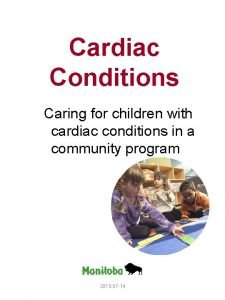
Cardiac Conditions Caring for children with cardiac conditions



- Slides: 22
Cardiac Conditions Caring for children with cardiac conditions in a community program 2015 -07 -14

How the Heart Works Ø Collects oxygen-poor blood from body and pumps it to the lungs to get oxygen Ø Pumps blood to the lungs and body by a sequence of organized contractions
Types of cardiac conditions Ø Congenital heart defects • Slows down or blocks blood flow in the heart or in the blood vessels near the heart Ø Arrhythmias • Abnormal heart beats Ø Genetic cardiac conditions Ø Acquired cardiac conditions • Occurs from infection

Treatment Ø Medication Ø Surgery • Heart transplant • Fontan procedure Ø Pacemaker Ø Internal Cardioverter Defibrillator (ICD)
Activity restrictions Ø Most children with cardiac conditions can participate in physical activities without restrictions Ø For some children, competitive or excessively stressful activities may be restricted
Infective Endocarditis Ø Inflammation caused by an infection in the lining of the heart Ø Caused by bacteria that gets into blood Ø Can lead to permanent damage of the heart Ø May require antibiotics before medical or dental procedure Inform EMS that child has cardiac condition
Congestive Heart Failure Ø Sweating during quiet time Ø Persistently rapid/labored breathing Ø Shortness of breath Ø Rapid heart rate or irregular heart rate Ø Chest pain Ø Nasal flaring Ø Blueness on or around the mouth, eyes, ears, and/or finger tips Ø Listlessness (tired and unwilling to do normal activities) Ø Inability to stop coughing Ø Skin becomes increasingly pale or blue Ø Suddenly tired

Responding to Congestive Heart Failure 1. Have child rest. 2. If condition doesn’t improve, contact parent/guardian. 3. If symptoms do not improve and parent/guardian or emergency contact cannot be reached within 5 to 10 minutes, activate 911/EMS. 4. Place child on the floor in recovery position (lying on left side). 5. Keep the airway open. Loosen any tight restrictive clothing. 6. Stay with child until EMS personnel arrive. If the child has noisy gurgled breathing, call 911/EMS.
Loss of consciousness 1. Call 911/EMS. 2. Implement CPR and the use of an automated external defibrillator (AED), if available. 3. Notify the parent/guardian. 4. Inform EMS that the child has a cardiac condition.
Child specific information Ø Type of cardiac condition Ø Activity restrictions Ø Additional information Health Care Plans are located in child file and binder
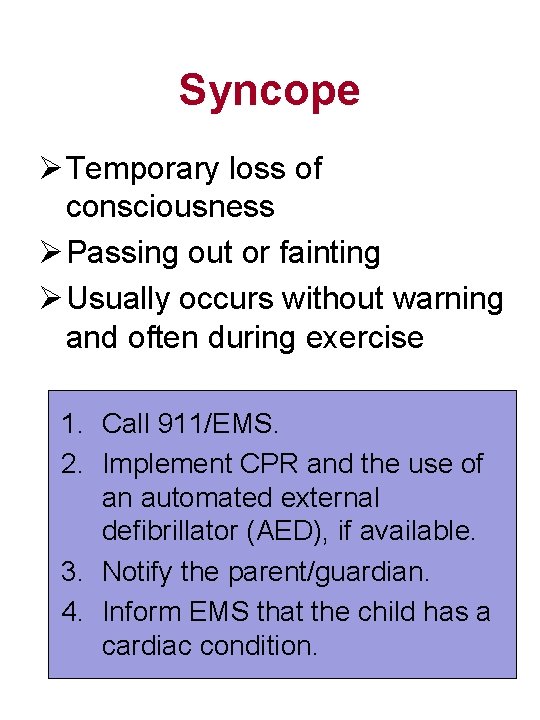
Syncope Ø Temporary loss of consciousness Ø Passing out or fainting Ø Usually occurs without warning and often during exercise 1. Call 911/EMS. 2. Implement CPR and the use of an automated external defibrillator (AED), if available. 3. Notify the parent/guardian. 4. Inform EMS that the child has a cardiac condition.
Tachycardia Ø Heart rate too fast to count Ø May experience fatigue, dizziness, lightheadedness, chest pain, shortness of breath, upset stomach, weakness
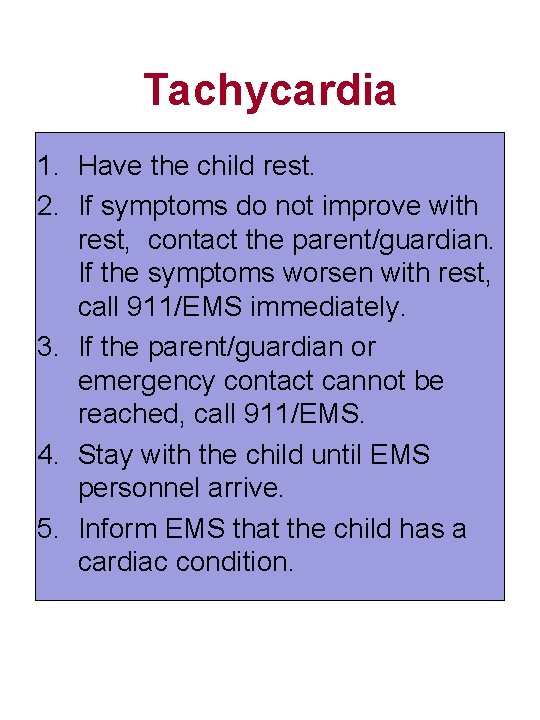
Tachycardia 1. Have the child rest. 2. If symptoms do not improve with rest, contact the parent/guardian. If the symptoms worsen with rest, call 911/EMS immediately. 3. If the parent/guardian or emergency contact cannot be reached, call 911/EMS. 4. Stay with the child until EMS personnel arrive. 5. Inform EMS that the child has a cardiac condition.
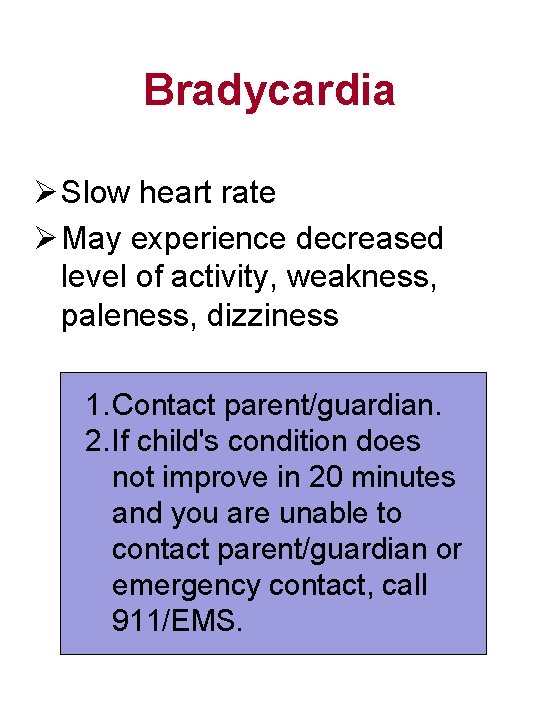
Bradycardia Ø Slow heart rate Ø May experience decreased level of activity, weakness, paleness, dizziness 1. Contact parent/guardian. 2. If child's condition does not improve in 20 minutes and you are unable to contact parent/guardian or emergency contact, call 911/EMS.
Pacemakers Ø Battery operated device used to maintain normal heart rhythm Ø May experience bradycardia and syncope Ø Some devices may interfere with the function of the defibrillator Ø Some sports may need to be avoided if they result in a blow to the chest
Internal Cardioverter Defibrillator (ICD) If child experiences an internal shock 1. Put child in recovery position (lying on left side). 2. Ensure child’s safety. 3. If child is responsive and received one shock, contact parent/guardian. 4. If parent/guardian or emergency contact cannot be reached, call 911/EMS. 5. If child is not responsive or received more than one shock, call 911/EMS.
Internal Cardioverter Defibrillator (ICD) Ø Battery operated device implanted for in chest or abdomen Ø If ICD is not working and child experiences tachycardia or syncope – call 911/EMS Ø Some sports may be restricted if they may result in a blow to the chest Ø Some devices may interfere with the function of the defibrillator
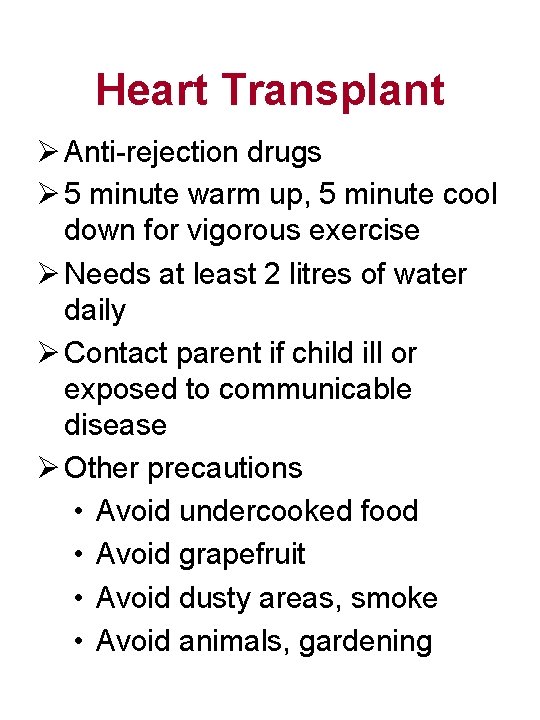
Heart Transplant Ø Anti-rejection drugs Ø 5 minute warm up, 5 minute cool down for vigorous exercise Ø Needs at least 2 litres of water daily Ø Contact parent if child ill or exposed to communicable disease Ø Other precautions • Avoid undercooked food • Avoid grapefruit • Avoid dusty areas, smoke • Avoid animals, gardening
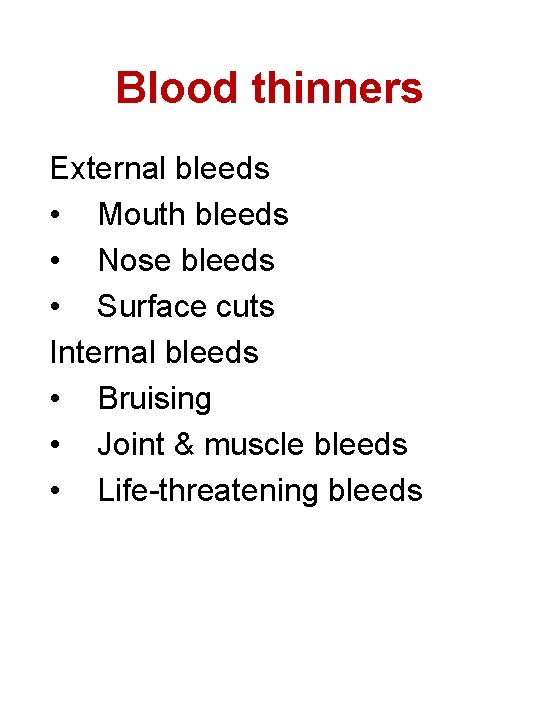
Blood thinners External bleeds • Mouth bleeds • Nose bleeds • Surface cuts Internal bleeds • Bruising • Joint & muscle bleeds • Life-threatening bleeds
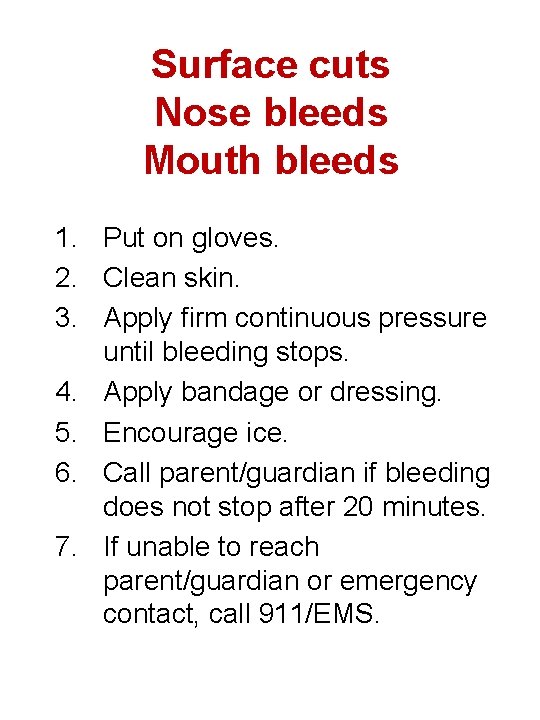
Surface cuts Nose bleeds Mouth bleeds 1. Put on gloves. 2. Clean skin. 3. Apply firm continuous pressure until bleeding stops. 4. Apply bandage or dressing. 5. Encourage ice. 6. Call parent/guardian if bleeding does not stop after 20 minutes. 7. If unable to reach parent/guardian or emergency contact, call 911/EMS.
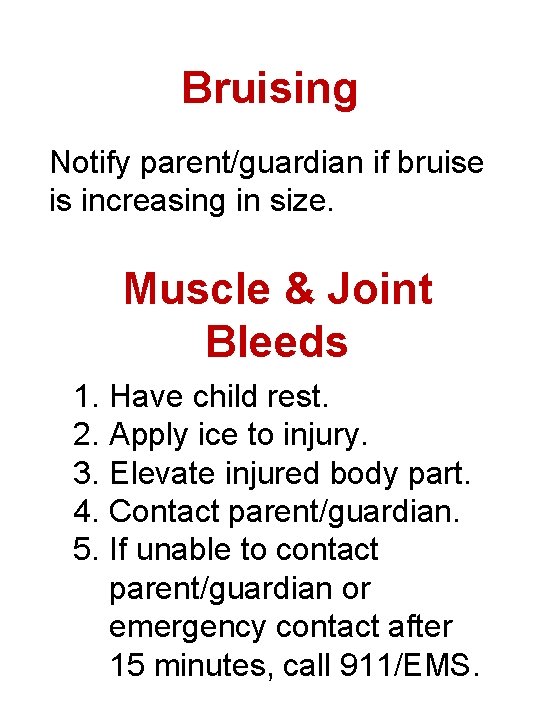
Bruising Notify parent/guardian if bruise is increasing in size. Muscle & Joint Bleeds 1. Have child rest. 2. Apply ice to injury. 3. Elevate injured body part. 4. Contact parent/guardian. 5. If unable to contact parent/guardian or emergency contact after 15 minutes, call 911/EMS.
Life-threatening Bleeds If a child has a significant injury to the head, eye, neck, chest or abdomen (with or without signs) 1. Call 911/EMS. 2. Notify parent/guardian.
 Actual caring occasion
Actual caring occasion Unit 10 caring for children and young people
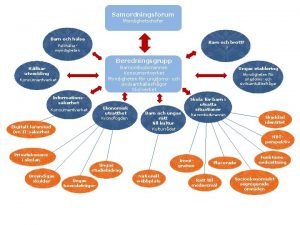
Unit 10 caring for children and young people Myndigheten för delaktighet
Myndigheten för delaktighet Presentera för publik crossboss
Presentera för publik crossboss Rådet för byggkompetens
Rådet för byggkompetens Kung som dog 1611
Kung som dog 1611 Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Adressändring ideell förening
Adressändring ideell förening Tack för att ni har lyssnat
Tack för att ni har lyssnat Mall för referat
Mall för referat Luftstrupen för medicinare
Luftstrupen för medicinare Start för skala
Start för skala Formel för lufttryck
Formel för lufttryck Vilket tal pekar pilen på
Vilket tal pekar pilen på Elektronik för barn
Elektronik för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Borra hål för knoppar
Borra hål för knoppar Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Bris för vuxna
Bris för vuxna Mat för unga idrottare
Mat för unga idrottare Trög för kemist
Trög för kemist Vad är ett minoritetsspråk
Vad är ett minoritetsspråk