Emergency Assessment and Procedures Emergency Assessment and Procedures
- Slides: 28
Emergency Assessment and Procedures
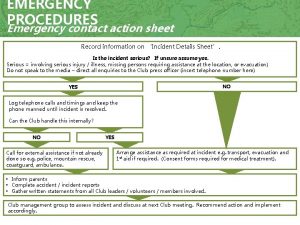
Emergency Assessment and Procedures • Athletic Trainers can begin emergency procedures only after determining the problem • They must first gather pieces of information during an assessment to determine what is going on with the athlete • Mechanism of Injury • History • Primary Assessment • Secondary Assessment • Vital signs
Permission to Treat • If working with an unfamiliar athlete, first introduce yourself and ask permission to treat the athlete • Most athletes are teenagers and can’t refuse treatment • Parents also customarily sign waivers that allow for treatment in their absence • If a parent refuses treatment, document the refusal of treatment • Have athlete sign refusal in front of a witness • Refusal of treatment is rare, but must be followed
Sign or Symptom? • When investigating an athlete’s injuries, the Athletic Trainer must ask question and observe for signs and symptoms • Sign • Objective evidence that a rescuer can measure of sense • Ex. Sweating, breath odor, temperature, blood pressure, breathing rate, heart rate • Symptom • Cannot be seen smelled or heard • Ex. Pain, nausea, and anxiety
Types of Assessments • Primary Assessment • Deals with injuries that are life threatening, or injuries involving the ABCs • Airway, Breathing, Circulation • Secondary Assessment • Involves all non-life threatening injuries
Primary Assessment • • Primary Assessments are done in the following order Check the scene Determining responsiveness CAB • Circulation • Airway • Breathing
Checking the Scene • The first step to preventing any more injuries includes making sure you do not get hurt • Approach the athlete only when the scene appears safe • Ex. If a player is hurt during a football game, ensure that play has stopped so that you don’t get hit by another player when stepping on the field
Determining Responsiveness • The first step is to determine whether an athlete is conscious and able to respond • An unconscious athlete may be able to hear the AT and respond to a voice if they do not have a severe head injury • If there is not response, check the CABs, immediately alert EMS and send for the AED • If an athlete can clearly and logically respond to a responsiveness check the AT knows that the airway, breathing and circulation is OK • At this point in the primary assessment the AT can skip the CABS and proceed to check for other injuries
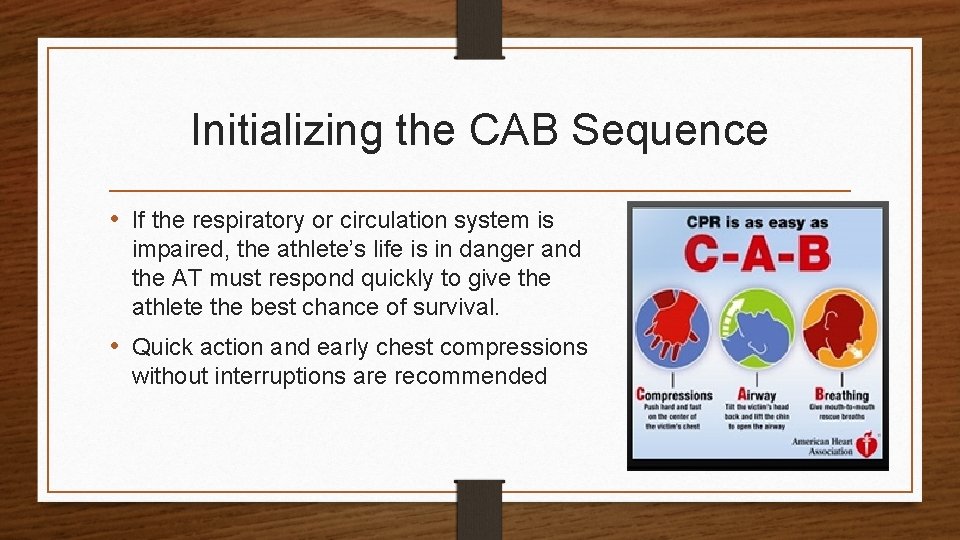
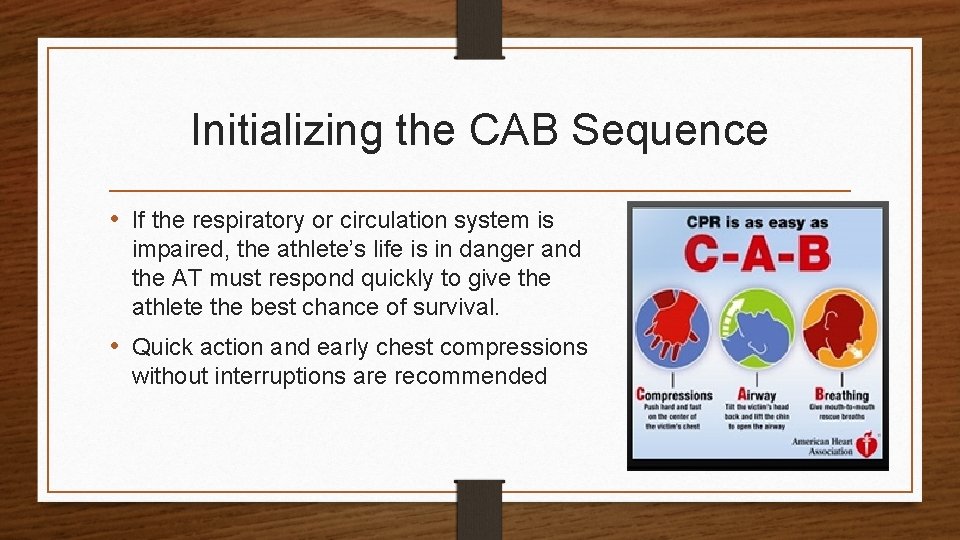
Initializing the CAB Sequence • If the respiratory or circulation system is impaired, the athlete’s life is in danger and the AT must respond quickly to give the athlete the best chance of survival. • Quick action and early chest compressions without interruptions are recommended
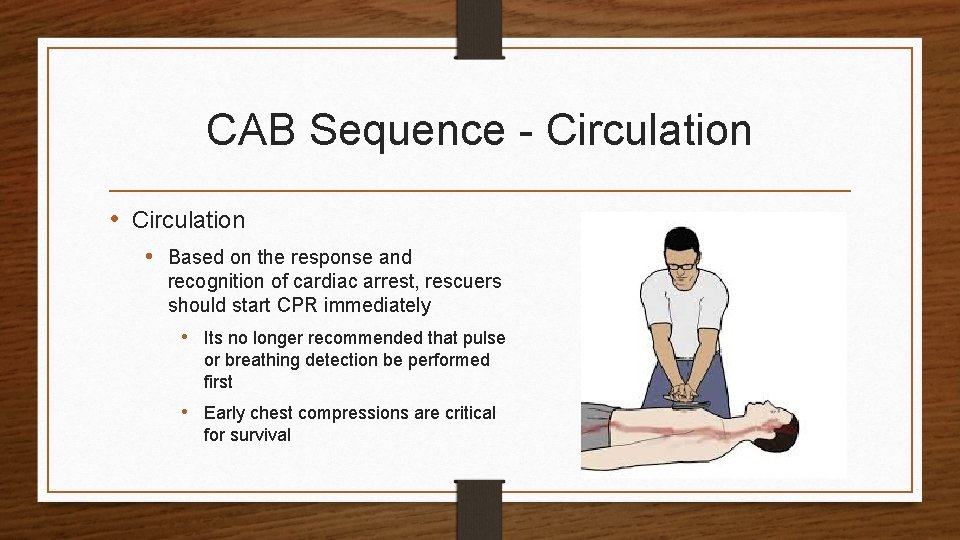
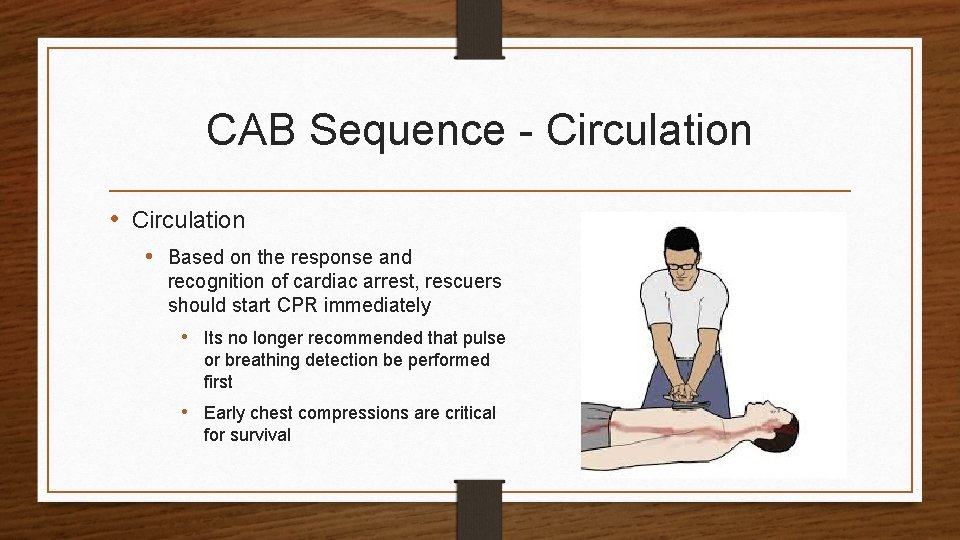
CAB Sequence - Circulation • Based on the response and recognition of cardiac arrest, rescuers should start CPR immediately • Its no longer recommended that pulse or breathing detection be performed first • Early chest compressions are critical for survival
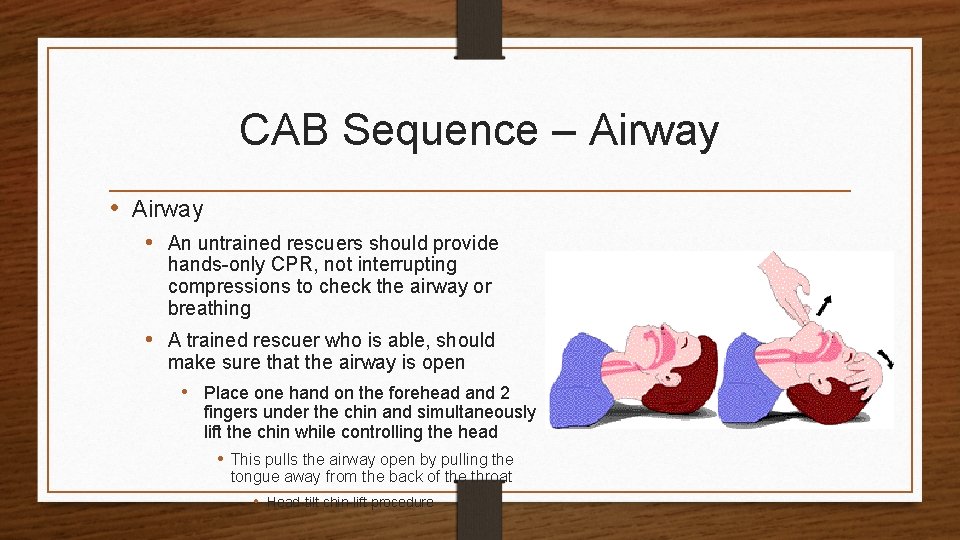
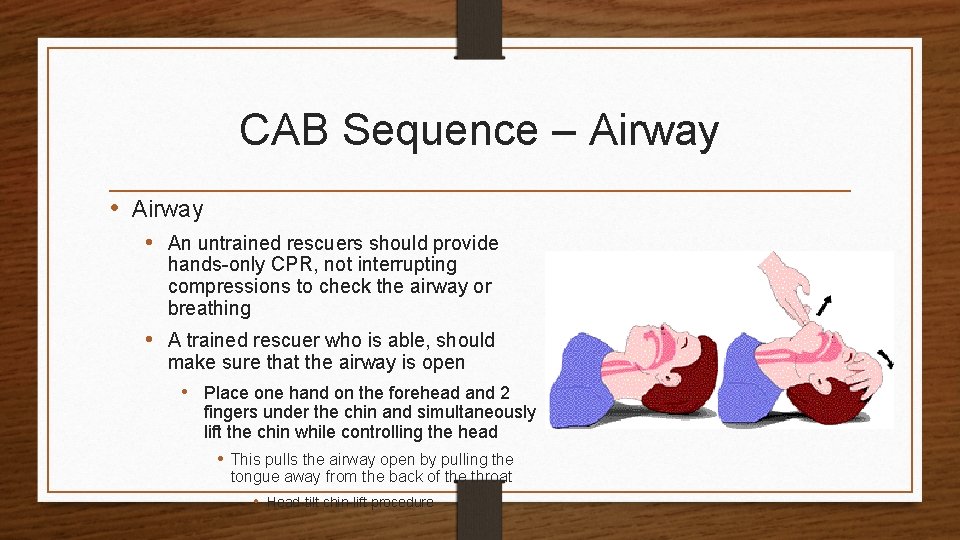
CAB Sequence – Airway • An untrained rescuers should provide hands-only CPR, not interrupting compressions to check the airway or breathing • A trained rescuer who is able, should make sure that the airway is open • Place one hand on the forehead and 2 fingers under the chin and simultaneously lift the chin while controlling the head • This pulls the airway open by pulling the tongue away from the back of the throat • Head-tilt chin-lift procedure
CAB Sequence - Breathing • To check the breathing, the AT will use a technique called look, listen and feel • Look at the chest and watch for the chest to rise and fall • Listen for breathing by placing an ear close to the mouth • Feel for hot breath on his cheek • The check for breathing should last about 10 seconds and should be done by a trained rescuer
Breathing Emergencies • Any situation in which breathing has stopped or is compromised is considered life threatening • If an AT determines that an athlete is not breathing when the primary survey is performed, rescue breaths and CPR may be initiated • An athlete’s airway can be obstructed in a number of ways, but the tongue is the number one airway obstructer
Obstructed Airway • In an unconscious athlete, especially one lying on their back, the tongue likely will relax and obstruct the air passage • Other possible obstructions • • Food Gum Mouth guards Broken teeth Vomit Blood Chewing tobacco • A conscious athlete with an obstructed airway will grab at their throat
Types of Airway Obstructions • An airway obstruction could be partial or total • Athlete will grab for the throat, the universal choking sign, usually an indication that he has a problem with the air passage • Partial airway obstruction • Occurs when an object cover the air passage but still allows some air to flow in and out of the lungs • Total airway obstruction • When an object blocks the entire air passage and does not allow enough air to flow into the lungs for the athlete to breath
Cardiopulmonary Emergencies • There are 2 cardiopulmonary emergencies that concern the AT • Heart attack • Occurs when the heart muscle is damaged by a blockage of a vessel to the heart • Cardiac Arrest • Occurs when the damage to the heart muscle is so severe that it interferes with the hearts electrical system, causing the heart to stop beating
Secondary Assessment • An evaluation of injuries that aren’t life threatening • Performed after the primary assessment has been completed and life threatening injuries taken care of • Performed in the following order • History • Head • Vital signs • Arms • Chest • Abdomen • Hips • Legs
HIT • When dealing with a specific complaint Athletic Trainers will do an assessment on a specific body part and use the HIT technique • History • Takes history to gather information about the situation and injury • Inspection • Visual examination of the body part • Testing • Includes touching, specific evaluations, checking range of motion and neurological testing
History • Taking a history includes asking questions and taking vital signs • Allows athletic trainer to obtain information about what happening as well as previous injuries and illnesses • Vital signs checked in the secondary assessment can include • • Body temperature Skin color Breathing and Heart rate Response to pain Pupillary reaction Ability to move Capillary refill
Inspection • During the inspection the AT will observe the athlete’s body and surrounding for clues as to what happened • Helps to suggest treatment options
Testing • Specific tests are done to determine the following • Severity of the injury • How the athlete should be moved • If they should be splinted • If medical help is immediately necessary
Concussions • A concussion is the temporary impairment of brain function caused by impact to the head or by a rotation force • Causes the athlete to be confused or dazed and some may lose consciousness
Symptoms of a Concussion • • • Nausea Dizziness Headache Vomiting Difficulty speaking • Ringing in the ears (tinnitus) • Loss of balance • Difficulty remembering things before or after (amnesia) • Possible battle signs • Disorientation
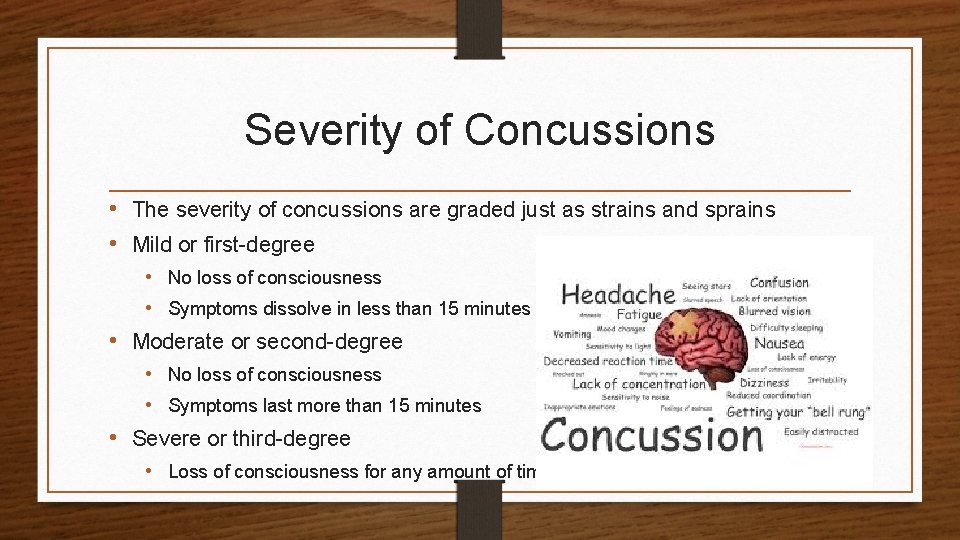
Severity of Concussions • The severity of concussions are graded just as strains and sprains • Mild or first-degree • No loss of consciousness • Symptoms dissolve in less than 15 minutes • Moderate or second-degree • No loss of consciousness • Symptoms last more than 15 minutes • Severe or third-degree • Loss of consciousness for any amount of time
Treating a Concussion • When an athlete receives a concussion they must be monitored by a physician to determine when it is safe to reenter competition • In general, an athlete can’t return to play after the first concussion until all signs and symptoms have dissolved • Decisions about return to play are made by the AT and team physician • Most athletes who receive concussions will not return to participation until they’ve completed a progression of physical activity and follow up assessments that begin after they are free of all concussion symptoms
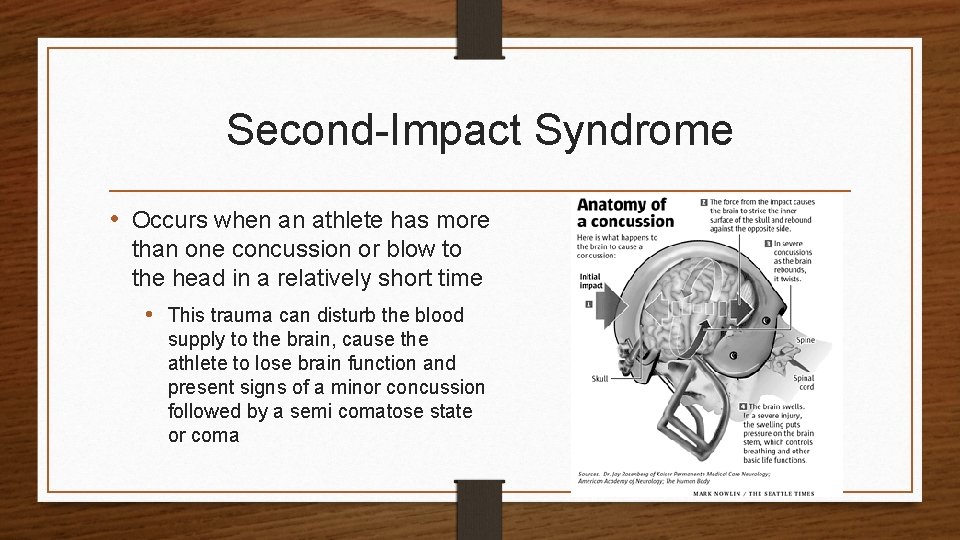
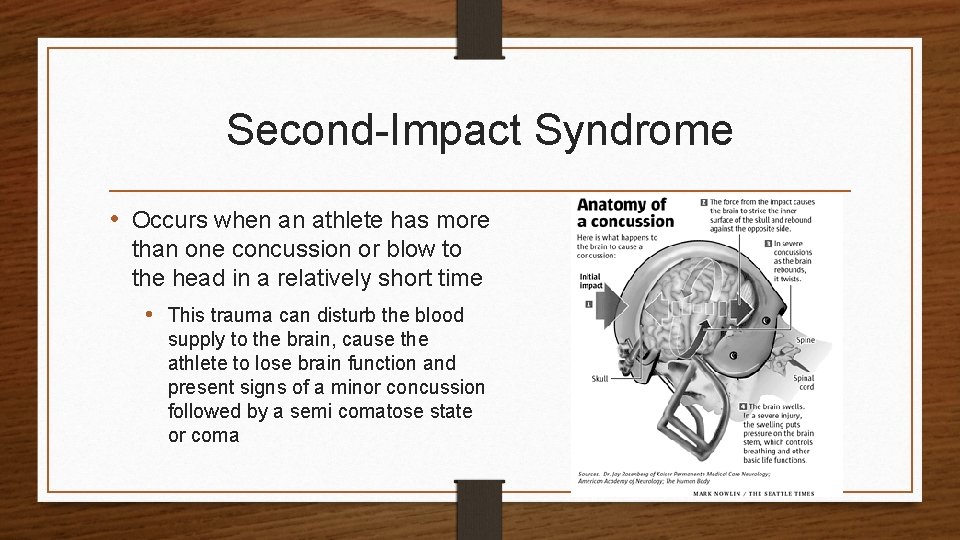
Second-Impact Syndrome • Occurs when an athlete has more than one concussion or blow to the head in a relatively short time • This trauma can disturb the blood supply to the brain, cause the athlete to lose brain function and present signs of a minor concussion followed by a semi comatose state or coma
Gfeller-Waller Concussion Awareness Act • This law was drafted and implemented to protect the safety of student-athletes in North Carolina • Signed into law by Governor Beverly Purdue on June 16, 2011 • Three main areas of focus • Education • Emergency action and post-concussion protocol implementation • Clearance/return to play or practice following concussion
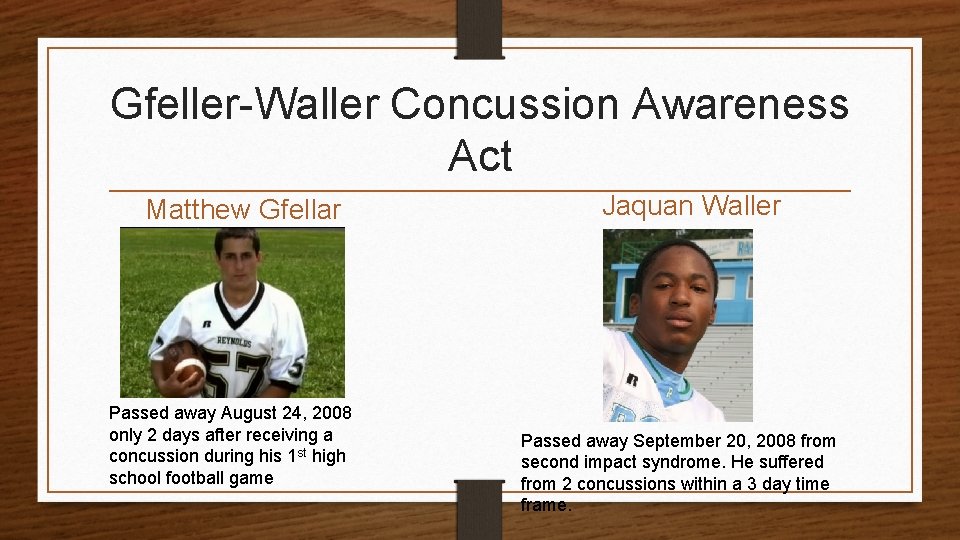
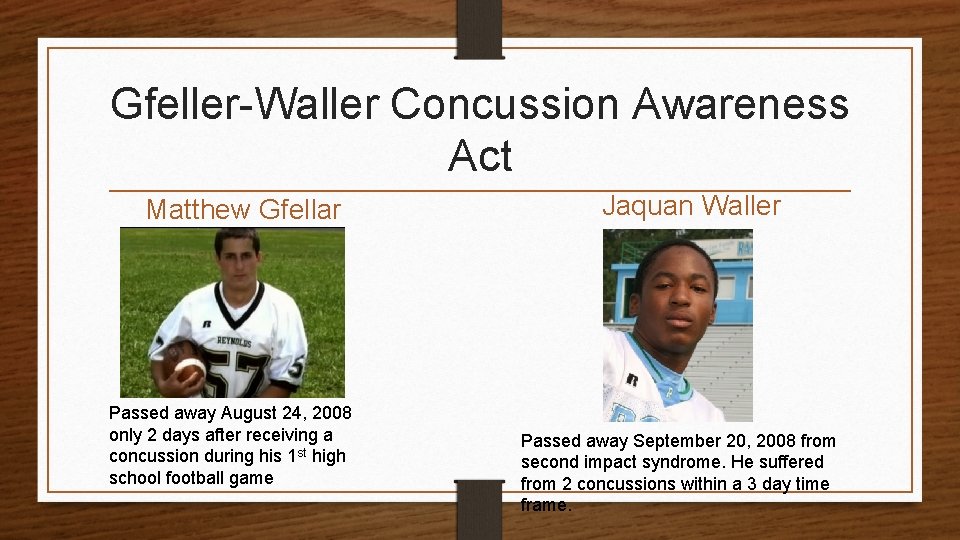
Gfeller-Waller Concussion Awareness Act Matthew Gfellar Passed away August 24, 2008 only 2 days after receiving a concussion during his 1 st high school football game Jaquan Waller Passed away September 20, 2008 from second impact syndrome. He suffered from 2 concussions within a 3 day time frame.
 Module 12 emergency procedures
Module 12 emergency procedures Emergency procedures in sport
Emergency procedures in sport Isa315
Isa315 Bsbhrm506
Bsbhrm506 Stock receiving and issuing procedures
Stock receiving and issuing procedures Sample timekeeping policy and procedures
Sample timekeeping policy and procedures Classroom policies and procedures
Classroom policies and procedures Chapter 47 laboratory materials and procedures
Chapter 47 laboratory materials and procedures Consolidation techniques and procedures
Consolidation techniques and procedures Chapter 15 diagnostic procedures and pharmacology
Chapter 15 diagnostic procedures and pharmacology Chapter 12 banking procedures and services vocabulary check
Chapter 12 banking procedures and services vocabulary check Piggybacking in go-back-n arq
Piggybacking in go-back-n arq Audit planning and analytical procedures
Audit planning and analytical procedures Capillary order of draw
Capillary order of draw Advantages and disadvantages of analytical procedures
Advantages and disadvantages of analytical procedures Bar opening and closing procedures
Bar opening and closing procedures Football field maintenance cost
Football field maintenance cost Database policy and procedures
Database policy and procedures Configuration management standards
Configuration management standards Lending policies and procedures managing credit risk
Lending policies and procedures managing credit risk Audit planning and analytical procedures
Audit planning and analytical procedures Triggers and stored procedures
Triggers and stored procedures Safe rigging
Safe rigging Collection methods and procedures
Collection methods and procedures Importance of policy and procedures
Importance of policy and procedures Biochemical data, medical tests, and procedures (bd)
Biochemical data, medical tests, and procedures (bd) Components of marketing information system
Components of marketing information system Classroom rules and procedures
Classroom rules and procedures Chapter 2 analyzing transactions
Chapter 2 analyzing transactions