Chapter 8 Private Payers Employersponsored Group health plans


- Slides: 23
Chapter 8 Private Payers

Employer-sponsored Group health plans Carve out~designed plan Open enrollment periods Regulated by state laws
Features of Group Plans Specific rules for eligibility Waiting period Late enrollees Premiums, deductibles, limits
COBRA Consolidated Omnibus Budget Reconciliation Act Continued coverage with employer HIPAA rules Preexisting conditions Credible coverage
Federally Guaranteed Provisions Newborns’ and Mothers’ Health Protection Act Women’s Health and Cancer Rights Act Mental Health Parity Act Genetic Information Nondiscrimination Act
Thinking It Through 8. 2 If a GHP has a 90 -day waiting period, on what day does health coverage become effective? In terms of enrollment in a health plan, what is the status of an infant born to a subscriber in the plan? A patient pays for a cosmetic procedure that is not medically necessary under the terms of the plan, Does this payment count toward the deductible?
Self-funded Health Plans Self-insured Funds set aside for payments Regulated by federal laws Third-party claims administrators Process and pay claims, collect premiums
Individual Health Plans Students Self-employed Early retirees Part-time employees not on group plan
Private Payers PPO—most popular Discount fee for service More choices than an HMO—second most popular Least amount of choices, lowest cost PCP Use a business model (financially responsible) Staff model-physician’s are employees Group model-owned facilities (capitation) POS Choose from a primary or secondary network
Payment Methods PPO—premium, deductible, coinsurance HMO—premium and copay POS—premium and copay Indemnity—premium, deductible, coinsurance
Capitation Contracts Patient eligibility Referral requirements Reports and write offs Billing procedures
Consumer-driven Health Plans High deductible Tax deferred saving accounts Consumer makes more decisions about health payments Have web tools to help with decisions What do you think the dangers are of having a CDHP?
Funding Accounts Reimbursement Employer funded High deductibles Medical Savings Funds set aside by employee to be spent on health care costs Also high deductible Flexible Savings Augment a health insurance plan Pretax dollars put into an account
Consumer-driven Payments 1. 2. Bill the patient Patient submits to reimbursement account OR withdraws from savings account OR pays bill and submits for funds from flexible account 3. Once funds are exhausted Coinsurance is paid by reimbursement account Patient pays out of pocket from savings accounts
Participating Providers’ Contracts Determine obligations with the contract Definitions of medical necessity Allowable fees Acceptance of members Referrals and preauthorizations Payment guidelines Why would a provider want to participate?
Physician Responsibilities Services offered Acceptance of members (all or a percentage) Referral rules—network only? Preauthorization necessity Utilization review (access to records)
Managed Care Plan Responsibilities Specific identification of enrolled patients Quick payment turn around Stop-loss provision (capitation)
Billing Guidelines Fees Billing requirements Filing deadlines Patient responsibilities Balance billing rules Coordination of benefits rules Timelines for incorrect payments
Billing Guidelines Bill from provider’s fee schedule—not allowed amounts Write off happens after all payers have paid before billing patient Payment for no shows When and how many copays are made
Preauthorization/Precertification Elective surgery Scheduled surgeries Emergency surgeries (48 hours) Use of a utilization review organization Out of network services Forms sent before admitting for surgery
Plan Summary Grid Quick reference showing Type of plan What is covered Patient responsibilities What needs authorization Whether patient can go out of network Process for hospitalization
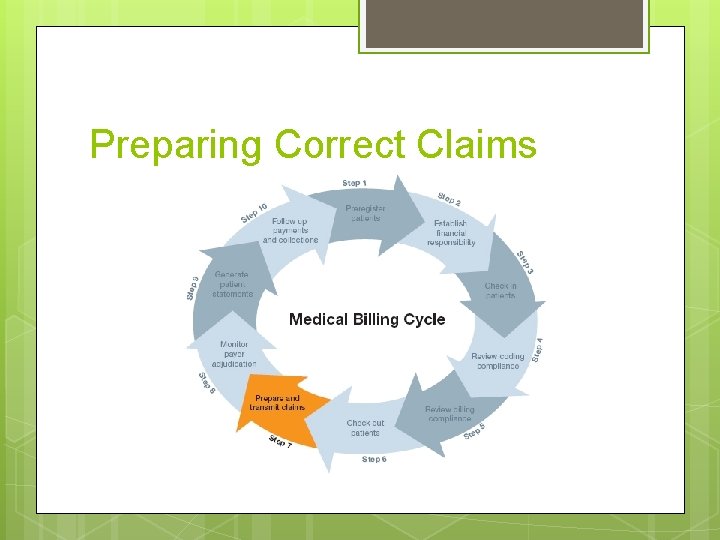
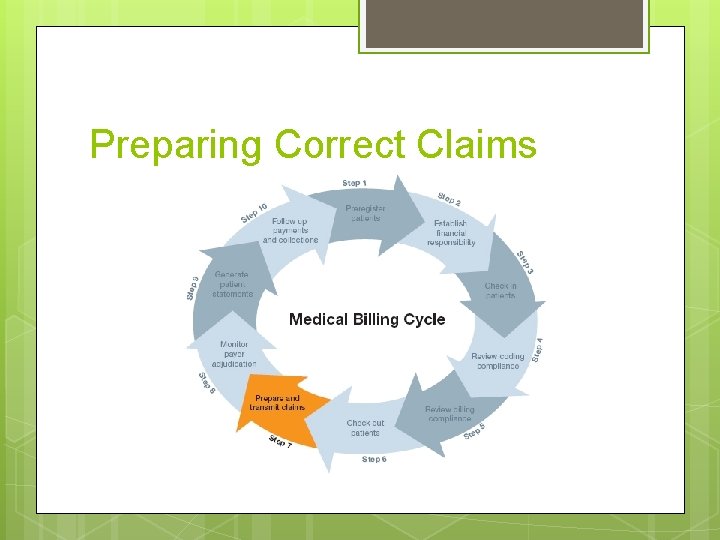
Preparing Correct Claims

 Food group plans
Food group plans Food group plans
Food group plans Nfp private client group
Nfp private client group Rocky mountain health plans dualcare plus
Rocky mountain health plans dualcare plus Mental health policy, plans and programmes michelle funk
Mental health policy, plans and programmes michelle funk 2159674690
2159674690 Apple health managed care plans
Apple health managed care plans Neft form raksha tpa
Neft form raksha tpa Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Glencoe health chapter 1 understanding health and wellness
Glencoe health chapter 1 understanding health and wellness Understanding health and wellness chapter 1
Understanding health and wellness chapter 1 Chapter 2 developing marketing strategies and plans
Chapter 2 developing marketing strategies and plans Chapter 24 section 1 animal characteristics answer key
Chapter 24 section 1 animal characteristics answer key Ilumination
Ilumination Group polarization in mean girls
Group polarization in mean girls Y = a(b)^x
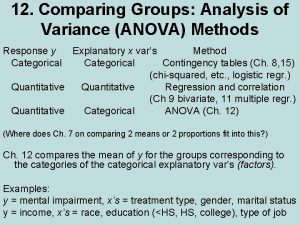
Y = a(b)^x Anova within group and between group
Anova within group and between group Unsocial group example
Unsocial group example Group 1 vs group 2 specialties
Group 1 vs group 2 specialties Thermal decomposition of group 1 nitrates
Thermal decomposition of group 1 nitrates Amino group and carboxyl group
Amino group and carboxyl group Amino group and carboxyl group
Amino group and carboxyl group In group out group
In group out group Group yourself or group yourselves
Group yourself or group yourselves