Department of Anesthesiology M M Conference MMPI Presenter

- Slides: 18
Department of Anesthesiology M & M Conference MMPI Presenter Name Presentation Date
M&M conference objectives • The goal of M&M is to discuss cases of adverse outcomes which might provide lessons in terms of cognitive errors made or identifying system issues that need to be addressed. • Ultimately, the aim is to prevent future adverse outcomes and improve quality of care. • The Department of Anesthesiology endorses a “non-blame” culture where errors can be openly acknowledged. It is recognized that medicine is challenging and that errors and adverse events are inevitable. The goal is to improve care by sharing and examining our collective experiences.
What is an MMPI Discussion Partner / Presenter? • A member of the Department of Anesthesiology’s Morbidity, Mortality, and Performance Improvement (MMPI) committee will be identified as a “discussion partner / presenter” for all cases. • MMPI members assist with case review and selection. They have interest and additional training in patient safety, quality improvement, and event analysis. • You are accountable for preparing the presentation. Discussion partner / presenters will assist with: – Streamlining presentations – Identifying discussion and take-home points – Discussing links between individual cases and new or ongoing performance improvement activities.
Recommended Presentation Format • • Event Identification Relevant PMH/Background Info Description of Event Differential Diagnostic Patient Outcome Discussion (include specific topics requested by MMPI) Take-home message The following slides will help you prepare your presentation.

Event Identification • The second slide should be a one-sentence description of why the case is being presented. This will help the audience focus on the details of the case. – Example: “I am presenting a case of a patient that was unintentionally extubated during surgery” – Example: “This is a case of a patient that developed a pneumothorax following a central line insertion. ”
Relevant Past Medical History • Only relevant information need be presented. Example: include allergies only if it matters to the case. • There is no need for detailed H & P. Example: it is enough to say the patient presented for CABG surgery because of CAD. • Same for medications, past surgical history, etc – keep information brief and omit if irrelevant.
Physical Exam/Labs/Testing • Include relevant vital signs and physical findings Example: If the presentation doesn’t have anything to do with the airway, omit the airway exam/MP class. • Include relevant labs and/or imaging Example: Elevated creatinine for a patient in ESRD does not need to be discussed, but hyperkalemia might if it relates to a cardiac event.
Description of the Event • Keep it brief and relevant. Example: if it relates to a postop event and the induction and intraop management was straightforward, its enough to say so. • Only relevant and needed information should be presented. Example: omit list of induction drugs if it isn’t relevant. • Use your judgment about what is needed. Your MMPI discussion partner can help with narrowing down to essential information for presentation efficiency • Include an exact description of the event being discussed
Differential Diagnostic • Brief list of differential diagnostics (if applicable) • Your diagnosis of what caused the morbidity/mortality
Patient Outcome • Tell us, briefly, how the patient did. Example: Did they leave the hospital alive? How long in the hospital/ICU? etc.
Discussion: Standard Topics What happened? Was the patient harmed? § If the event reached the patient, options include: § No harm resulted § Need for increased monitoring or treatment § Temporary/permanent harm § Patient died as a result of the event § Or, was this a near miss/close call where the event did not reach the patient? What went wrong? (See next two slides for discussion ideas)
Discussion: Possible Topics* (1/2) Were there any patient factors that increased this patient’s risk for harm? § Examples: medical conditions, language barriers, social situations Did teamwork failure contribute to the outcome? § Examples: breakdown in communication between team members, across shifts, between teams, and across specialty boundaries or due to inappropriate assignment of personnel Were there any local environmental contributors? § Examples: staffing, stocking, equipment, sufficient policies/guidelines Were there any hospital-wide contributors? § Examples: production pressure, access to consultants, beds, treatments *Note that you should NOT list/address all of these questions in each presentation! Include only relevant items that contributed to adverse outcome or helped mitigate more severe harm.
Discussion: Possible Topics* (2/2) Were there any cognitive issues (errors) or biases? § These terms refer to specific pitfalls in clinical decision making – examples include anchoring bias, confirmation bias, loss aversion. Click the links to learn more, or ask your MMPI discussion partner. Were there any issues with communication? Were there any contributing skill-set errors? § Examples: procedural complications or errors in interpretation of ECGs, laboratory or diagnostic imaging tests Were there any task-based errors? § Examples: failure of routine behaviors such as preop assessment, attention to vital signs and appropriate monitoring *Note that you should NOT list/address all of these questions in each presentation! Include only relevant items that contributed to adverse outcome or helped mitigate more severe harm.
What is the “Take Home” Message? § Tell us what you learned from this case § For example… § Was there a way the outcome could have been avoided, or harm reduced? § How might others avoid a similar outcome in the future?
Presentation Tips (1) • The goal is to present the case in less than 5 minutes in order to have more time for discussion. That means less time for information that doesn’t contribute to understanding what happened. • The attending for the case being presented and the MMPI discussion partner / presenter should have seen and approved the presentation. • The anesthesia team involved in the case should contact the MMPI discussion partner with any question. The presentation should be sent to the MMPI presenter at least 1 week prior to the date of the presentation.
Presentation Tips (2) • Pictures or images of x-rays, ECGs are great additions to your presentation (omit/crop patient identifiers). • Consider using a screenshot of the anesthetic record to illustrate vital sign patterns (crop patient identifiers and enlarge/zoom to area of interest). • You are not asked to present a literature review or an elaborate presentation on the topic. The goal is to focus on the case and learning from any adverse outcome.
Presentation Tips (3) • At least 28 point font should be used. • Please use this slide template/format for your presentation. • It is OK to use phrases instead of sentences.
Please contact Dr. Megan Anders (manders@anes. umm. edu) or the SCORE program (quality@anes. umm. edu) if you have any questions about preparing your presentation.
 Tufts medical center anesthesiology residency
Tufts medical center anesthesiology residency Umass memorial nurse residency program
Umass memorial nurse residency program Hans and sybil eysenck personality dimensions
Hans and sybil eysenck personality dimensions Mmpi scales
Mmpi scales Mmpi training
Mmpi training Mmpi skale
Mmpi skale Mmpi minnesota multiphasic personality inventory
Mmpi minnesota multiphasic personality inventory Clinical scales of mmpi
Clinical scales of mmpi Validity scales of mmpi-2
Validity scales of mmpi-2 Personality mod
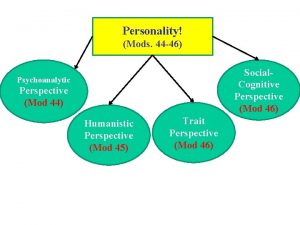
Personality mod Mmpi test romana
Mmpi test romana Interpreting the mmpi-2-rf
Interpreting the mmpi-2-rf Mmpi vs myers briggs
Mmpi vs myers briggs Mmpi scoring
Mmpi scoring Tes mmpi tidak valid
Tes mmpi tidak valid General conference stewardship department
General conference stewardship department Presentation name
Presentation name Mitel presenter
Mitel presenter Presenter (se bifogad flik)
Presenter (se bifogad flik)