Early Vasopressor use following traumatic injury Luca Carenzo

![PICO Question In patient with acute traumatic injury [Population] what is the effect of PICO Question In patient with acute traumatic injury [Population] what is the effect of](https://slidetodoc.com/presentation_image_h2/a5dca412cedd778a1ad7202fc27061ba/image-6.jpg)
- Slides: 13

(Early) Vasopressor use following traumatic injury Luca Carenzo Adult Critical Care Clinical Fellow @carenzmd RLH TREATS
Background • Principles of contemporary management of trauma patients: DCR strategy • Permissive Hypotension • […] The approach also excludes the use of vasopressors in hypovolemic trauma patients. RLH TREATS
Background • Vasopressors and inotropic agents • Recommendation 15 • In the presence of life threatening hypotension, we reccomend administration of vasopressors in addition to fluids to maintain target arterial pressure (Grade 1 C). • We recommend infusion of an inotropic agent in the presence of myocardial dysfunction (Grade 1 C). RLH TREATS
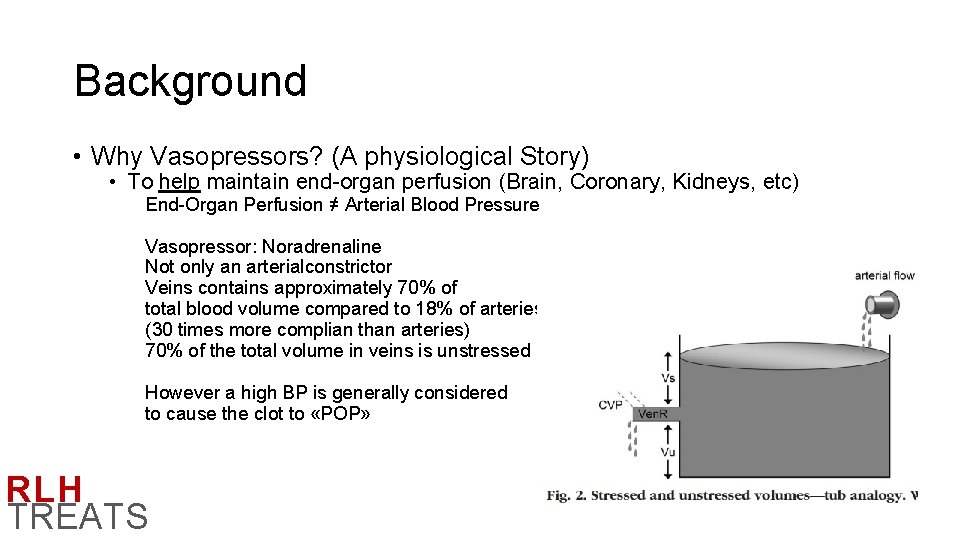
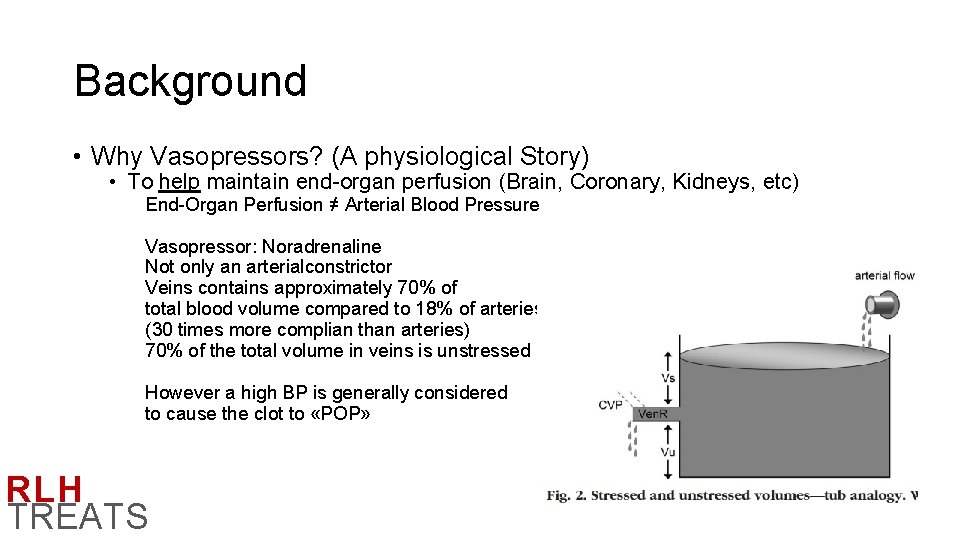
Background • Why Vasopressors? (A physiological Story) • To help maintain end-organ perfusion (Brain, Coronary, Kidneys, etc) End-Organ Perfusion ≠ Arterial Blood Pressure Vasopressor: Noradrenaline Not only an arterialconstrictor Veins contains approximately 70% of total blood volume compared to 18% of arteries (30 times more complian than arteries) 70% of the total volume in veins is unstressed However a high BP is generally considered to cause the clot to «POP» RLH TREATS
Practice at RLH • Early* Vasopressors use following traumatic injury are not routinely used at RLH. *Early: occurring during the prehospital or emergency department phase of care or during emergency trauma surgery. RLH TREATS
![PICO Question In patient with acute traumatic injury Population what is the effect of PICO Question In patient with acute traumatic injury [Population] what is the effect of](https://slidetodoc.com/presentation_image_h2/a5dca412cedd778a1ad7202fc27061ba/image-6.jpg)
PICO Question In patient with acute traumatic injury [Population] what is the effect of vasopressors administration [Intervention] versus no vasopressors [Comparator] in patient important outcomes (30 D Mortality, 90 D+ Mortality, Fluid and Blood Products Usage, Renal Replacement Therapy, Duration of Mechanical Ventilation, Neurological Outcome and Quality of Life) [Outcome] RLH TREATS
Results • Most Recent Literature Review (2017) RLH TREATS
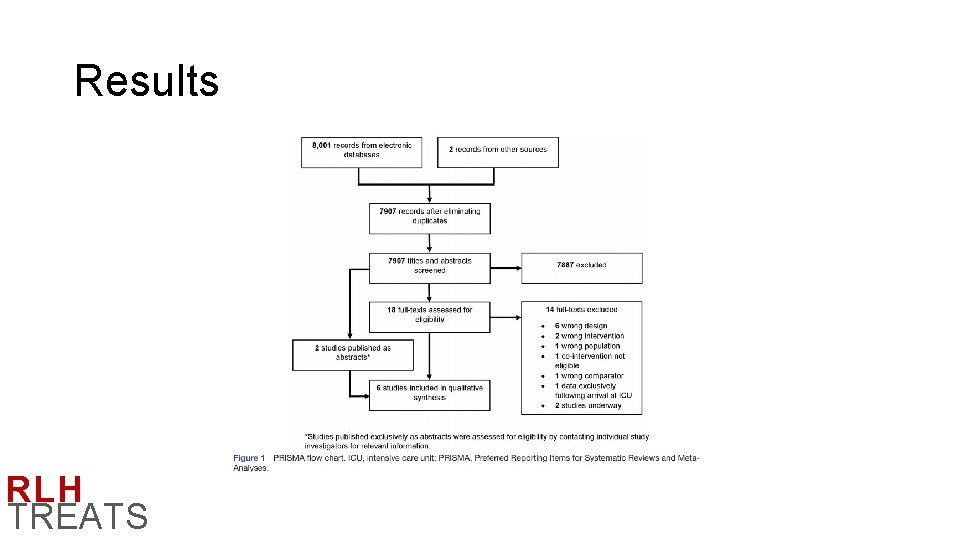
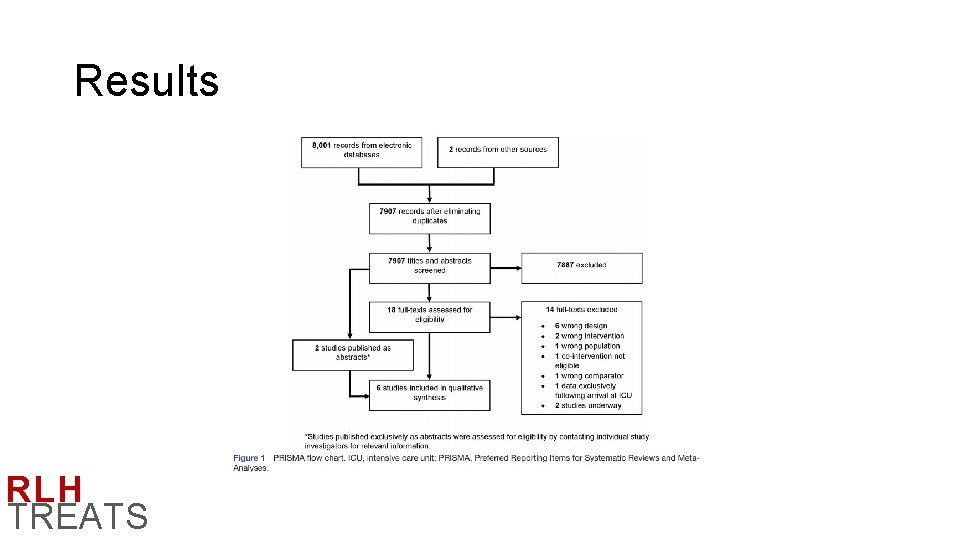
Results RLH TREATS
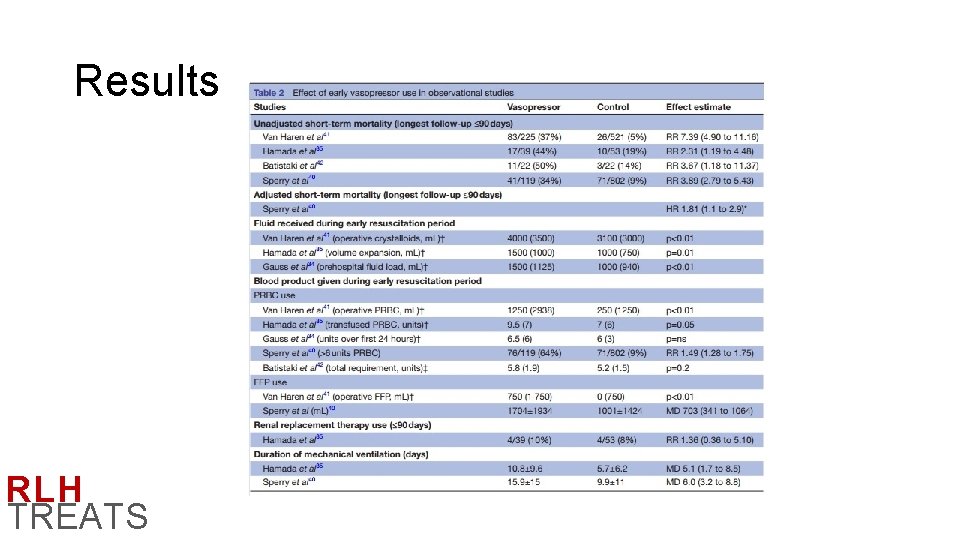
Results • 6 Studies • 1 RCT • 5 Observational studies (2 of which abstracts – prehospital use) • RCT (Cohn et al) reported that survival to 30 days was similar between patients receiving low-dose vasopressine infusion vs. placebo • Across all observational studies, early vasopressor use was associated with a statistically significant inscreased risk of early mortality (RR 2. 317. 39) • Overall very high biases RLH TREATS
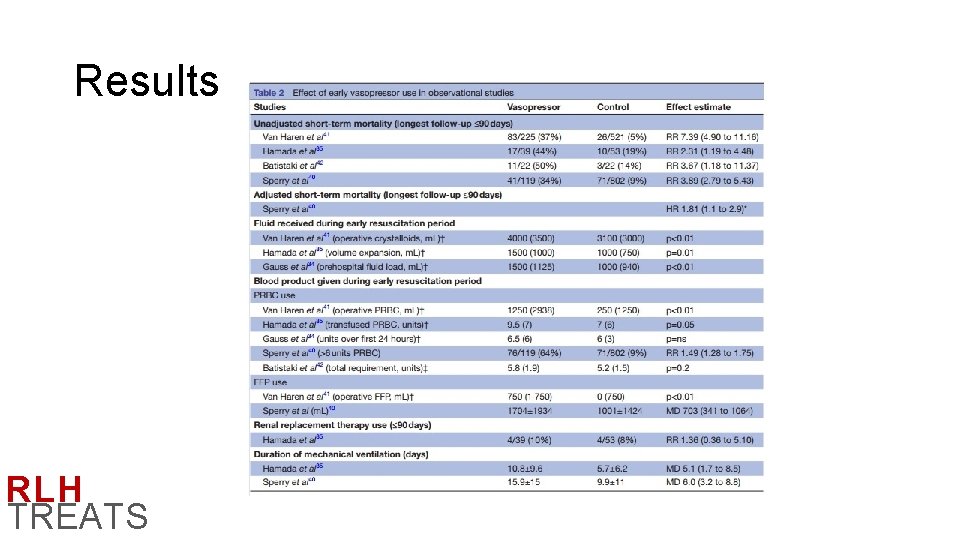
Results RLH TREATS
Results • This systematic review highlights that the balance between benefits and harms of vasopressor therapy during the early phase of resuscitation following traumatic injury is uncertain… • Current evidence does not suggest use of vasopressors in the early phase of hemorrhagic shock • A randomized controlled trial would be justified. (would need clear long term outcome measures, precise population selection, precision medicine) RLH TREATS
So what? (the twitter battle continues…) RLH TREATS
So what? What if we could target specific inotropic therapy with real time assessment of hearth function and RV failure during primary resuscitation? Would our outcome change? What about patients with very low initial blood pressure, limited response to blood products due to peripheral vasoplegia? How low are we going to accept? And what about long prehospital transfer time in remote and austere environments? RLH TREATS
 Subdural hematoma concept map
Subdural hematoma concept map Traumatic brain injury concept map
Traumatic brain injury concept map Standardised inotrope and vasopressor guidelines
Standardised inotrope and vasopressor guidelines Vasopressör
Vasopressör How to protect yourself from intentional injuries
How to protect yourself from intentional injuries C ptsd
C ptsd Diagnosis of post traumatic stress disorder
Diagnosis of post traumatic stress disorder N
N Battle's sign
Battle's sign Damselfly
Damselfly Post traumatic cervical dystonia
Post traumatic cervical dystonia Traumatic overbite
Traumatic overbite Csf traumatic tap
Csf traumatic tap Post traumatic stress disorder
Post traumatic stress disorder