Health Promoting Hospitals PATHWAYS OF INTEGRATED CARE FOR


- Slides: 21
Health Promoting Hospitals PATHWAYS OF INTEGRATED CARE FOR PATIENTS AFFECTED BY HEART FAILURE Mariella Martini Coordinator of HPH Emilia Romagna Regional Network 1
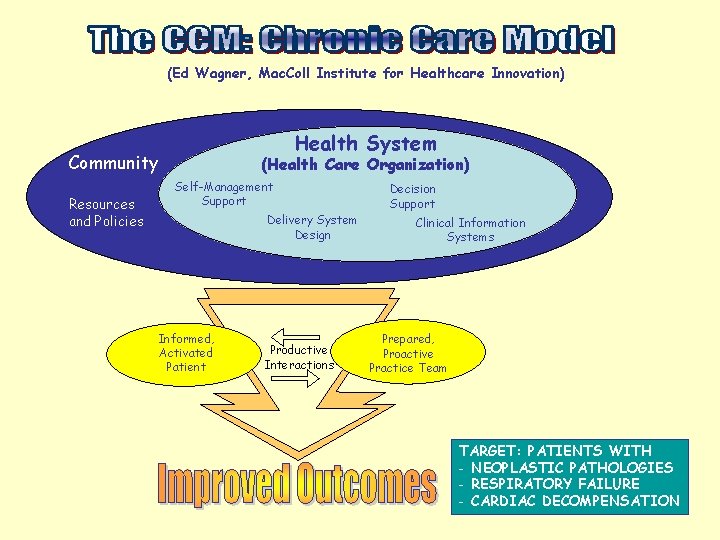
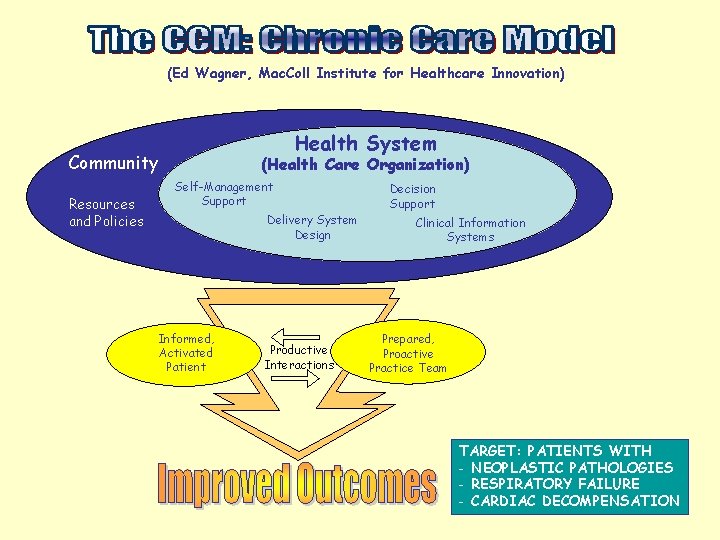
(Ed Wagner, Mac. Coll Institute for Healthcare Innovation) Health System Community Resources and Policies (Health Care Organization) Self-Management Support Delivery System Design Informed, Activated Patient Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team TARGET: PATIENTS WITH - NEOPLASTIC PATHOLOGIES - RESPIRATORY FAILURE - CARDIAC DECOMPENSATION
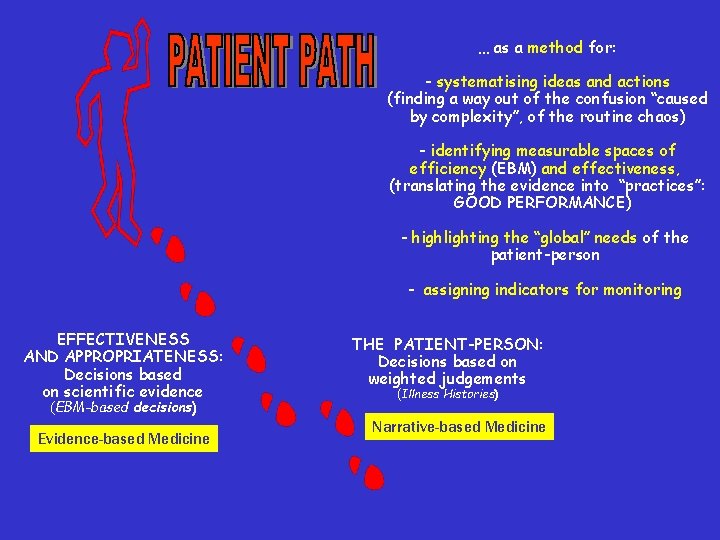
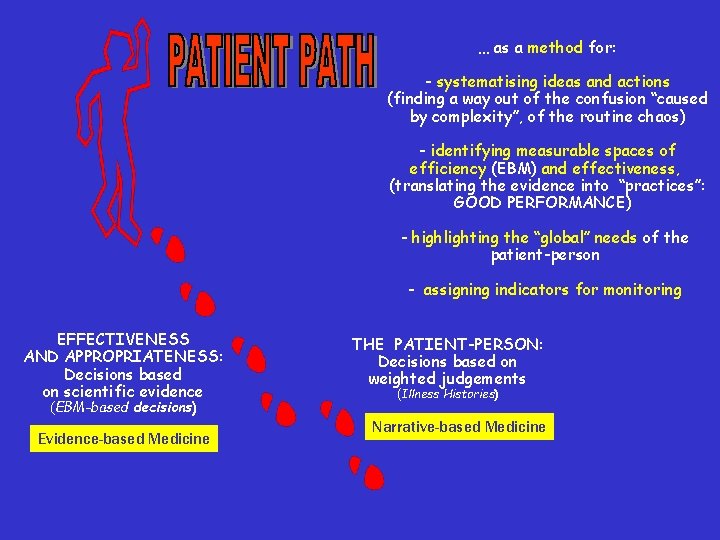
… as a method for: - systematising ideas and actions (finding a way out of the confusion “caused by complexity”, of the routine chaos) - identifying measurable spaces of efficiency (EBM) and effectiveness, (translating the evidence into “practices”: GOOD PERFORMANCE) - highlighting the “global” needs of the patient-person - assigning indicators for monitoring EFFECTIVENESS AND APPROPRIATENESS: Decisions based on scientific evidence (EBM-based decisions) Evidence-based Medicine THE PATIENT-PERSON: Decisions based on weighted judgements (Illness Histories) Narrative-based Medicine
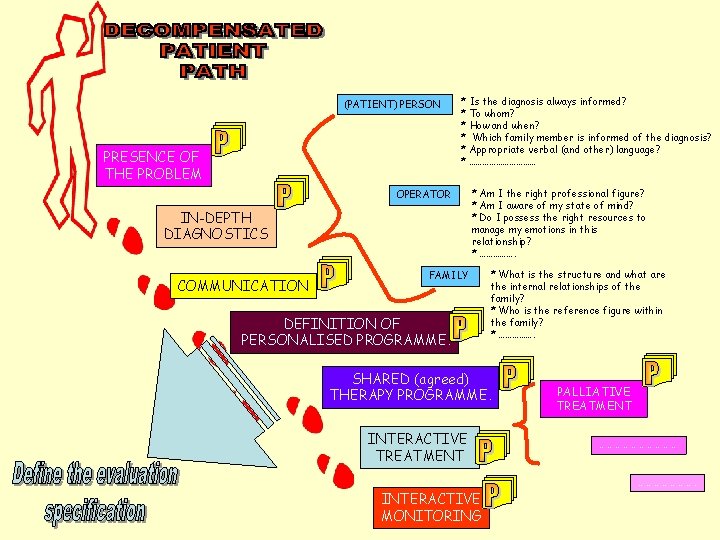
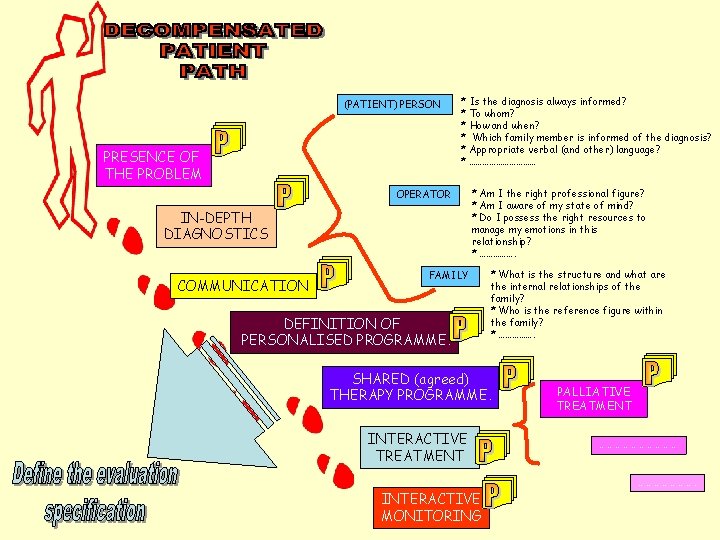
(PATIENT) PERSON PRESENCE OF THE PROBLEM * Is the diagnosis always informed? * To whom? * How and when? * Which family member is informed of the diagnosis? * Appropriate verbal (and other) language? * …………… OPERATOR IN-DEPTH DIAGNOSTICS COMMUNICATION * Am I the right professional figure? * Am I aware of my state of mind? * Do I possess the right resources to manage my emotions in this relationship? * ……………. FAMILY DEFINITION OF PERSONALISED PROGRAMME. * What is the structure and what are the internal relationships of the family? * Who is the reference figure within the family? * ……………. SHARED (agreed) THERAPY PROGRAMME. INTERACTIVE TREATMENT PALLIATIVE TREATMENT …………………. INTERACTIVE MONITORING
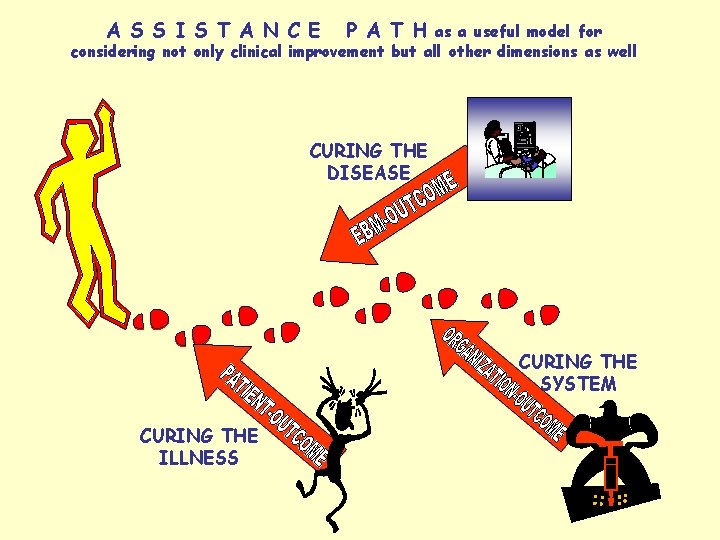
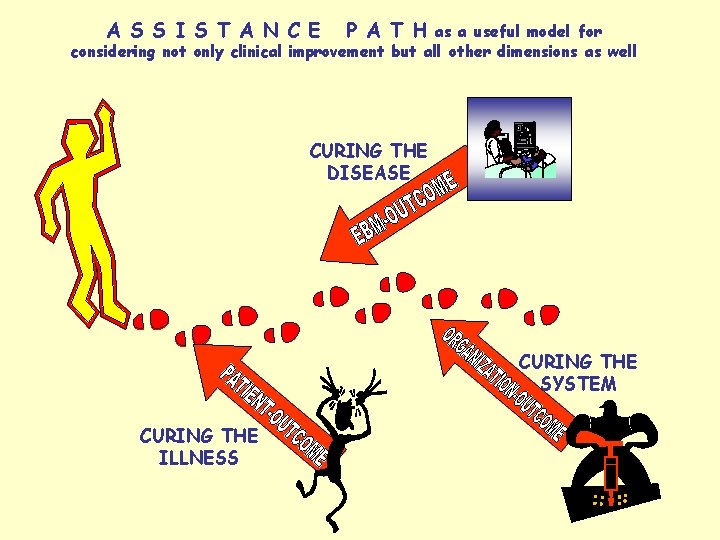
A S S I S T A N C E P A T H as a useful model for considering not only clinical improvement but all other dimensions as well CURING THE DISEASE CURING THE SYSTEM CURING THE ILLNESS
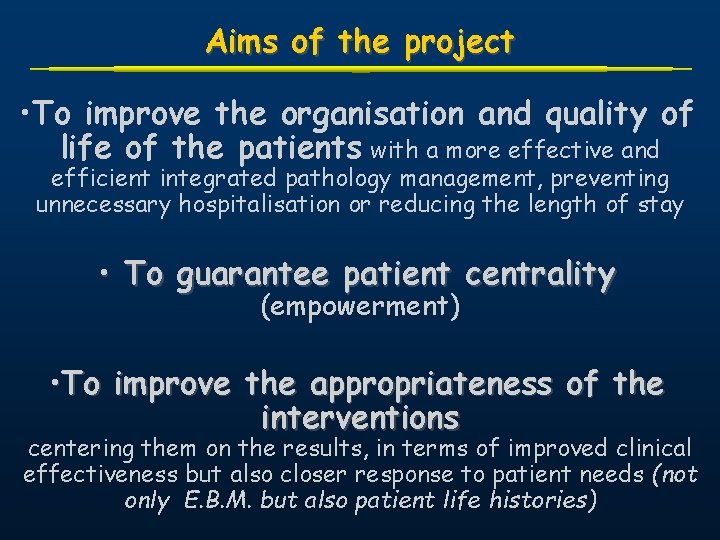
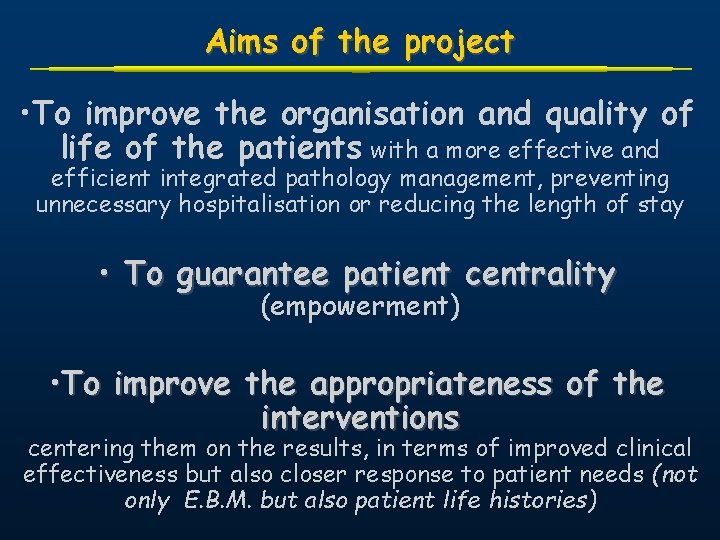
Aims of the project • To improve the organisation and quality of life of the patients with a more effective and efficient integrated pathology management, preventing unnecessary hospitalisation or reducing the length of stay • To guarantee patient centrality (empowerment) • To improve the appropriateness of the interventions centering them on the results, in terms of improved clinical effectiveness but also closer response to patient needs (not only E. B. M. but also patient life histories)
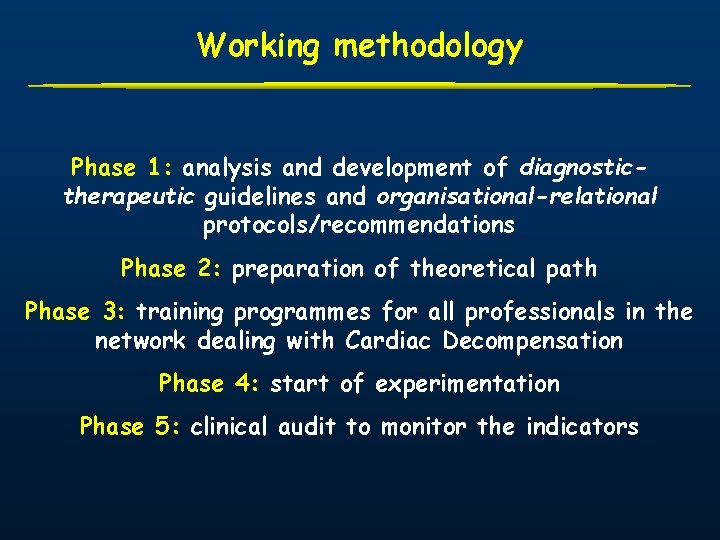
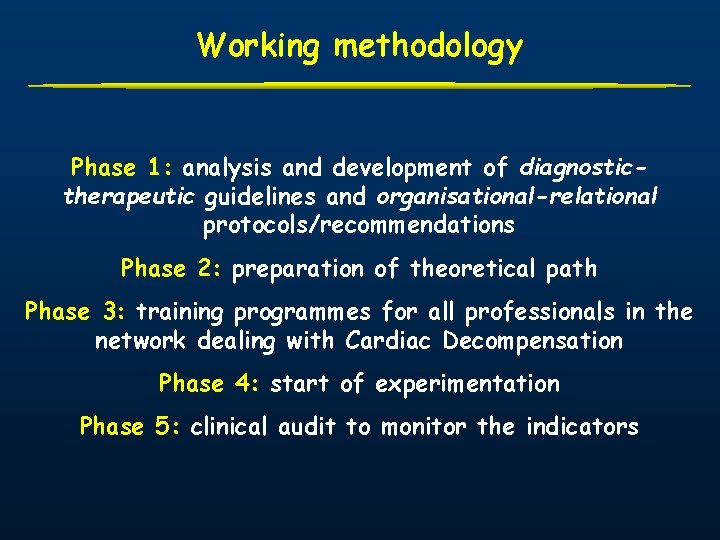
Working methodology Phase 1: analysis and development of diagnostictherapeutic guidelines and organisational-relational protocols/recommendations Phase 2: preparation of theoretical path Phase 3: training programmes for all professionals in the network dealing with Cardiac Decompensation Phase 4: start of experimentation Phase 5: clinical audit to monitor the indicators
Working tools/1 üDiagnostic-therapeutic guidelines and organisational-relational recommendations ü Path flow-chart ü Follow up sheet

Decompensated patient path PRESENCE OF SYMPTOMS 1 ST DIAGNOSIS GENERAL PRACTITIONER HOSPITAL REFERRAL TO LOCAL / HOSPTIAL SPECIALIST FOR FURTHER INVESTIGATIONS NO NYHA I CLASS INVESTIGATIONS DECO MPEN SATI ON YES NYHA II CLASS NYHA IV CLASS
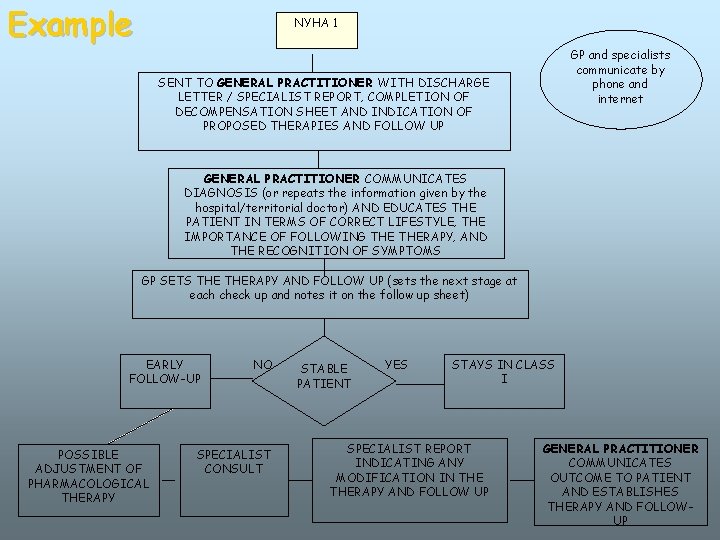
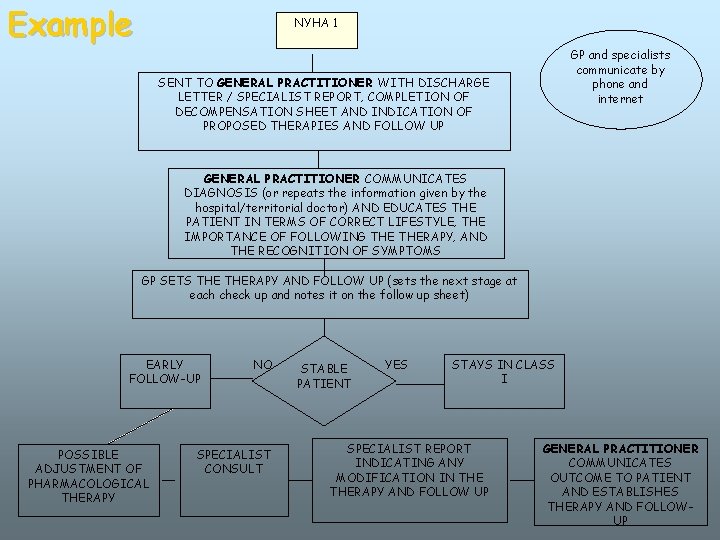
Example NYHA 1 GP and specialists communicate by phone and internet SENT TO GENERAL PRACTITIONER WITH DISCHARGE LETTER / SPECIALIST REPORT, COMPLETION OF DECOMPENSATION SHEET AND INDICATION OF PROPOSED THERAPIES AND FOLLOW UP GENERAL PRACTITIONER COMMUNICATES DIAGNOSIS (or repeats the information given by the hospital/territorial doctor) AND EDUCATES THE PATIENT IN TERMS OF CORRECT LIFESTYLE, THE IMPORTANCE OF FOLLOWING THERAPY, AND THE RECOGNITION OF SYMPTOMS GP SETS THERAPY AND FOLLOW UP (sets the next stage at each check up and notes it on the follow up sheet) EARLY FOLLOW-UP POSSIBLE ADJUSTMENT OF PHARMACOLOGICAL THERAPY NO SPECIALIST CONSULT STABLE PATIENT YES STAYS IN CLASS I SPECIALIST REPORT INDICATING ANY MODIFICATION IN THERAPY AND FOLLOW UP GENERAL PRACTITIONER COMMUNICATES OUTCOME TO PATIENT AND ESTABLISHES THERAPY AND FOLLOWUP
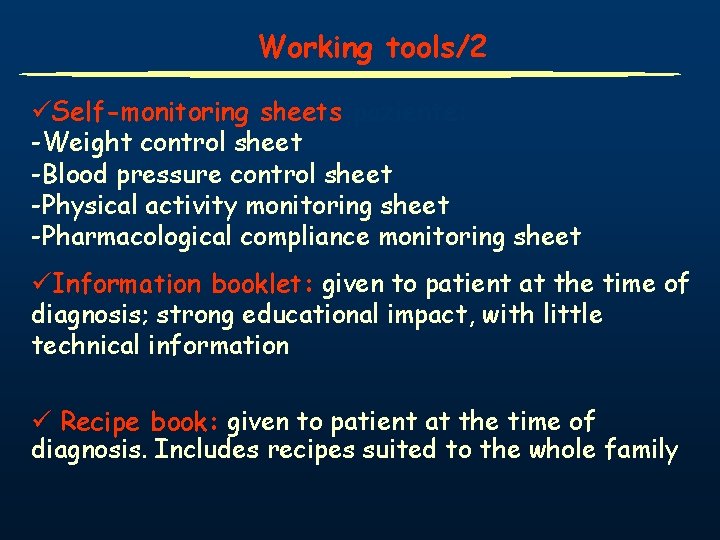
Working tools/2 üSelf-monitoring sheets paziente: -Weight control sheet -Blood pressure control sheet -Physical activity monitoring sheet -Pharmacological compliance monitoring sheet üInformation booklet: given to patient at the time of diagnosis; strong educational impact, with little technical information ü Recipe book: given to patient at the time of diagnosis. Includes recipes suited to the whole family
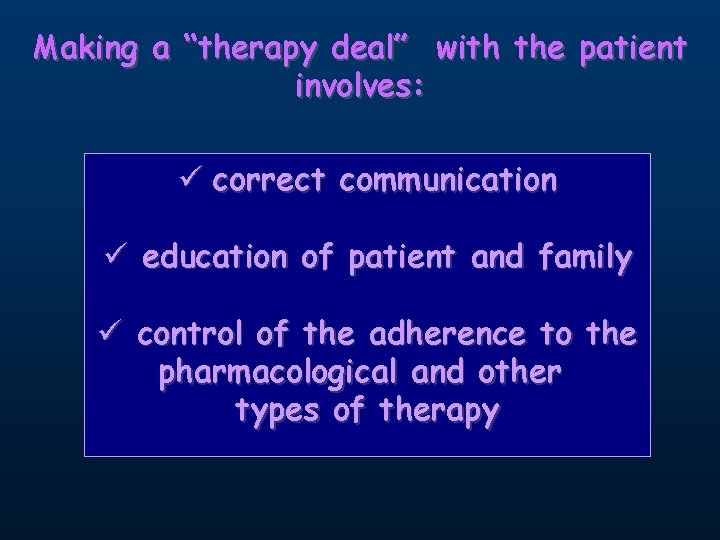
Making a “therapy deal” with the patient involves: ü correct communication ü education of patient and family ü control of the adherence to the pharmacological and other types of therapy
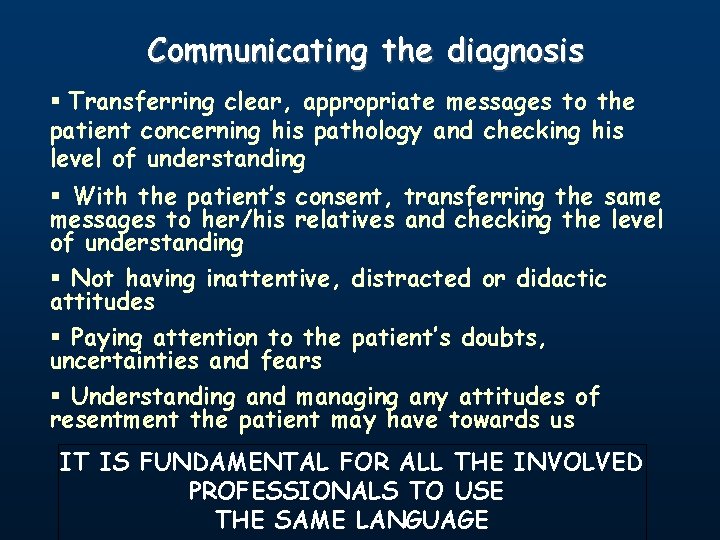
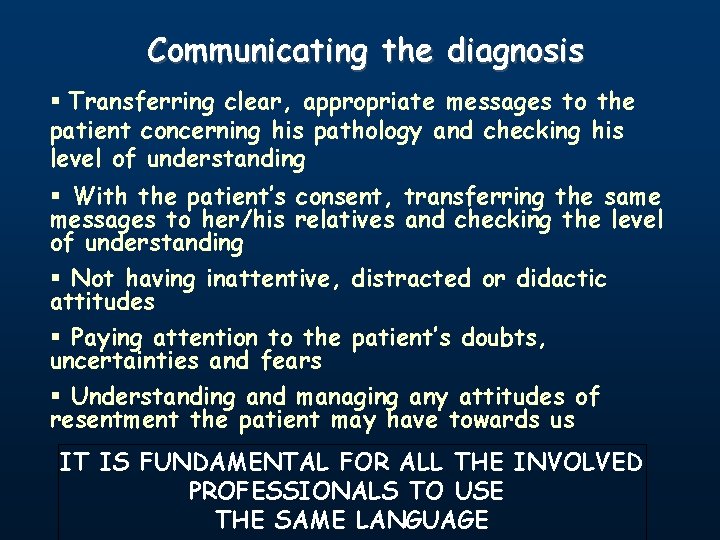
Communicating the diagnosis § Transferring clear, appropriate messages to the patient concerning his pathology and checking his level of understanding § With the patient’s consent, transferring the same messages to her/his relatives and checking the level of understanding § Not having inattentive, distracted or didactic attitudes § Paying attention to the patient’s doubts, uncertainties and fears § Understanding and managing any attitudes of resentment the patient may have towards us IT IS FUNDAMENTAL FOR ALL THE INVOLVED PROFESSIONALS TO USE THE SAME LANGUAGE
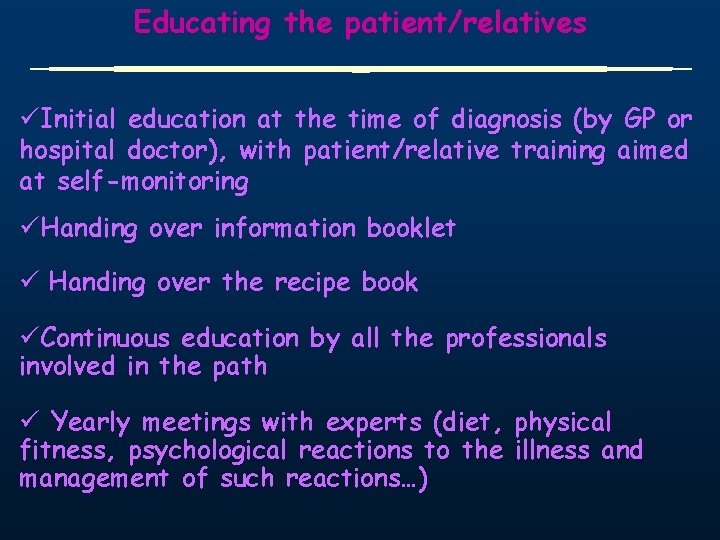
Educating the patient/relatives üInitial education at the time of diagnosis (by GP or hospital doctor), with patient/relative training aimed at self-monitoring üHanding over information booklet ü Handing over the recipe book üContinuous education by all the professionals involved in the path ü Yearly meetings with experts (diet, physical fitness, psychological reactions to the illness and management of such reactions…)
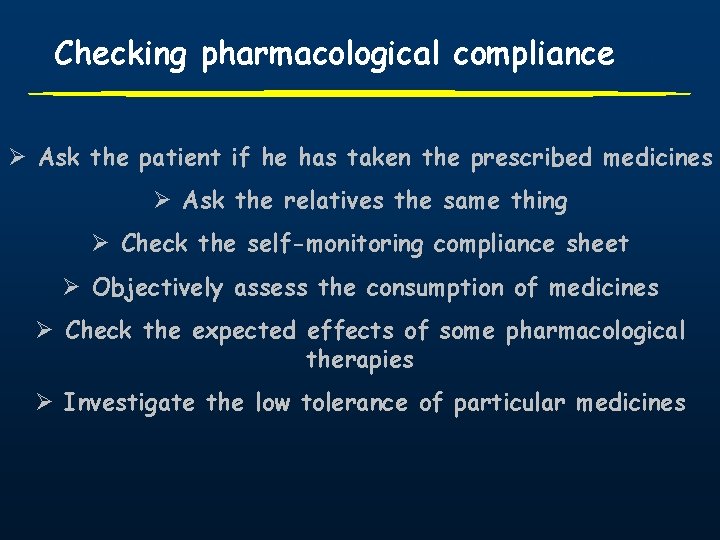
Checking pharmacological compliance…. Ø Ask the patient if he has taken the prescribed medicines Ø Ask the relatives the same thing Ø Check the self-monitoring compliance sheet Ø Objectively assess the consumption of medicines Ø Check the expected effects of some pharmacological therapies Ø Investigate the low tolerance of particular medicines
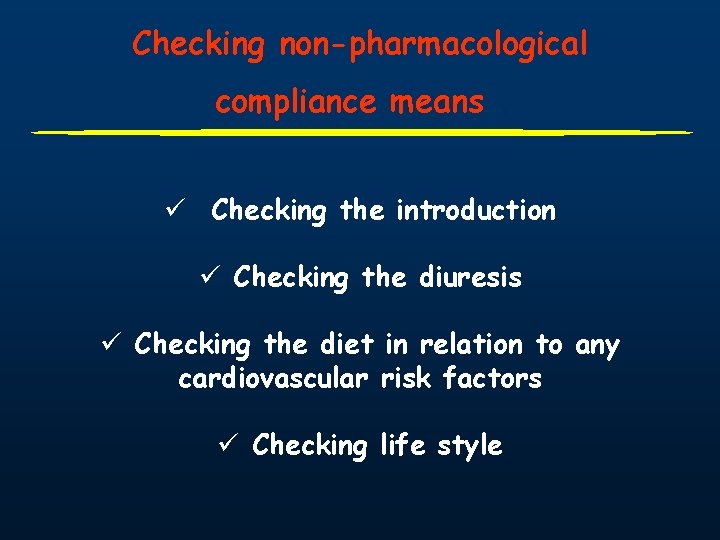
Checking non-pharmacological compliance means…. ü Checking the introduction ü Checking the diuresis ü Checking the diet in relation to any cardiovascular risk factors ü Checking life style
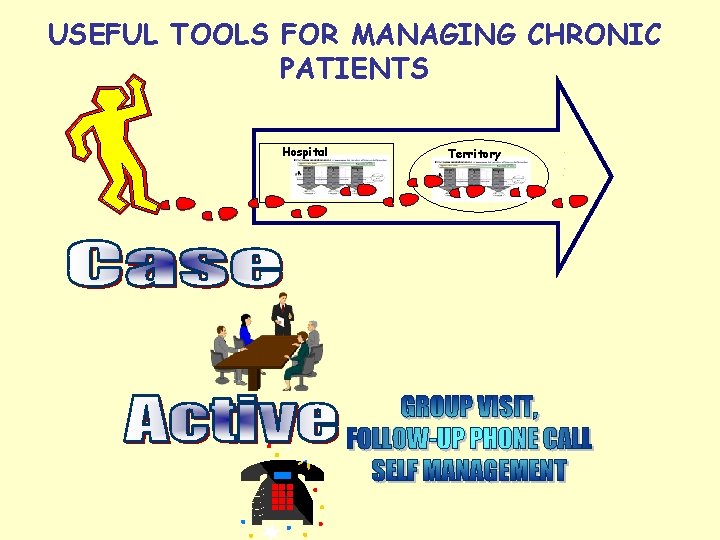
USEFUL TOOLS FOR MANAGING CHRONIC PATIENTS Hospital Territory
IN GOD WE TRUST. ALL OTHERS MUST USE DATA. W. E. Deming
WHERE, WHAT, WHEN, HOW… TO EVALUATE?
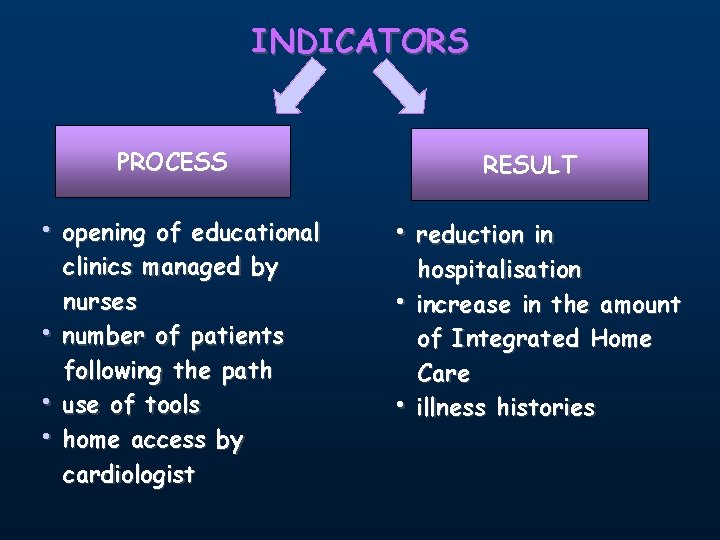
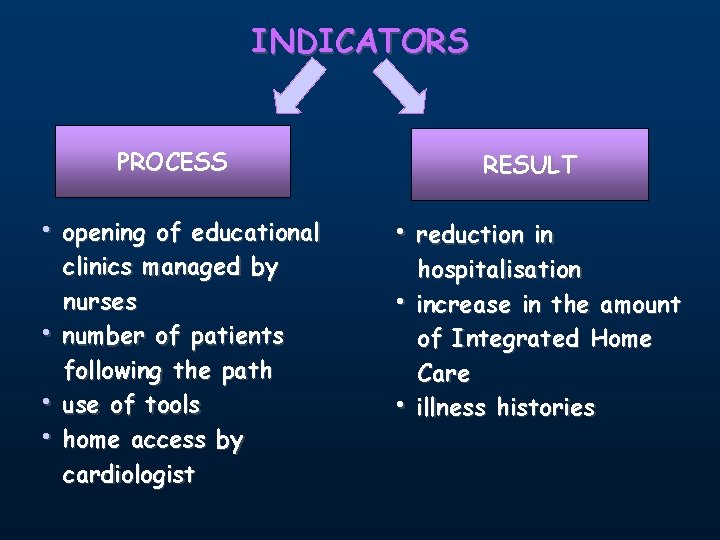
INDICATORS PROCESS • opening of educational • • • clinics managed by nurses number of patients following the path use of tools home access by cardiologist RESULT • reduction in • • hospitalisation increase in the amount of Integrated Home Care illness histories

Accountability
 Support services career pathway
Support services career pathway Example of health care pathways
Example of health care pathways West calcasieu cameron 3767 baton rouge la 70821
West calcasieu cameron 3767 baton rouge la 70821 Promoting excellence in dementia care
Promoting excellence in dementia care Chapter 1 lesson 4 promoting health and wellness
Chapter 1 lesson 4 promoting health and wellness Chapter 1 understanding health and wellness lesson 4
Chapter 1 understanding health and wellness lesson 4 Lesson 4 promoting health and wellness
Lesson 4 promoting health and wellness Keeping an infant safe and well section 7-3
Keeping an infant safe and well section 7-3 Chapter 7 promoting health and wellness
Chapter 7 promoting health and wellness Health promoting schools model
Health promoting schools model Promoting a positive health and safety culture
Promoting a positive health and safety culture Health promoting school
Health promoting school Health and wellness vocabulary
Health and wellness vocabulary Integrated primary health care model
Integrated primary health care model Delirium care pathways
Delirium care pathways Tertiary level of care
Tertiary level of care Health science careers cluster
Health science careers cluster Unit 2 equality diversity and rights
Unit 2 equality diversity and rights Health and social care component 3
Health and social care component 3 Mandatory standards
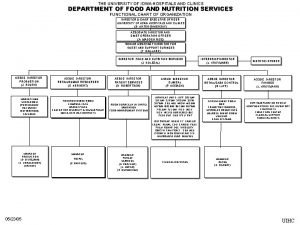
Mandatory standards University of iowa hospitals and clinics
University of iowa hospitals and clinics Portsmouth hospitals nhs trust values
Portsmouth hospitals nhs trust values