Implementing pretransplant performance review by the Membership and
Implementing pre-transplant performance review by the Membership and Professional Standards Committee Membership & Professional Standards Committee Fall 2014
The Problem § Performance review includes only post-transplant performance and functional inactivity § Unbalanced review of transplant programs § Previous high profile incidences of waiting list mismanagement

Goal of the Proposal § Need tool to identify and review programs that need pre-transplant performance improvement § Areas to monitor: § § § Acceptance of deceased donor organ offers Transplantation of patients on the waiting list Mitigation of waiting list mortality
How the Proposal will Achieve its Goal § Use composite pre-transplant metric (CPM) that includes: § § § Waiting list mortality rates (liver programs) Geography-adjusted transplant rates Organ offer acceptance rates § Safety net metric based on waiting list mortality § Identify outlier programs that may need pretransplant performance review § Balanced program performance review
Long Term Effort § July 2009 - CPM concept initially presented to MPSC § CPM work group § December 2011 - pilot and survey § Presentations/Discussions § § § American Transplant Congress Transplant Management Forum PSR Consensus Conference
Composite Metric? § Incorporate acceptance rates but temper impact § No single metric fully represents pre-transplant performance § Mitigates effect of geography § Identifies programs needing improvement that would not be identified by single metric § Summary statistic to prioritize MPSC resources
Alternative Approaches Considered § Using acceptance rates alone § Using transplant rates alone § Using independent acceptance, transplant, and mortality rate thresholds § Life Years from Listing (LYFL) § CUSUM –potential complementary tool to CPM in the future
Other Key Decision Points § Weighting the CPM sub-components § Accounting for varying sample sizes among programs § Adjusting for geography (supply-to-demand) § Including both living and deceased donor transplants § Including both active and inactive patients § Choosing a threshold for identifying programs § Use of a “safety net”
Thresholds for Identification § Review transplant program based on pre-transplant performance if the program meets either of the following criteria over a 1 -year period: § § CPM >1. 5 waiting list mortality rate O/E ratio > 2. 0 and one-sided pvalue < 0. 05 § At first, only liver and kidney programs § In an example analysis, 14 programs were newly identified for review
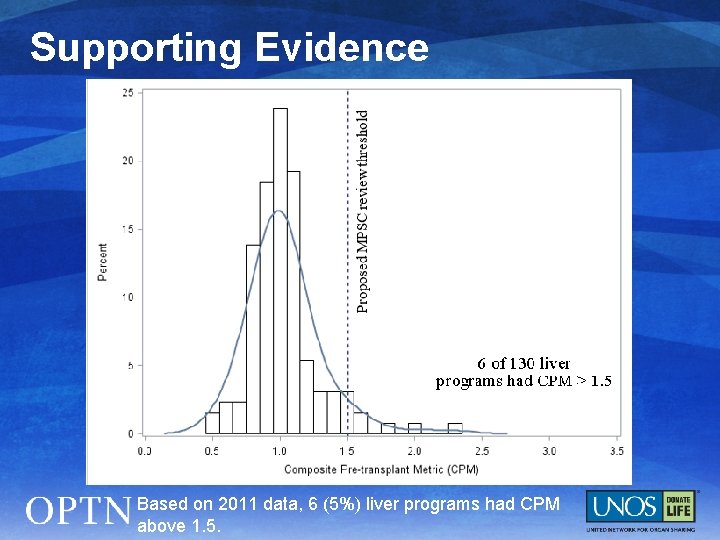
Supporting Evidence Based on 2011 data, 6 (5%) liver programs had CPM above 1. 5.
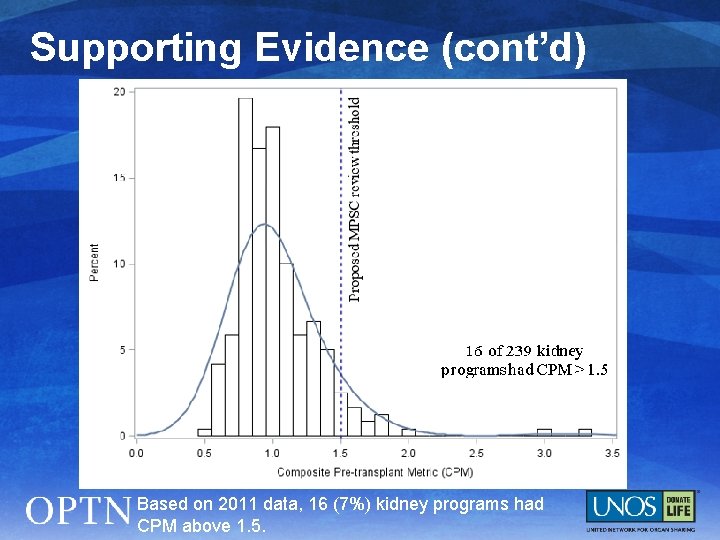
Supporting Evidence (cont’d) Based on 2011 data, 16 (7%) kidney programs had CPM above 1. 5.
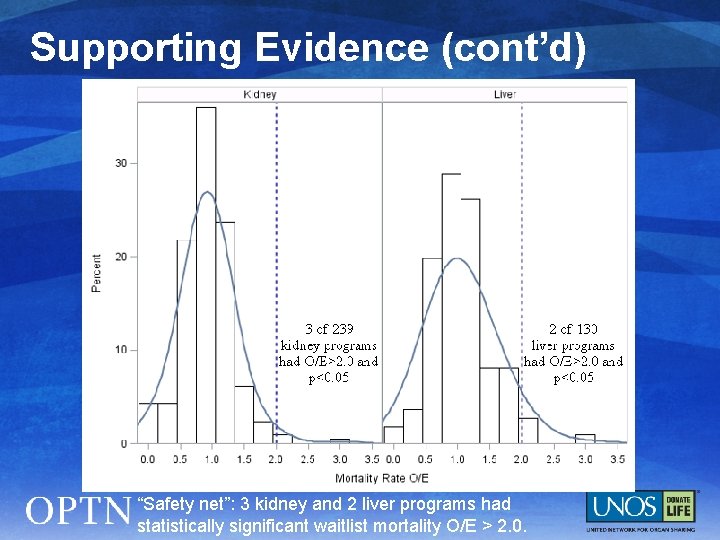
Supporting Evidence (cont’d) “Safety net”: 3 kidney and 2 liver programs had statistically significant waitlist mortality O/E > 2. 0.
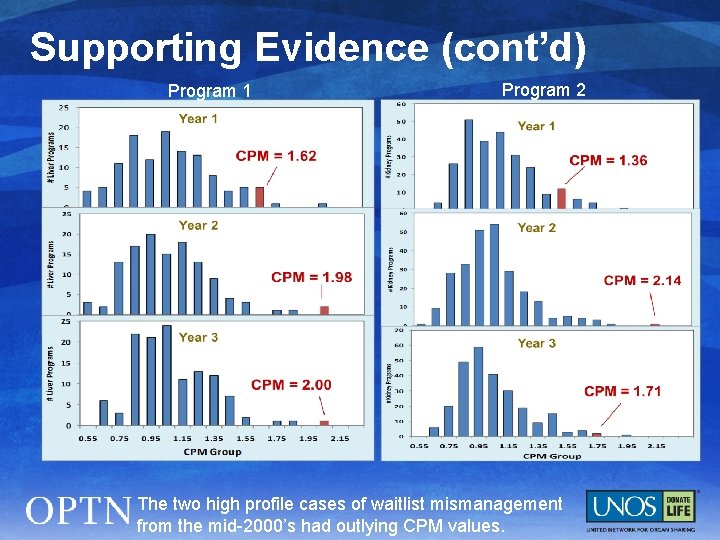
Supporting Evidence (cont’d) Program 1 Program 2 The two high profile cases of waitlist mismanagement from the mid-2000’s had outlying CPM values.
What Members will Need to Do § No additional data submission for CPM analysis § Respond to inquiry from MPSC if identified for review. Will request information on: § § waiting list management process any unique clinical aspects (i. e. , potential mitigating factors) that may influence ability to meet the thresholds
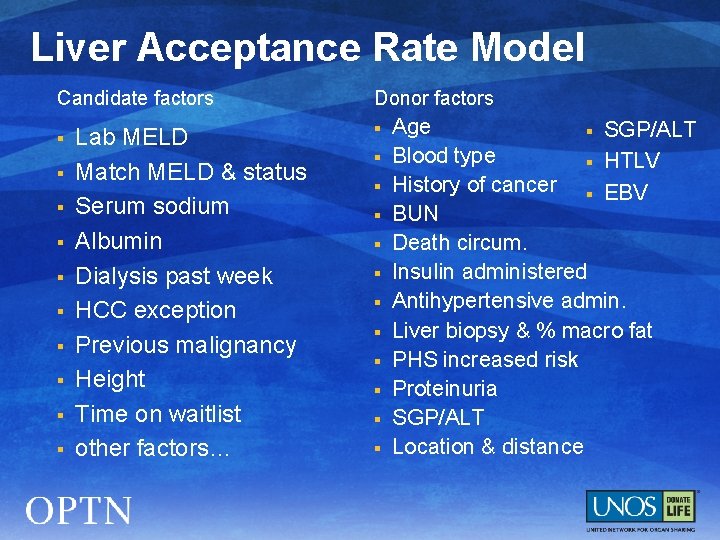
Liver Acceptance Rate Model Candidate factors § § § § § Lab MELD Match MELD & status Serum sodium Albumin Dialysis past week HCC exception Previous malignancy Height Time on waitlist other factors… Donor factors § § § Age § SGP/ALT Blood type § HTLV History of cancer § EBV BUN Death circum. Insulin administered Antihypertensive admin. Liver biopsy & % macro fat PHS increased risk Proteinuria SGP/ALT Location & distance
Questions? § Jonathan Chen, M. D. Committee Chair jonathan. chen@seattlechildrens. org § Regional representative name (RA will complete) Region X Representative email address § Sharon Shepherd Committee Liaison sharon. shepherd@unos. org
- Slides: 16