Early Prediction of Chylothorax in Children After Cardiac
- Slides: 9
Early Prediction of Chylothorax in Children After Cardiac Surgery Melissa Winder, CPNP-AC; Rohin Moza, MD; Zhining Ou, MS; Angela Presson, Ph. D; Senthuran Vijayarajah, MD; Stephanie Goldstein, MD; David Bailly, MD Primary Children’s Hospital / University of Utah The Heart Center At Primary Children’s Hospital
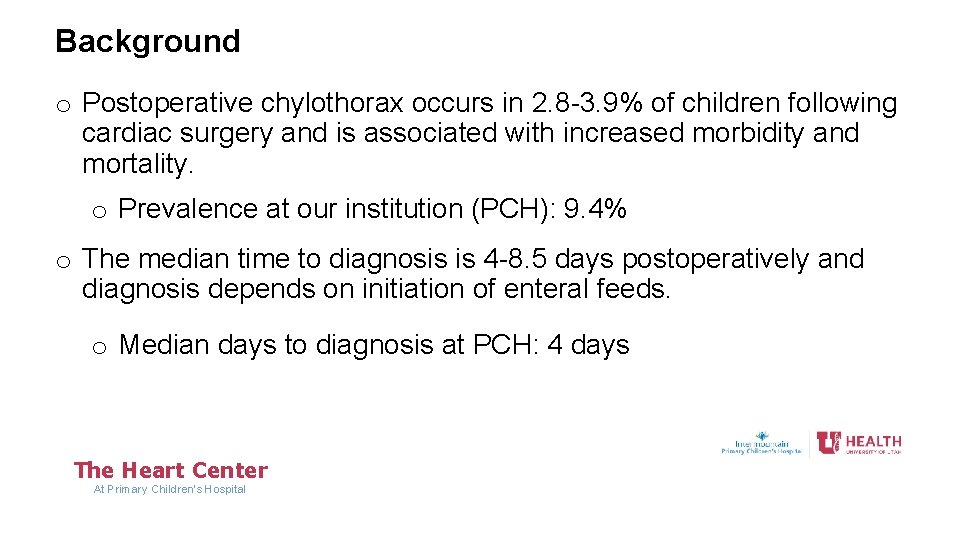
Background o Postoperative chylothorax occurs in 2. 8 -3. 9% of children following cardiac surgery and is associated with increased morbidity and mortality. o Prevalence at our institution (PCH): 9. 4% o The median time to diagnosis is 4 -8. 5 days postoperatively and diagnosis depends on initiation of enteral feeds. o Median days to diagnosis at PCH: 4 days The Heart Center At Primary Children’s Hospital
Aim o Create a predictive model to detect chylothorax earlier than traditional pleural fluid testing. The Heart Center At Primary Children’s Hospital
Methods • Design: Prospective cohort analysis of 735 postoperative patients (763 surgical encounters) at a single tertiary-care pediatric academic center between 2016 and 2020 • Inclusion criteria: Cardiac surgery • Exclusion criteria: Mechanical circulatory support and chylothorax diagnosis within post-sternal closure day 1 (the first day after primary or delayed sternal closure) • Outcome: Chylothorax diagnosis confirmed by traditional pleural fluid testing if any criteria met: • • • Triglycerides >110 mg/d. L Lymphocytes > 80% Pleural > serum triglycerides The Heart Center At Primary Children’s Hospital
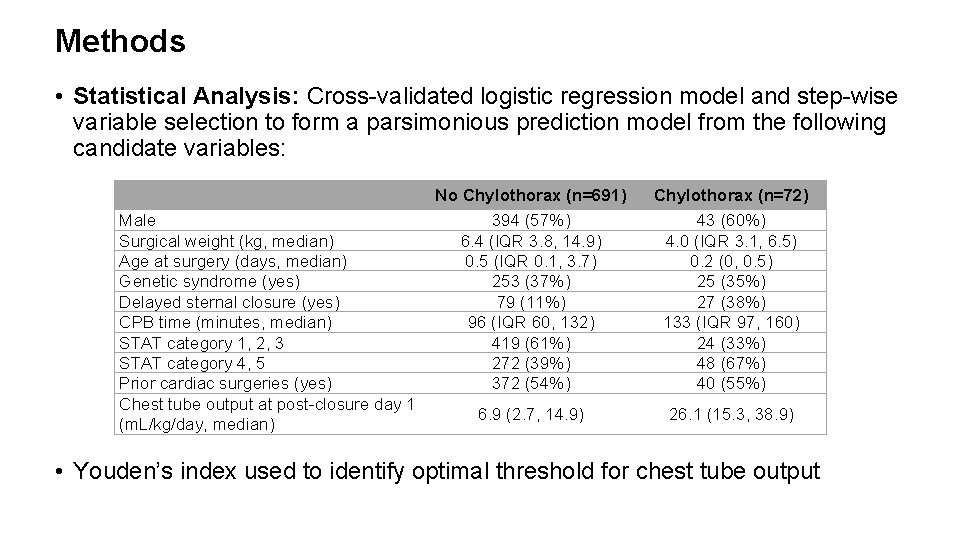
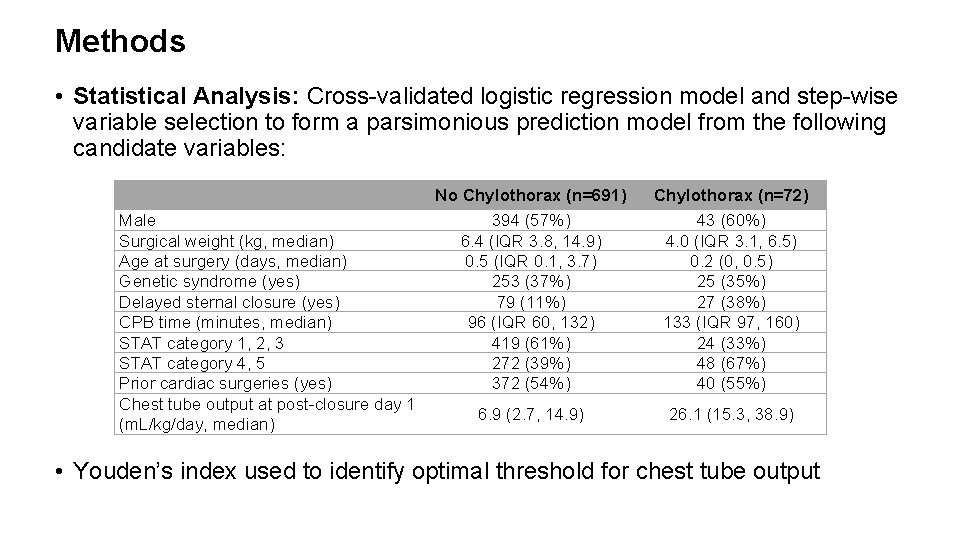
Methods • Statistical Analysis: Cross-validated logistic regression model and step-wise variable selection to form a parsimonious prediction model from the following candidate variables: Male Surgical weight (kg, median) Age at surgery (days, median) Genetic syndrome (yes) Delayed sternal closure (yes) CPB time (minutes, median) STAT category 1, 2, 3 STAT category 4, 5 Prior cardiac surgeries (yes) Chest tube output at post-closure day 1 (m. L/kg/day, median) No Chylothorax (n=691) 394 (57%) 6. 4 (IQR 3. 8, 14. 9) 0. 5 (IQR 0. 1, 3. 7) 253 (37%) 79 (11%) 96 (IQR 60, 132) 419 (61%) 272 (39%) 372 (54%) Chylothorax (n=72) 43 (60%) 4. 0 (IQR 3. 1, 6. 5) 0. 2 (0, 0. 5) 25 (35%) 27 (38%) 133 (IQR 97, 160) 24 (33%) 48 (67%) 40 (55%) 6. 9 (2. 7, 14. 9) 26. 1 (15. 3, 38. 9) • Youden’s index used to identify optimal threshold for chest tube output
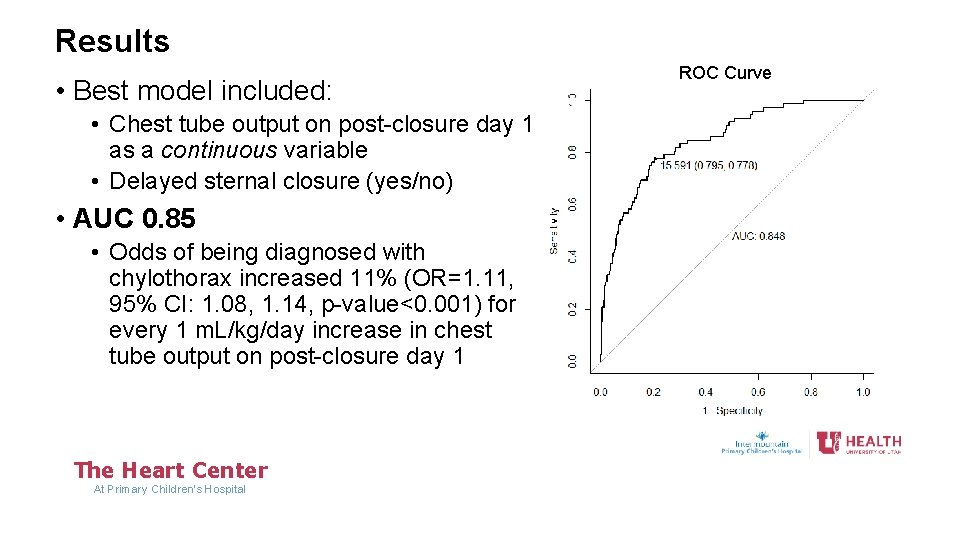
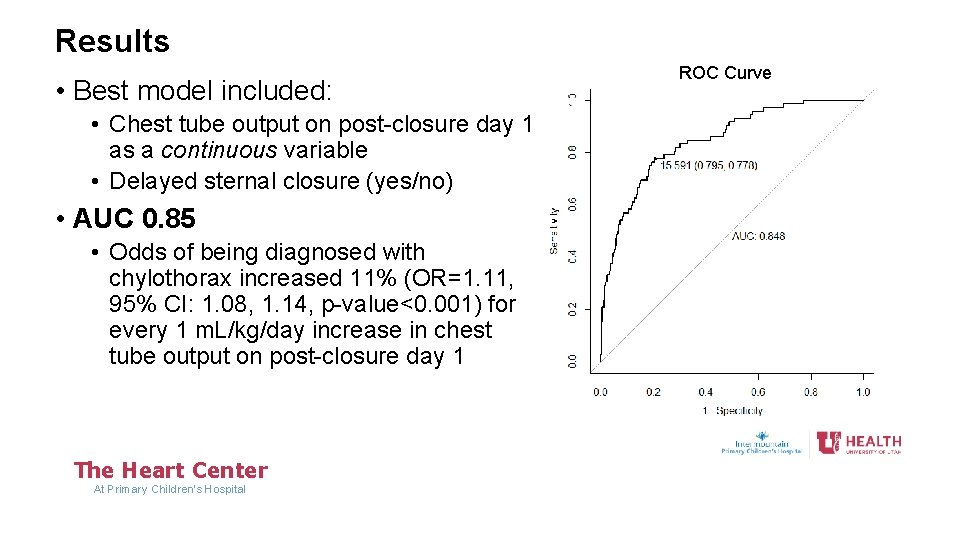
Results • Best model included: • Chest tube output on post-closure day 1 as a continuous variable • Delayed sternal closure (yes/no) • AUC 0. 85 • Odds of being diagnosed with chylothorax increased 11% (OR=1. 11, 95% CI: 1. 08, 1. 14, p-value<0. 001) for every 1 m. L/kg/day increase in chest tube output on post-closure day 1 The Heart Center At Primary Children’s Hospital ROC Curve
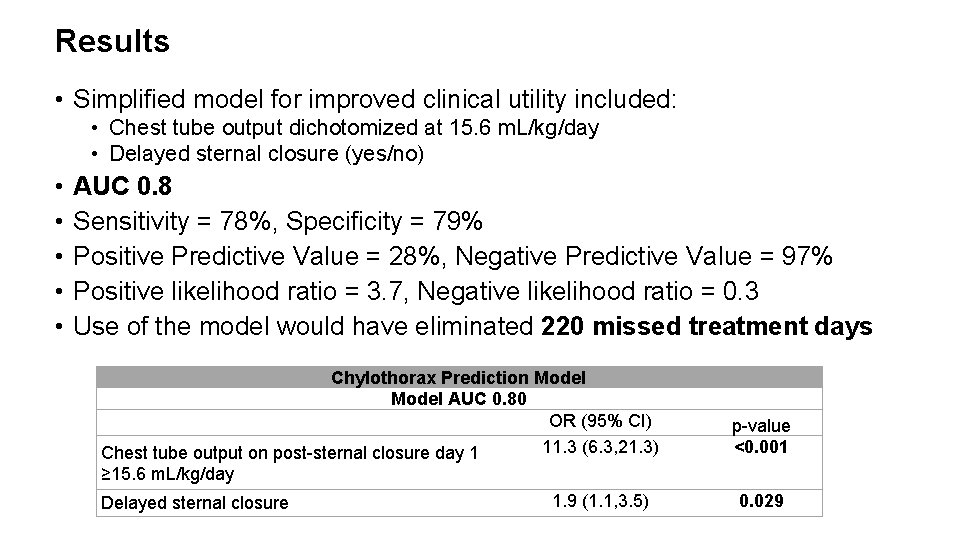
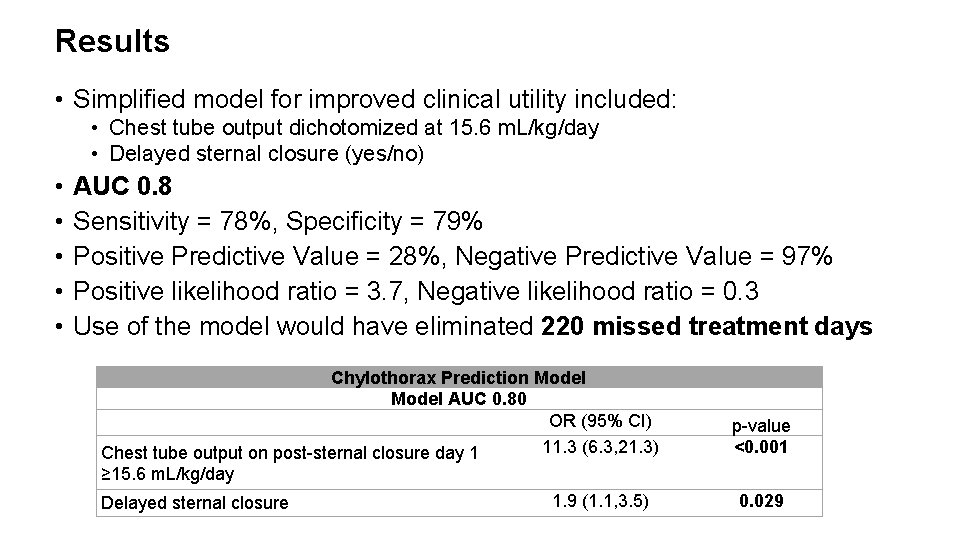
Results • Simplified model for improved clinical utility included: • Chest tube output dichotomized at 15. 6 m. L/kg/day • Delayed sternal closure (yes/no) • • • AUC 0. 8 Sensitivity = 78%, Specificity = 79% Positive Predictive Value = 28%, Negative Predictive Value = 97% Positive likelihood ratio = 3. 7, Negative likelihood ratio = 0. 3 Use of the model would have eliminated 220 missed treatment days Chylothorax Prediction Model AUC 0. 80 OR (95% CI) 11. 3 (6. 3, 21. 3) Chest tube output on post-sternal closure day 1 ≥ 15. 6 m. L/kg/day 1. 9 (1. 1, 3. 5) Delayed sternal closure p-value <0. 001 0. 029
Conclusion • High volume chest tube output (>15 ml/kg/day) on the first poststernal closure day may be an early predictor of chylothorax, allowing for diagnosis and treatment prior to the initiation of enteral feeds which may lead to earlier resolution. The Heart Center At Primary Children’s Hospital
Acknowledgements • Thanks to Jennifer Marietta, RN, and Greg Adamson, MD, for additional support for this project. The Heart Center At Primary Children’s Hospital