Clinicians Guide to PreTransplant Evaluation and Management of
- Slides: 3
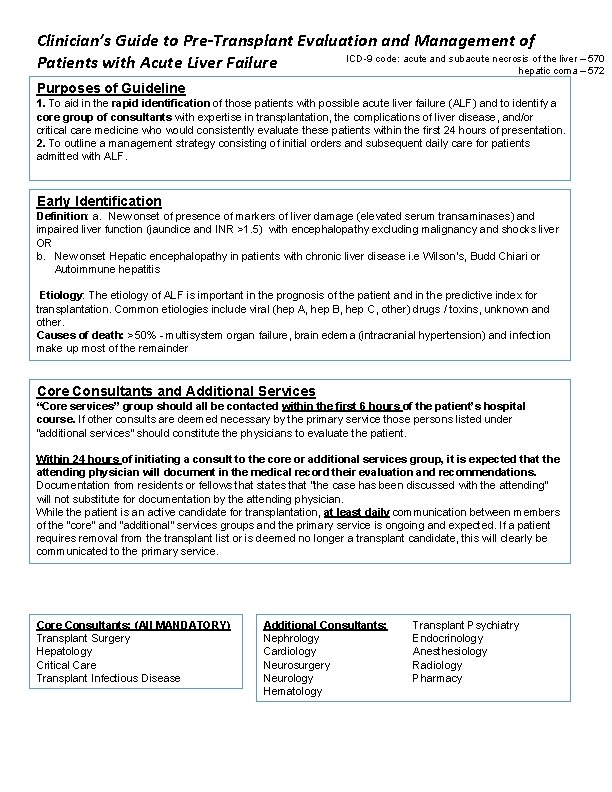
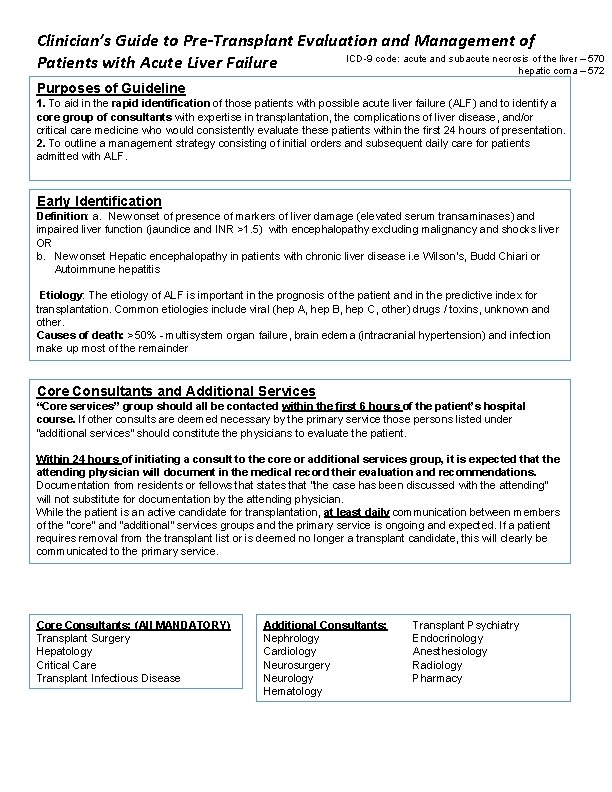
Clinician’s Guide to Pre-Transplant Evaluation and Management of ICD-9 code: acute and subacute necrosis of the liver – 570 Patients with Acute Liver Failure hepatic coma – 572 Purposes of Guideline 1. To aid in the rapid identification of those patients with possible acute liver failure (ALF) and to identify a core group of consultants with expertise in transplantation, the complications of liver disease, and/or critical care medicine who would consistently evaluate these patients within the first 24 hours of presentation. 2. To outline a management strategy consisting of initial orders and subsequent daily care for patients admitted with ALF. Early Identification Definition: a. New onset of presence of markers of liver damage (elevated serum transaminases) and impaired liver function (jaundice and INR >1. 5) with encephalopathy excluding malignancy and shocks liver OR b. New onset Hepatic encephalopathy in patients with chronic liver disease i. e Wilson’s, Budd Chiari or Autoimmune hepatitis Etiology: The etiology of ALF is important in the prognosis of the patient and in the predictive index for transplantation. Common etiologies include viral (hep A, hep B, hep C, other) drugs / toxins, unknown and other. Causes of death: >50% - multisystem organ failure, brain edema (intracranial hypertension) and infection make up most of the remainder Core Consultants and Additional Services “Core services” group should all be contacted within the first 6 hours of the patient’s hospital course. If other consults are deemed necessary by the primary service those persons listed under “additional services” should constitute the physicians to evaluate the patient. Within 24 hours of initiating a consult to the core or additional services group, it is expected that the attending physician will document in the medical record their evaluation and recommendations. Documentation from residents or fellows that states that “the case has been discussed with the attending” will not substitute for documentation by the attending physician. While the patient is an active candidate for transplantation, at least daily communication between members of the “core“ and “additional” services groups and the primary service is ongoing and expected. If a patient requires removal from the transplant list or is deemed no longer a transplant candidate, this will clearly be communicated to the primary service. Core Consultants: (All MANDATORY) Transplant Surgery Hepatology Critical Care Transplant Infectious Disease Additional Consultants: Nephrology Cardiology Neurosurgery Neurology Hematology Transplant Psychiatry Endocrinology Anesthesiology Radiology Pharmacy
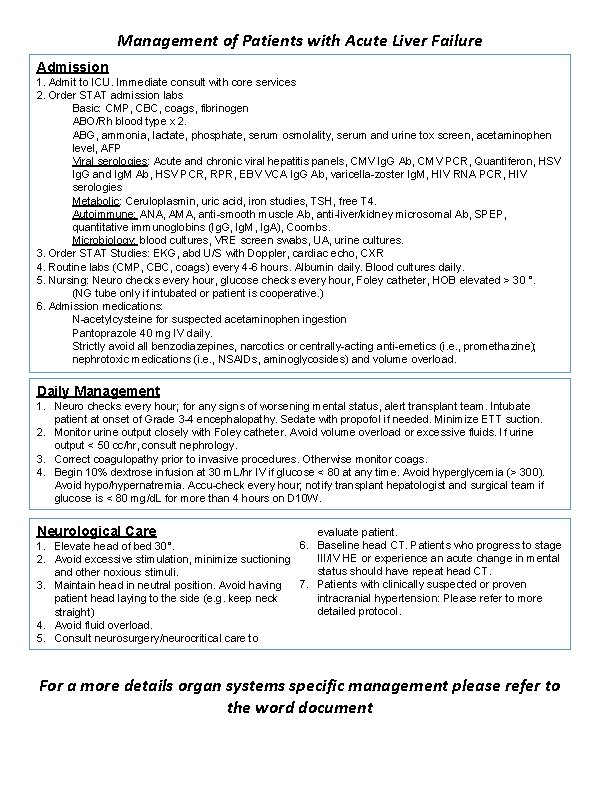
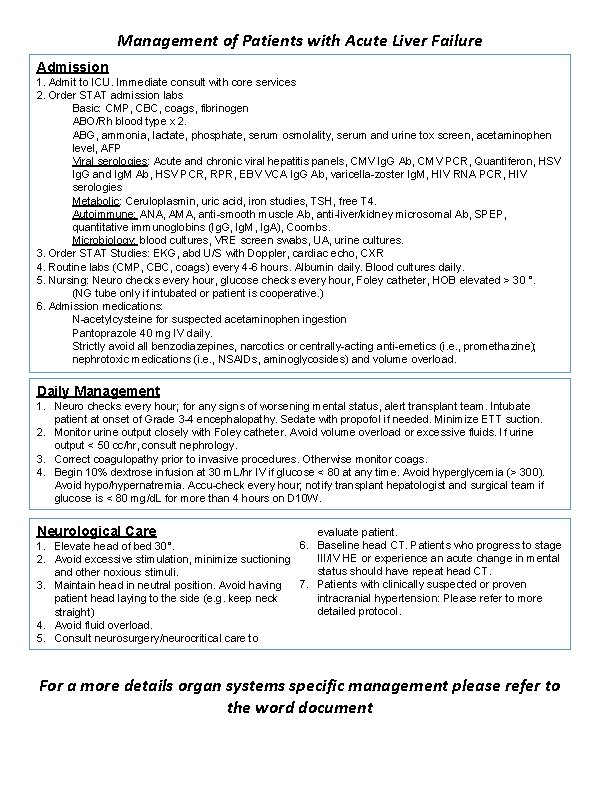
Management of Patients with Acute Liver Failure Admission 1. Admit to ICU. Immediate consult with core services 2. Order STAT admission labs Basic: CMP, CBC, coags, fibrinogen ABO/Rh blood type x 2. ABG, ammonia, lactate, phosphate, serum osmolality, serum and urine tox screen, acetaminophen level, AFP Viral serologies: Acute and chronic viral hepatitis panels, CMV Ig. G Ab, CMV PCR, Quantiferon, HSV Ig. G and Ig. M Ab, HSV PCR, RPR, EBV VCA Ig. G Ab, varicella-zoster Ig. M, HIV RNA PCR, HIV serologies Metabolic: Ceruloplasmin, uric acid, iron studies, TSH, free T 4. Autoimmune: ANA, AMA, anti-smooth muscle Ab, anti-liver/kidney microsomal Ab, SPEP, quantitative immunoglobins (Ig. G, Ig. M, Ig. A), Coombs. Microbiology: blood cultures, VRE screen swabs, UA, urine cultures. 3. Order STAT Studies: EKG, abd U/S with Doppler, cardiac echo, CXR 4. Routine labs (CMP, CBC, coags) every 4 -6 hours. Albumin daily. Blood cultures daily. 5. Nursing: Neuro checks every hour, glucose checks every hour, Foley catheter, HOB elevated > 30 °. (NG tube only if intubated or patient is cooperative. ) 6. Admission medications: N-acetylcysteine for suspected acetaminophen ingestion Pantoprazole 40 mg IV daily. Strictly avoid all benzodiazepines, narcotics or centrally-acting anti-emetics (i. e. , promethazine); nephrotoxic medications (i. e. , NSAIDs, aminoglycosides) and volume overload. Daily Management 1. Neuro checks every hour; for any signs of worsening mental status, alert transplant team. Intubate patient at onset of Grade 3 -4 encephalopathy. Sedate with propofol if needed. Minimize ETT suction. 2. Monitor urine output closely with Foley catheter. Avoid volume overload or excessive fluids. If urine output < 50 cc/hr, consult nephrology. 3. Correct coagulopathy prior to invasive procedures. Otherwise monitor coags. 4. Begin 10% dextrose infusion at 30 m. L/hr IV if glucose < 80 at any time. Avoid hyperglycemia (> 300). Avoid hypo/hypernatremia. Accu-check every hour; notify transplant hepatologist and surgical team if glucose is < 80 mg/d. L for more than 4 hours on D 10 W. Neurological Care 1. 2. 3. 4. 5. evaluate patient. 6. Baseline head CT. Patients who progress to stage Elevate head of bed 30°. III/IV HE or experience an acute change in mental Avoid excessive stimulation, minimize suctioning status should have repeat head CT. and other noxious stimuli. 7. Patients with clinically suspected or proven Maintain head in neutral position. Avoid having intracranial hypertension: Please refer to more patient head laying to the side (e. g. keep neck detailed protocol. straight) Avoid fluid overload. Consult neurosurgery/neurocritical care to For a more details organ systems specific management please refer to the word document
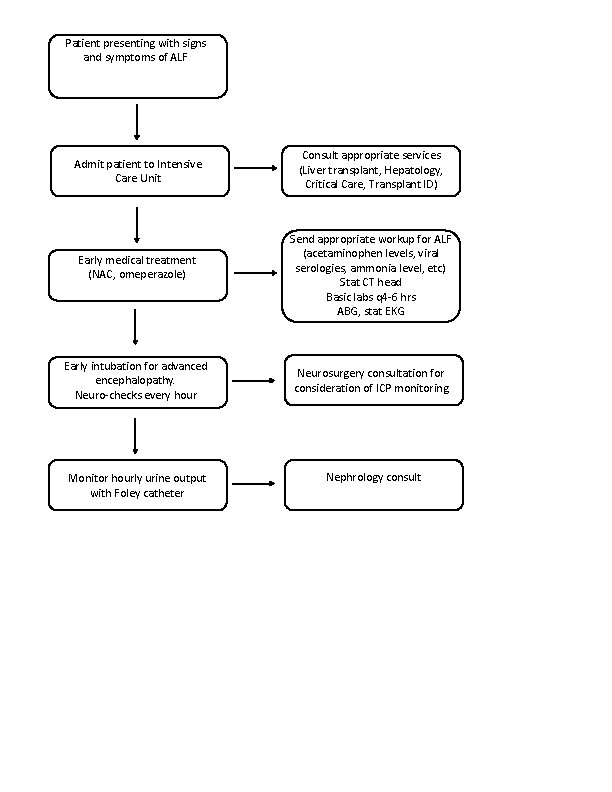
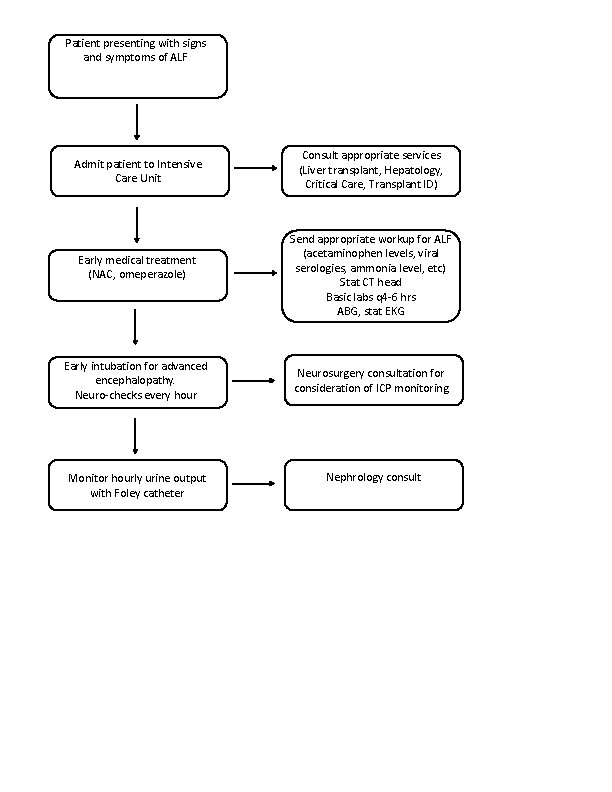
Patient presenting with signs and symptoms of ALF Admit patient to Intensive Care Unit Early medical treatment (NAC, omeperazole) Early intubation for advanced encephalopathy. Neuro-checks every hour Monitor hourly urine output with Foley catheter Consult appropriate services (Liver transplant, Hepatology, Critical Care, Transplant ID) Send appropriate workup for ALF (acetaminophen levels, viral serologies, ammonia level, etc) Stat CT head Basic labs q 4 -6 hrs ABG, stat EKG Neurosurgery consultation for consideration of ICP monitoring Nephrology consult