: Natural History of Type 2 Diabetes Age 0 -15 Genes 15 -40+ 15 -50+ 25 -70+ Envir. + Other Disease Macrovascular Complications Insulin Resistance Obesity (visceral) IR phenotype Poor Diet Inactivity Atherosclerosis obesity hypertension HDL, TG, HYPERINSULINEMIA MI CVA Amp Endothelial dysfunction pp>7. 8 PCO, ED Beta Cell Secretion Risk of Dev. Complications Disability IGT ETOH BP Smoking Eye Nerve Kidney Type II DM Blindness Amputation CRF Disability Microvascular Complications DEATH

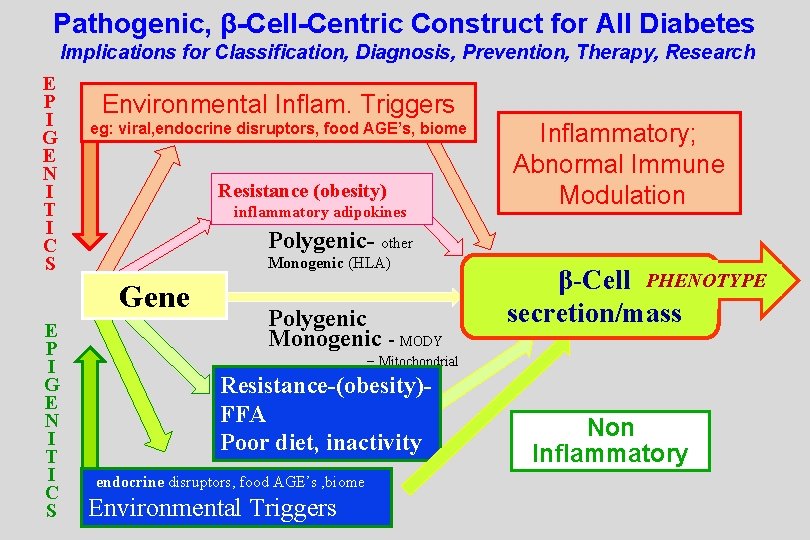
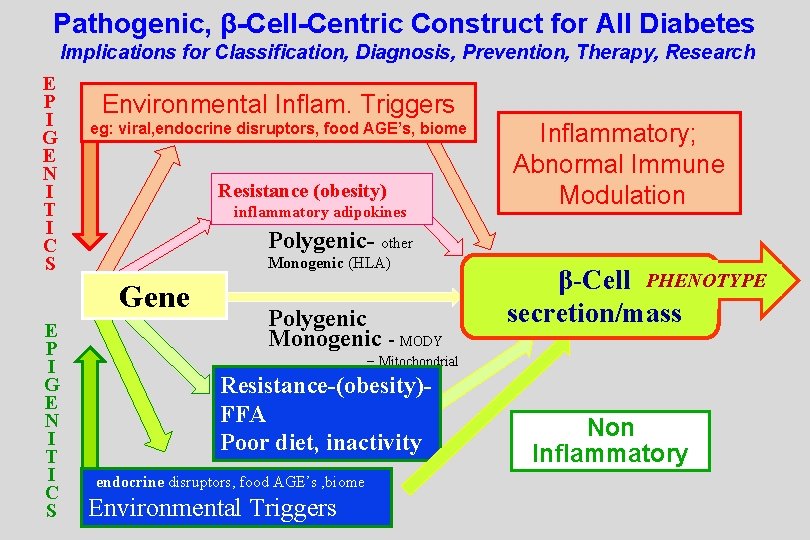
Pathogenic, β-Cell-Centric Construct for All Diabetes Implications for Classification, Diagnosis, Prevention, Therapy, Research E P I G E N I T I C S Environmental Inflam. Triggers eg: viral, endocrine disruptors, food AGE’s, biome Resistance (obesity) inflammatory adipokines Polygenic- other Monogenic (HLA) Gene E P I G E N I T I C S Inflammatory; Abnormal Immune Modulation Polygenic Monogenic - MODY β-Cell PHENOTYPE secretion/mass − Mitochondrial Resistance-(obesity)FFA Poor diet, inactivity endocrine disruptors, food AGE’s , biome Environmental Triggers Non Inflammatory
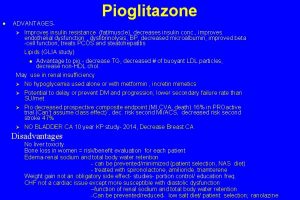
Implications for Therapy · Treat Central Mechanisms IR · Treat Peripheral IR- fat, liver, muscle · Treat Inflammation · Treat Biome
Insulin Resistance- Provide Substrate for the Brain a. Increased liver production sugar b. Decreased peripheral Glucose Uptake c. Increased production FFA from Adipose tissue (alternate fuel source) 1. But potential for Maladaptive Effects of IR on Body if A. Biologic Clock Dysfunction B Peripheral IR causes HYPERINSULINEMIAincreases MAP-kinase pathway- cytokines , etc inc ASCVD risk factors C. Visceral Adipose tissue 1. excessive FFA release, decrease b-cell function= lipotoxicity in genetically susceptible perrson, inc. risk/severity DM 2. D. adipocytokines increase inflammation, endothelial dysfunction
Insulin Resistance a. Increased liver production sugar b. Decreased peripheral Glucose Uptake c. Increased production FFA from Adipose tissue (alternate fuel source) 1. But potential for Maladaptive Effects of IR on Body if A. Biologic Clock Dysfunction B Peripheral IR causes HYPERINSULINEMIAincreases MAP-kinase pathway- cytokines , etc inc ASCVD risk factors C. Visceral Adipose tissue 1. excessive FFA release, decrease b-cell function= lipotoxicity in genetically susceptible perrson, inc. risk/severity DM 2. D. adipocytokines increase inflammation, endothelial dysfunction
Central Insulin Resistance (IR) a. Increased liver production sugar b. Decreased peripheral Glucose Uptake c. Increased production FFA from Liver and Adipose tissue (alternate fuel source) 1. Normal Response to Hibernation, Migration, Periods of Food lack!! BUT ALSO, Normal DIURNAL VARIATION IN INSULIN SENSITIVITY 2. Centrally Induced IR Exacerbated by: obesity, high fat diets, high CHO diets, abnormal sleep cycle, decreased exercise: translates to IR all day long



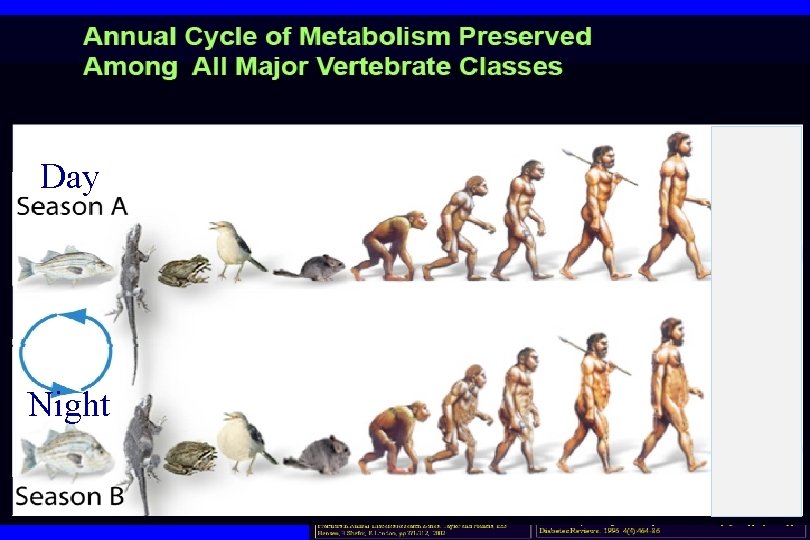
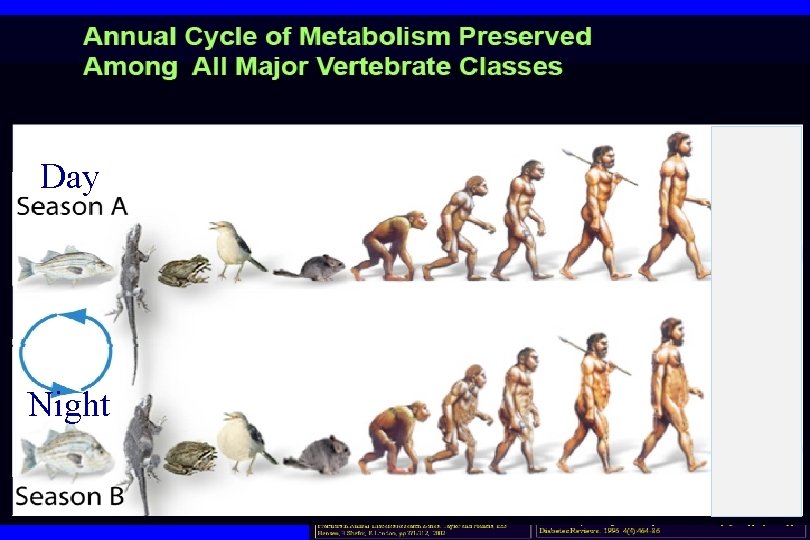
Day Night
 Print pushing eye exercise
Print pushing eye exercise Insulin and insulin receptor
Insulin and insulin receptor Insulin and insulin receptor
Insulin and insulin receptor State of survival survival of the fittest tweak
State of survival survival of the fittest tweak State of survival survival of the fittest stages
State of survival survival of the fittest stages Insulin resistance
Insulin resistance Insulin resistance
Insulin resistance Diagnosis of insulin resistance
Diagnosis of insulin resistance Mechanism insulin action
Mechanism insulin action 2-h pg
2-h pg Constant rate filtration example
Constant rate filtration example What is a force that opposes motion through direct contact
What is a force that opposes motion through direct contact Insulin and sodium retention
Insulin and sodium retention