Concrete Actions Johns Hopkins Neurology Neurohospitalist Advanced Clinical

- Slides: 14
Concrete Actions: Johns Hopkins Neurology Neurohospitalist Advanced Clinical Practice Instructorship John C. Probasco, MD Assistant Professor of Neurology, Johns Hopkins School of Medicine AUPN Leader’s Forum New Orleans, LA October 12, 2013 1
Neurohospitalists: • Care of inpatients with or at risk for neurological disease. 1 • Practice in academic and non-academic settings. 2 • High acuity patients with a wide spectrum of neurological disease. 2, 3 • Natural interests: Care quality, patient safety, neurological disease pathophysiology, treatment and education. 2 • The necessity of specific training and core features of training not defined. 2, 3 1. AAN (2012). 2. Likosky, et al. (2010) Frontiers in Neurology. 3. Josephson, et al. (2008) Annals of Neurology. 2/12/2022 2
Johns Hopkins Neurohospitalist Experience In 2011, Johns Hopkins Neurology began process of developing a neurohospitalist training program. Raised questions: • Demand for specialized training? • What should training entail? • Fellowship vs. Instructorship? 2/12/2022 3
Neurohospitalists: Perceived Need in Academic Neurology • In 2012, survey of leadership of ACGME accredited neurology departments. • 38% of respondents employ neurohospitalists. • 65% felt there should be an ACGME accredited neurohospitalist fellowship. • 4 departments had a neurohospitalist training program. • 10 departments planned to create a training program within two years. Probasco, et al (2013). The Neurohospitalist. 2/12/2022 4
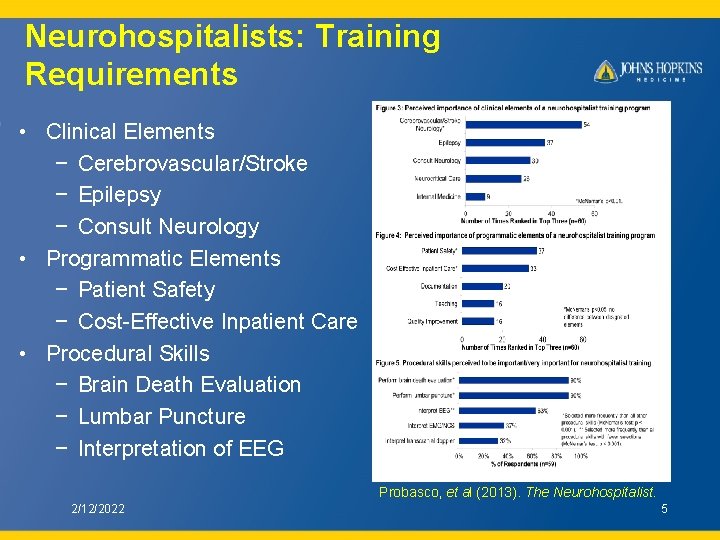
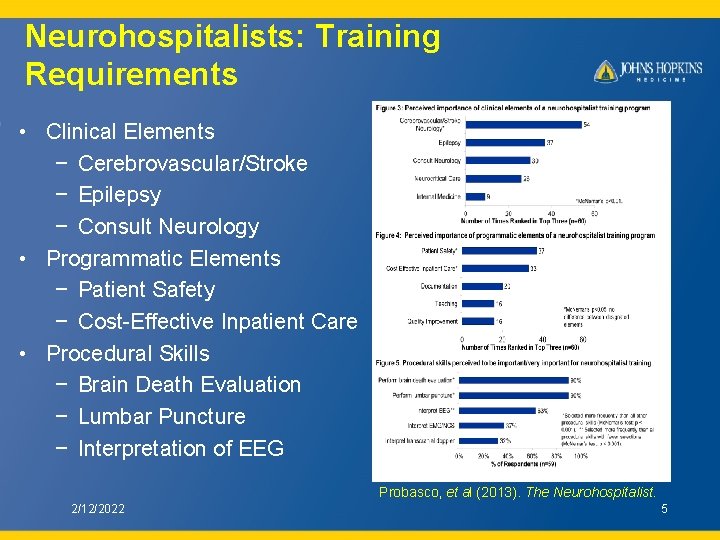
Neurohospitalists: Training Requirements • Clinical Elements − Cerebrovascular/Stroke − Epilepsy − Consult Neurology • Programmatic Elements − Patient Safety − Cost-Effective Inpatient Care • Procedural Skills − Brain Death Evaluation − Lumbar Puncture − Interpretation of EEG Probasco, et al (2013). The Neurohospitalist. 2/12/2022 5
Johns Hopkins Neurohospitalist Advanced Clinical Practice Instructorship In July 2012, Johns Hopkins Neurology introduced an advanced clinical practice instructorship in general inpatient neurology. Goal: Provide neurologists the experience and skill set to excel in this developing area of clinical neurology and academia. • Clinical Care • Education • Research 2/12/2022 6
Clinical Care 1. Attend on inpatient academic services: • Work alongside students, residents, fellows and PAs • Johns Hopkins Hospital Inpatient General Neurology Service − Broad neurology exposure − Develop clinical instruction and procedural skill set • Johns Hopkins Hospital Neurology Consultation Service • Johns Hopkins Bayview Medical Center Inpatient Neurology Service − Broad exposure, including cerebrovascular/stroke − Experience managing intermediate care patients 2/12/2022 7
Clinical Care 2. Urgent care and post-hospitalization clinic • Develop and maintain outpatient skills • Broad clinical exposure • Understand issues of patient care transitions between the outpatient and inpatient settings − Urgent new patient evaluation − Expedited outpatient evaluation − Coordinate admission and evaluation − Facilitate post-hospitalization care transition 2/12/2022 8
Education • Develop expertise in the education of residents and fellows while attending • Provided further clinical training through: − Departmental conferences − One-on-one instruction with senior faculty • Emphasis on quality improvement − Participation in departmental and care unit initiatives 2/12/2022 9

Research • Opportunity to pursue complementary training in a variety of areas: − Patient safety and quality improvement − Clinical research − Global neurology • Provide protected time for development of research interests • Senior faculty provide research guidance and mentorship 2/12/2022 10
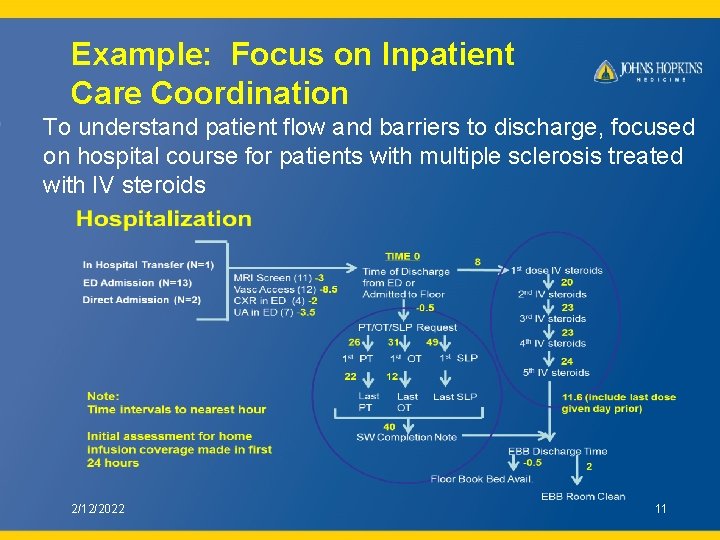
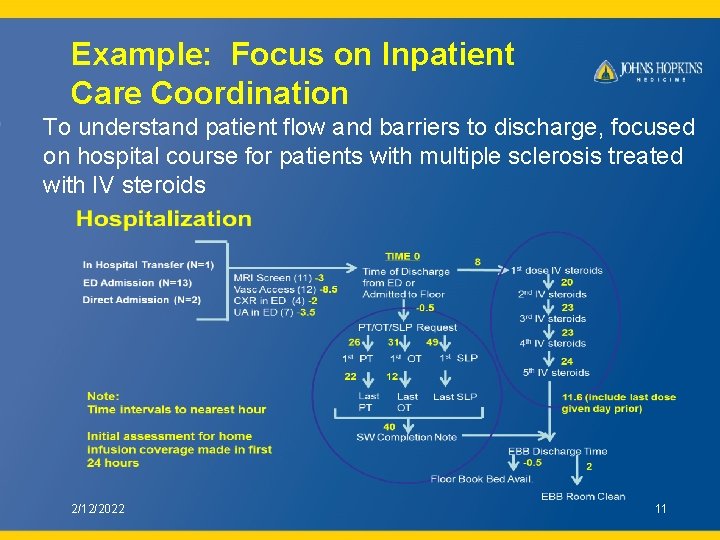
Example: Focus on Inpatient Care Coordination To understand patient flow and barriers to discharge, focused on hospital course for patients with multiple sclerosis treated with IV steroids 2/12/2022 11
Example: Focus on Inpatient Care Coordination • Interventions: 1. Interdisciplinary provider checklist 2. Provider order set 3. Patient checklist and education materials • Preliminary analysis: − Improved care coordination Reduced time from request to first therapy assessment from 26 to 13 hours − Improved discharge process efficiency Reduced time from treatment completion to discharge from 8. 5 to 4. 5 hours 2/12/2022 12
Funding Source Instructor position funded through hospital resources • Inpatient clinical activity • Outpatient clinical activity • Training in billing through departmental administrative offices 2/12/2022 13
Acknowledgments Dr. Arun Venkatesan Dr. Michael Levy Dr. Rafael Llinas Dr. Justin Mc. Arthur Contact: John Probasco, MD Johns Hopkins Department of Neurology jprobas 1@jhmi. edu 2/12/2022 14
 Sneedville
Sneedville Johns hopkins individual evidence summary tool
Johns hopkins individual evidence summary tool Johns hopkins
Johns hopkins Dr petri lupus center
Dr petri lupus center Johns hopkins medicine strategic plan
Johns hopkins medicine strategic plan Innovation 2023
Innovation 2023 Homewood student affairs
Homewood student affairs John hopkins community physicians
John hopkins community physicians Jhu apl internship
Jhu apl internship Johns hopkins essays
Johns hopkins essays Redcap hopkins
Redcap hopkins Wilmer eye clinic bel air maryland
Wilmer eye clinic bel air maryland Adobe captivate advanced actions
Adobe captivate advanced actions Informal inventory
Informal inventory Concrete semi concrete abstract
Concrete semi concrete abstract