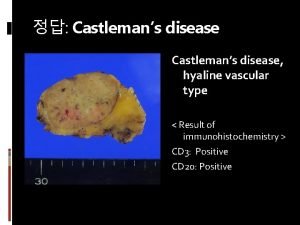
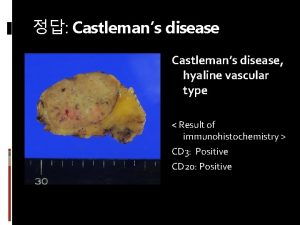
Castleman Disease 12152010 Castlemans Disease Angiofollicular lymph node
- Slides: 10
Castleman Disease 12_15_2010
Castleman’s Disease • Angiofollicular lymph node hyperplasia – Lymphoproliferative disorder • characterized by nodal expansions that usually leave the structure of the underlying lymph node at least partially intact • linked to excessive release of interleukin IL-6 • May be an association with HHV-8
Unicentric Disease • isolated benign lymphoproliferative disorder of young adults that is unassociated with HHV-8 infection and generally curable with surgical resection • vast majority of patients are asymptomatic – Diagnosed incidentally on imaging • The median size of the lesion was 5 to 9 cm – 70 percent located in the mediastinum or hilum of the lung, with abdominal sites the next most frequent – Peripheral lymphadenopathy is unusual – laboratory abnormalities were seen in less than 25 percent • anemia, elevated sedimentation rate, hypergammaglobulinemia
Unicentric Disease • Treatment – Complete resection is curative – No reports of recurrence – Systemic symptoms resolve as well – Partially resected masses may remain asymptomatic for years • Radiation • Rituximab (case report)
Unicentric Disease • Complications – May have increased risk of lymphoma – Paraneoplastic pemphigus
Multicentric Disease • May be associated with HIV • Median age in 50’s, but may be earlier in HIV+ pts • Non-specific symptoms suggestive of inflammatory disease – Fever, night sweats, weight loss, fatigue – Less than 10% are asymptomatic
Multicentric Disease • peripheral lymphadenopathy • Hepato – splenomegaly in 50% of cases • anemia, hypoalbuminemia, hypergammaglobulinemia, and an elevated sedimentation rate • associated with increased levels of a variety of cytokines, most notably IL-10 and IL-6
Multicentric Disease • patterns of disease progression – Indolent – can persist for months to years without progression – episodic relapsing form may be aggressive for a short period and then remit spontaneously or in response to treatment, only to recur at a later time – rapidly progressive form that can lead to death within weeks may be more common in HIV+ patients
Multicentric Disease • Complications – Most pts die of fulminant infection, progressive disease or related malignancies • Kaposi sarcoma • Hodgkin and non-Hodgkin lymphoma
Multicentric Disease • Treatment – Steroids – 60 -70% response rate – Chemotherapy – Anti-viral agents – Inhibition of IL-6 – tocilizumab – Thalidomide – Rituximab
 Lymph tends to stall inside lymph nodes
Lymph tends to stall inside lymph nodes Lymph tends to stall inside lymph nodes. this is due to
Lymph tends to stall inside lymph nodes. this is due to Lymph node diagram
Lymph node diagram Lymph node structure
Lymph node structure Supraclavicular lymph nodes picture
Supraclavicular lymph nodes picture Picture of swollen epitrochlear lymph nodes
Picture of swollen epitrochlear lymph nodes Lymph node dissection
Lymph node dissection Lymph node hard
Lymph node hard Sentinel lymph node biopsy indications
Sentinel lymph node biopsy indications Sln mamma
Sln mamma Lymph node structure
Lymph node structure