Awake Craniotomy Role in Neurosurgical Management Christine Stewart
- Slides: 15
Awake Craniotomy: Role in Neurosurgical Management Christine Stewart University of Minnesota, MS 4
Outline • Case R. P. • Classic indications and exclusion criteria • Factors to consider when defining eloquent areas • Recommendations
R. P. • 42 RHM w/ long history of seizures recently changed in character, worsening H/A over past several months. Wife notes increasing apathy, slow processing • Difficulty with word-finding, long-term memory, mood-swings • Other PMHx: – Cyclist v. car 1983: LOC 1 -2 minutes, right frontal frx w/ CSF leak meningitis – 1 st seizure 1985 GTC w/ auras – Another episode of meningitis 1985 intracranial abscess R. frontal lobe R. frontal craniotomy – Imaging from 2002 -2008 show a hypodensity in the left frontal lobe which was interpreted as encephalomalcia given hx – Hypothyroidism • Medications: – Lamictal 400 mg – Vimpat 200 mg BID – Levothyroxine
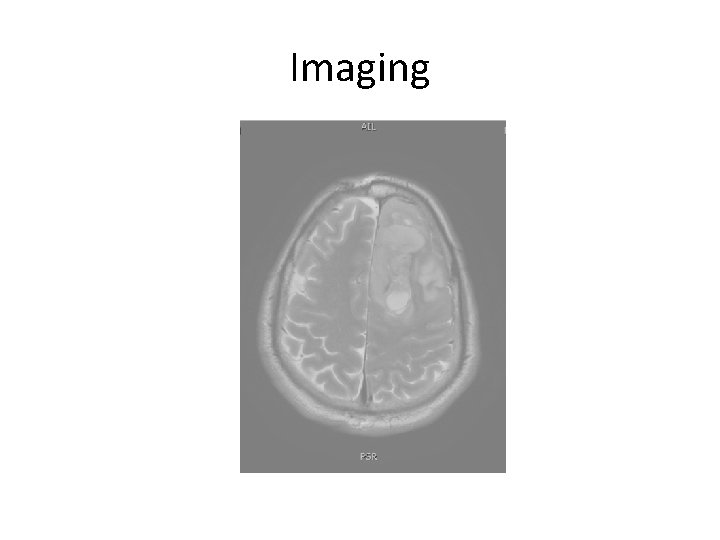
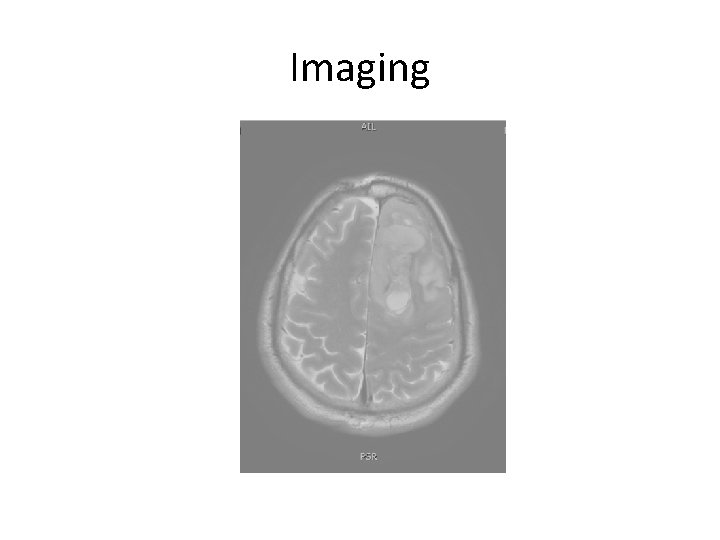
Imaging
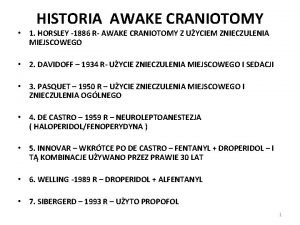
Classic Indications for Awake Craniotomy 1 • Surgery in ‘eloquent’ brain – Near motor strip – Speech/language centers – Thalamus • Removal of brainstem tumors • Search for a focus of seizure activity
Exclusion Criteria 2, 3, 4 • Inability to cooperate: dysphasia, language barrier, emotional labiality, cognitive impairment • Low occipital tumors • Tumors with significant dural attachment • Patients < 11 years old 5
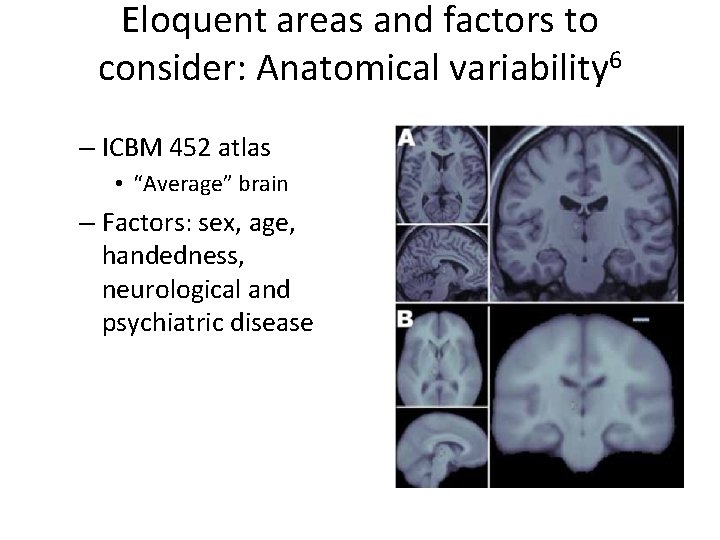
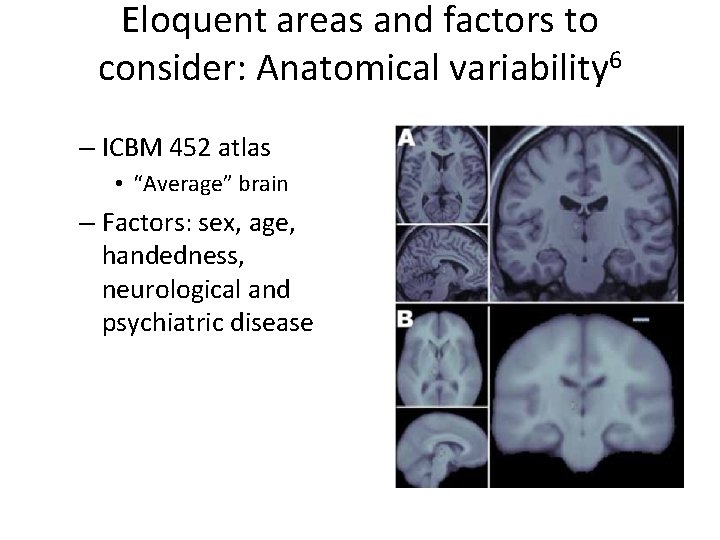
Eloquent areas and factors to consider: Anatomical variability 6 – ICBM 452 atlas • “Average” brain – Factors: sex, age, handedness, neurological and psychiatric disease
Eloquent areas and factors to consider: Functional variability 6, 7, 8 – Even areas with the same anatomical landmarks may not harbor the same underlying function • Motor cortex variability: – “Hand knob” of pre-central gyrus can represent primary motor cortex or premotor cortex – Stimulation in pre-central cortex can result in sensory and motor responses or motor responses in > 1 motor group – Primary motor area may extend > 20 mm anterior to the central sulcus
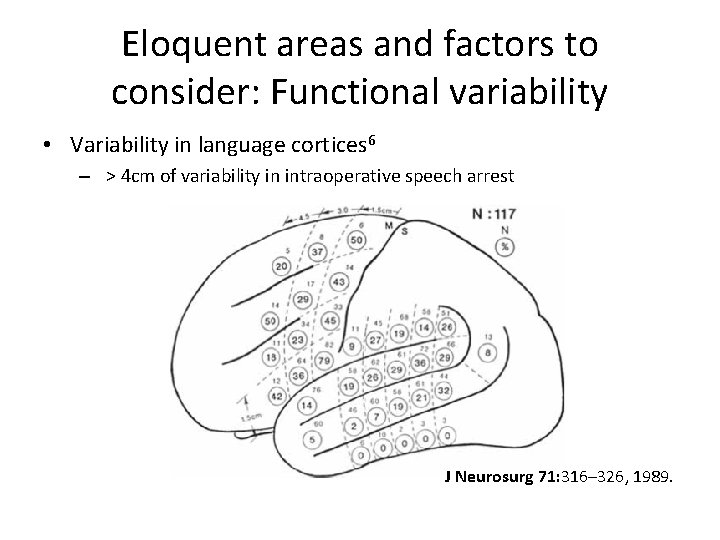
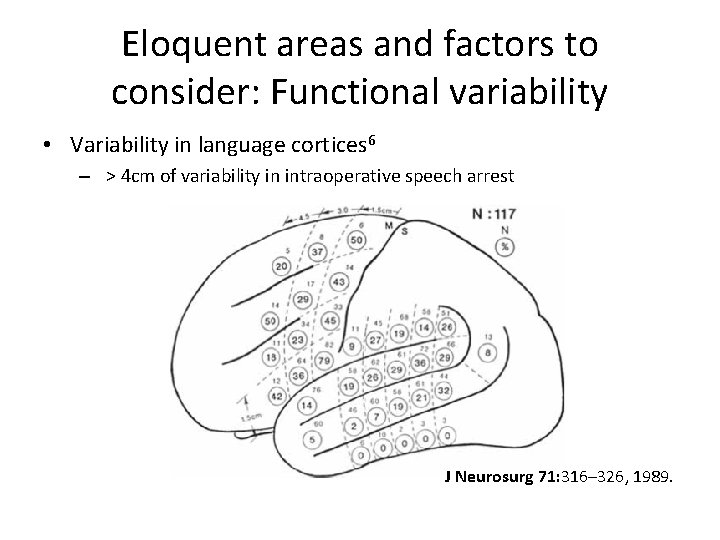
Eloquent areas and factors to consider: Functional variability • Variability in language cortices 6 – > 4 cm of variability in intraoperative speech arrest J Neurosurg 71: 316– 326, 1989.
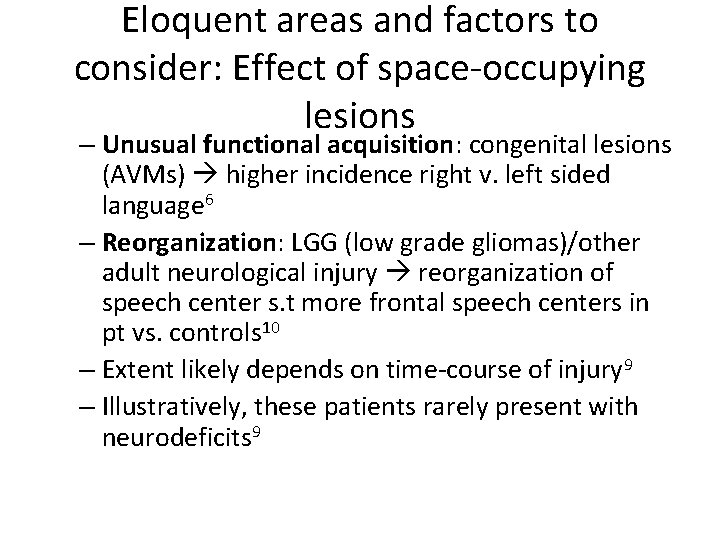
Eloquent areas and factors to consider: Effect of space-occupying lesions – Unusual functional acquisition: congenital lesions (AVMs) higher incidence right v. left sided language 6 – Reorganization: LGG (low grade gliomas)/other adult neurological injury reorganization of speech center s. t more frontal speech centers in pt vs. controls 10 – Extent likely depends on time-course of injury 9 – Illustratively, these patients rarely present with neurodeficits 9
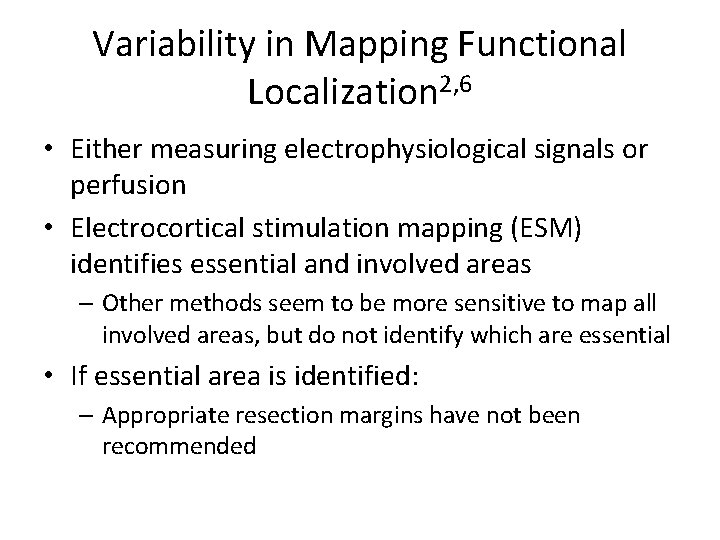
Variability in Mapping Functional Localization 2, 6 • Either measuring electrophysiological signals or perfusion • Electrocortical stimulation mapping (ESM) identifies essential and involved areas – Other methods seem to be more sensitive to map all involved areas, but do not identify which are essential • If essential area is identified: – Appropriate resection margins have not been recommended
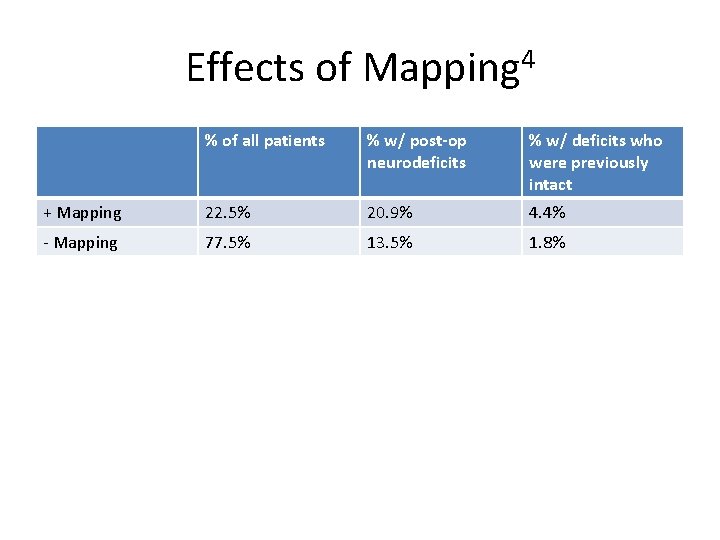
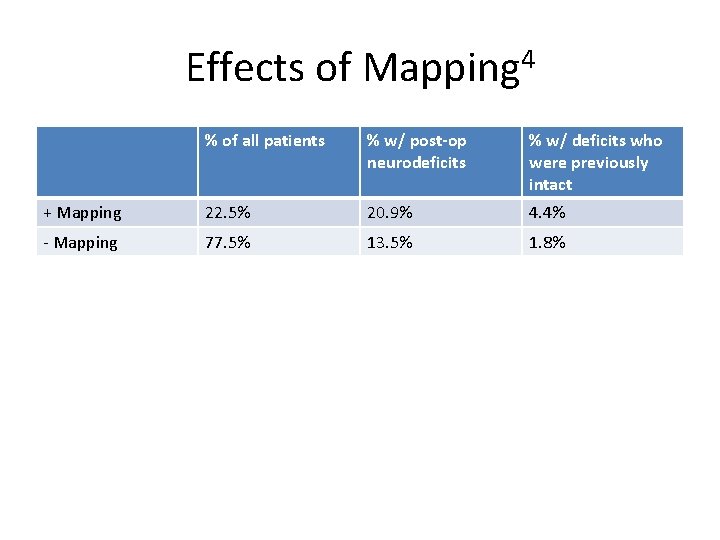
Effects of Mapping 4 % of all patients % w/ post-op neurodeficits % w/ deficits who were previously intact + Mapping 22. 5% 20. 9% 4. 4% - Mapping 77. 5% 13. 5% 1. 8%
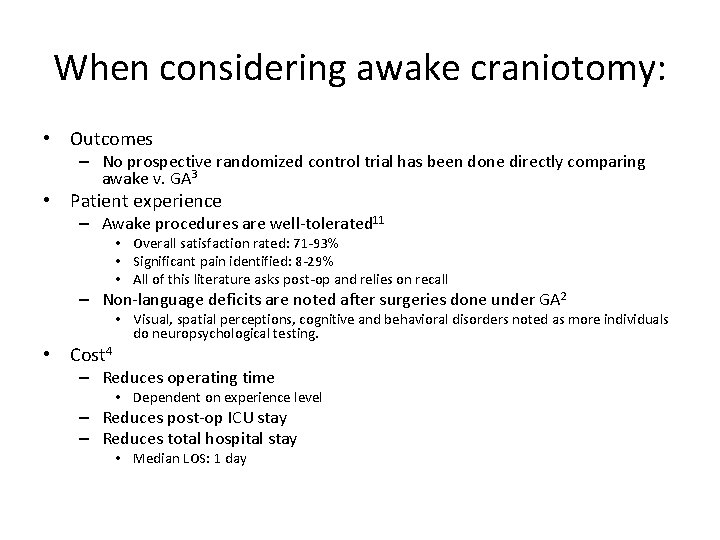
When considering awake craniotomy: • Outcomes – No prospective randomized control trial has been done directly comparing awake v. GA 3 • Patient experience – Awake procedures are well-tolerated 11 • Overall satisfaction rated: 71 -93% • Significant pain identified: 8 -29% • All of this literature asks post-op and relies on recall – Non-language deficits are noted after surgeries done under GA 2 • Cost 4 • Visual, spatial perceptions, cognitive and behavioral disorders noted as more individuals do neuropsychological testing. – Reduces operating time • Dependent on experience level – Reduces post-op ICU stay – Reduces total hospital stay • Median LOS: 1 day
Recommendations • No ‘gold standards’ for pre-operative mapping b/c no outcomes-correlated evidence – f. MRI at minimum – DTI may help define white matter tracts in and around the lesion – Others: MEG, PET • Intra-operative monitoring should be mandatory – only technique with validated outcomes measures
References 1 Greenberg, M. Handbook of Neurosurgery. 7 th edition. 2 Duffau, H. Awake surgery for non-language mapping. Neurosurgery. 66: 523 -529, 2010. 3 Kirsch, B. and Bernstein, M. Ethical challenges with awake craniotomy for tumor. Can. J. Neurol Sci 39: 78 -82, 2012. 4 Serletis, D. and Bernstein, M. Prospective study of awake craniotomy used routinely and nonselectively for supratentorial tumors. J Neurosurgery. 107: 1 -6, 2007. 5 Berger, MS. The impact of technical adjuncts in surgical management of cerebral low grade gliomas of childhood. J. of neuro-oncology. 1996; 28: 129 -155. 6 Pourtrain, N. and Bookheimer, S. Reliability of anatomy as a predictor of eloquence: a review. Neurosurg Focus 28: E 3, 2010. 7 Shinoura N, Suzuki Y, Yamada R, Tabei Y, Saito K, Yagi K: Precentral knob corresponds to the primary motor and premotor area. Can J Neurol Sci 36: 227– 233, 2009 8 Uematsu S, Lesser R, Fisher RS, et al: Motor and sensory cortex in humans: topography studied with chronic subdural stimulation. Neurosurgery 31: 59– 72, 1992 9 Desmurget M, Bonnetblanc F, Duffau H: Contrasting acute and slow-growing lesions: a new door to brain plasticity. Brain 130: 898– 914, 2007 10 Lucas TH II, Drane DL, Dodrill CB, Ojemann GA: Language reorganization in aphasics: an electrical stimulation mapping investigation. Neurosurgery 63: 487– 497, 2008 11 Manchella, S. et al. The experience of patients undergoing awake craniotomy for excision of intracranial masses: expectations, recall, satisfaction and functional outcome. British Journal of Neurosurgery. June 2011. 25(3): 391 -400.
 Oculocardiac reflex pathway
Oculocardiac reflex pathway Steriotaxis
Steriotaxis Awake the united states
Awake the united states Food to stay awake
Food to stay awake Save us lord while we are awake
Save us lord while we are awake Figures of speech in the poem animals by walt whitman
Figures of speech in the poem animals by walt whitman Buddha i am awake
Buddha i am awake Awake
Awake Trauma bond meaning
Trauma bond meaning Only that day dawns to which we are awake
Only that day dawns to which we are awake Irregular verb meet
Irregular verb meet Awake dbs
Awake dbs Elizabethan drama introduction
Elizabethan drama introduction Wide awake drawing close stirred by grace
Wide awake drawing close stirred by grace Save us lord while we are awake
Save us lord while we are awake Christ is risen from the grave come awake
Christ is risen from the grave come awake