Ethics Rights and DoctorPatient Relationship Gender Mainstreaming in
- Slides: 31
Ethics, Rights and Doctor-Patient Relationship Gender Mainstreaming in Medical Education Amar Jesani Indian Journal of Medical Ethics
Presentation covers …. Morality and Ethics principles Needs, Rights & Duties Doctor-Patient Relationship Four models Patients Rights and Empowerment Shift in doctor-patient relationship
Moral Judgments Any judgement that consists of approving or disapproving of an action in such a way that we state our (dis)approval in some sort of detached and quasi objective way. It is about judging an action as good or bad. Such judgments are based on the standard one uses for approving or disapproving an action. Morality and ethics are often used interchangeably, but they could be looked at separately in order to distinguish moral judgments based on considered reasoning from those based on first order beliefs.
Morality refers to the first-order beliefs and practices about good and evil by means of which we guide our behaviour. Morality is made up of a lot of values and duties based on beliefs that people take for granted most of the time. Values describe certain qualities that constitute “a good life”. Duties describe actions in response to claims that are either self-imposed or imposed by others.
Ethics is a second-order, systematic, reflective consideration of our moral beliefs & practices. In other words, it is a conscious stepping back and reflecting on morality. Requires a human 'agent' doing the acting, if not always also a human as the recipient of the action; Moral action requires the capacity in the agent to reason about their action and understand it as moral or immoral; and The agent must be responsible for their action and have the freedom to act otherwise.
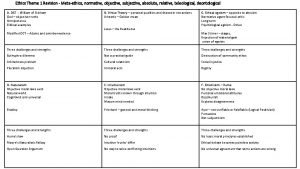
Normative & Non-Normative Ethics Provide prescriptive actions – guides Revolves around principles-used as foundation for resolving specific moral dilemmas. Non-Normative Ethics To establish what factually or conceptually is case, not what ethically ought to be the case. Descriptive: Factual investigation of moral behaviour and beliefs. Meta-ethics: Analysis of meanings of ‘rights’, ‘virtue’, ‘responsibility” etc.
Ethics Theories and Principles They provide tools for analysis, for moral reasoning Theories are general overviews or statements that are based on certain assumptions of rights and wrongs. But often it is not adequate to use one theory for all purposes and contexts. Hence, some useful norms or elements developed that could guide action expressing respect for the dignity of human being – they are called Principles
Theories Deontological Theories (deon = duty) Immanuel Kant (18 th C) Diverse origin (e. g. religion) – divine revelation, intuition, common sense, hypothetical contract Concept of duty is independent of concept of good, and right actions are not determined exclusively by production of non-moral goods. One is acting rightly when one acts according to duties and rights.
Theories Utilitarian Theories Consequentialist (rightness or wrongness of actions depend upon their consequences), Teleological (telos=end) David Hume, Jeremy Bentham, JS Mill Morally right actions are determined by the non-moral value, such as pleasure, happiness, knowledge, health, etc. Utilitarianism: In all circumstance we ought to produce the greatest possible balance of value over disvalue for all persons affected (or the least possible balance of disvalue if only bad result can be brought about)
Feminist approaches or framework Based on the understanding that (a) there is systematic oppression of and discrimination against women, (b) such oppression is morally wrong and unjust. There are different streams of feminism, each having different approaches. More eclectic than having coherent bioethics theory. Instead of separation, bringing women’s concerns into the mainstream
Principles (1) Non-maleficence – (2) Beneficence Non-maleficence Primum non nocere: above all or first, do no harm Beneficence All actions only for prevention of harm, removal of harm and for the provision of benefits Cost/Risk-Benefit Analysis
Principles (3) Autonomy – (4) Justice Autonomy The ability to freely determine one’s own course in life Assumption: An autonomous person determines his/her course of action in accordance with a plan chosen by him/herself. Informed consent Justice How social burden and benefits ought to be allocated – Fairness, Equity, Distributive justice - Resource allocation
Principles (5) Confidentiality – (6) Fidelity – (7) Veracity Confidentiality of information received from patient, client, participant. Absolute and partial confidentiality Fidelity: Latin fides means faithfulness Being faithful to patient entails meeting patient’s reasonable expectations Veracity means that you will tell the truth. Also includes honesty
Doctor – Patient Relationship
Crucial issues in doctor-patient relationship Patients rights – autonomy Unilateral decision making on either side or shared decision making? If shared, what areas of sharing? Doctor restricts only to health related morality or also engage in patient’s personal morality? Is doctor-patient relationship devoid of power relationship?
Four Models (1) Paternalistic (2) Informative (3) Interpretive (4) Deliberative Let us try to understand each by examining – (a) What is it? (b) What does it assume? (c) What is happening?
1. Paternalistic Model What is it? Also called “Parental” or “Priestly” model Doctor determines patient’s medical condition, stage of disease process, identifies the medical tests and treatment Doctor provides selected information to patient that will encourage patient to consent to the proposed intervention At the extreme, doctor authoritatively informs of the intervention to be initiated
1. Paternalistic Model What does it assume? The Doctor and Patient share the same criteria for determining what is best Or that the criteria used by the doctor are the only objective and best criteria Patient will ultimately be thankful for decisions made by the doctor even if not agreed at that time.
1. Paternalistic Model What is happening? Doctor acts as patient’s guardian, articulating and implementing what is best for patient Doctor’s ethics and obligations - include that of placing patient’s interest above his/her own and soliciting the views of others when lacking adequate knowledge Patient autonomy = Patient assent
2. Informative Model What is it? Also called “scientific”, “engineering” or consumer model Doctor provides patient with all relevant information – of disease state, nature of possible diagnostic and therapeutic interventions, probability of risks and benefits and any uncertainty of knowledge. The patient selects the medical intervention s/he consider best suited to his/her values.
2. Informative Model What does it assume? Assumes fairly clear distinction between facts and values – patient knows his/her values but lacks health care facts, so only they are to be provided by doctor No role for doctor’s values, his/her understanding of patient’s values, or his/her judgment of the worth of patient’s values
2. Informative Model What is happening? Doctor is treated merely as technical expert His/her obligation is only to provide truthful and scientific information, to maintain competence in his/her area of expertise, to consult others when lacking in knowledge and skills. Patient autonomy = Patient control over medical decision making.
3. Interpretive Model What is it? Doctor provides patient with facts about disease and possible interventions, and in addition Doctor elucidates patient’s values and what s/he actually wants, and helps the patient to select the available medical interventions that realise these values. Doctor helps patient to interpret patient’s values for the patient.
3. Interpretive Model What does it assume? Patient’s values are not necessarily fixed and often even known to patient, and when patient applies them to his/her medical situation, they may even conflict. So doctor works with patient to reconstruct patient’s goals and aspirations, commitment and character Doctor does not judge patient’s values, only helps the patient to understand & use them in the medical situation.
3. Interpretive Model What is happening? Doctor is a counselor or advisor Doctor’s obligations in addition to those in informative model, include engaging in a joint process of understanding Patient autonomy = self-understanding, comes to know who s/he is and how various medical options bear on his/her identity
4. Deliberative Model What is it? Aim is to help patient to determine and choose the best health related values that can be realised in the clinical situation. Doctor explains why certain health related values are more worthy & should be aspired to Doctor-Patient deliberate about what kind of health related values patient could and should pursue.
4. Deliberative Model What does it assume? Doctor discusses only health related value – that is morality of pursuing different kind of interventions. Doctor does and should not engage with patient’s personal values Coercion is strictly avoided Patient capable of relating morality of different intervention with his/her values
4. Deliberative Model What is happening? Doctor acts as teacher or friend – explains not only what patient could, but also should do. Engages patient in a dialogue about what course of medical action is the best. Patient autonomy = self-development, empowered through dialogue on various medical alternatives available.
Patients Rights & Empowerment Demands capacity building of the patients for enhancing their ability to choose. It is essential that patients are provided full information in the form they understand informed of their rights It is equally important to change the setting of the health care so that it is non-threatening and caring. The understanding and respecting sociocultural background and the value system of patient are also pre-requisite for the promoting patient empowerment.
Patients Rights & Empowerment Patient empowerment leads to at least four health care outcomes sensitive to rights and ethics: (1) Improves patients situation within the health care system, making them partner in health care. (2) Patients are able to influence how services are run. (3) Improves quality of care (4) Increases accountability of providers.
Shift in Doctor-Patient Relationship Shift from two extremes – “paternalism” and “self-determination without doctor’s participation” to a collaborative and deliberative model of relationship Inclusion of care as a principle of providing services. Asking questions – what does my commitment to caring for this person requires me to do? And what is the best way to express that “I care”?
 What is gender mainstreaming?
What is gender mainstreaming? What is gender mainstreaming?
What is gender mainstreaming? Gender mainstreaming
Gender mainstreaming Gender mainstreaming
Gender mainstreaming Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Protection mainstreaming principles
Protection mainstreaming principles Epmc doe
Epmc doe Mainstreaming in swahili
Mainstreaming in swahili Ethics and employee rights
Ethics and employee rights Ethics and employee rights and discipline
Ethics and employee rights and discipline Positive rights vs negative rights
Positive rights vs negative rights Duties towards self
Duties towards self Legal rights vs moral rights
Legal rights vs moral rights Negative right
Negative right Media rights and ethics scavenger hunt answer key
Media rights and ethics scavenger hunt answer key Littoral rights include
Littoral rights include What is negative right
What is negative right Negative right
Negative right Rosalind hursthouse
Rosalind hursthouse Duty vs responsibility
Duty vs responsibility Micro ethics and macro ethics
Micro ethics and macro ethics Relationship between law and ethics
Relationship between law and ethics That's what i do
That's what i do Relationship between law and ethics
Relationship between law and ethics Separatist view of business ethics
Separatist view of business ethics Difference between political science and psychology
Difference between political science and psychology Descriptive ethics
Descriptive ethics Briefly recap
Briefly recap Valuing time in professional ethics
Valuing time in professional ethics Methaethics
Methaethics Descriptive ethics vs normative ethics
Descriptive ethics vs normative ethics Discipline
Discipline