Altered Mental Status Sean Ruland D O Professor

- Slides: 15

Altered Mental Status Sean Ruland, D. O. Professor Department of Neurology
Outline Terminology Diagnosis Work-up Specific etiologies and treatments Appropriate consultation
Terminology and Definition Encephalopathy Diffuse cerebral dysfunction Acute (onset hours to days) encephalopathy = delirium = acute confusional state
Clinicoanatomical Correlation Ascending reticular activating system impairment (ARAS) Impaired arousal (hypoactive delirium) Occasionally agitated delirium
History Collateral sources of information often necessary Define temporal course Past medical and surgical history DM; hepatic, renal, and thyroid disorders; and mental illness Comprehensive medication reconciliation ETOH and illicit substance use Baseline cognitive function
General Examination ABCs Intubation may be required Respiratory rate, depth, and pattern Autonomic dysregulation Core temperature Inspection Signs of trauma, jaundice, petechial hemorrhage, ecchymosis, spider angiomata, needle tracks and evidence of skin popping, pressure ulcers (prolonged immobility) Breath odor ETOH, acetone (ketoacidosis), fetid (uremia) Palpation Hepatomegaly, nodular liver, ascites
Neurologic Examination Altered sensorium Ranges from mild inattention to coma (waxes and wanes) Pitfall—eye opening apraxia Impaired cognition Meningeal signs Papilledema Pupillary function Mydriasis—central herniation, HIE, anticholinergic or sympathomimetic exposure Miosis—opioid or organophosphate exposure, pontine injury, advanced age Asymmetry—uncal herniation, previous ocular injury, midbrain damage, Horner syndrome
Neurologic Examination Eye movements Dysconjugate gaze but typically oculocephalic and oculovestibular reflexes present Decreased saccades, nystagmus, frank ophthalmoplegia Corneal and pharyngeal reflexes typically present unless severe Motor Asterixis, diffuse myoclonus, extrapyramidal signs, symmetrical posturing, upgoing plantar responses
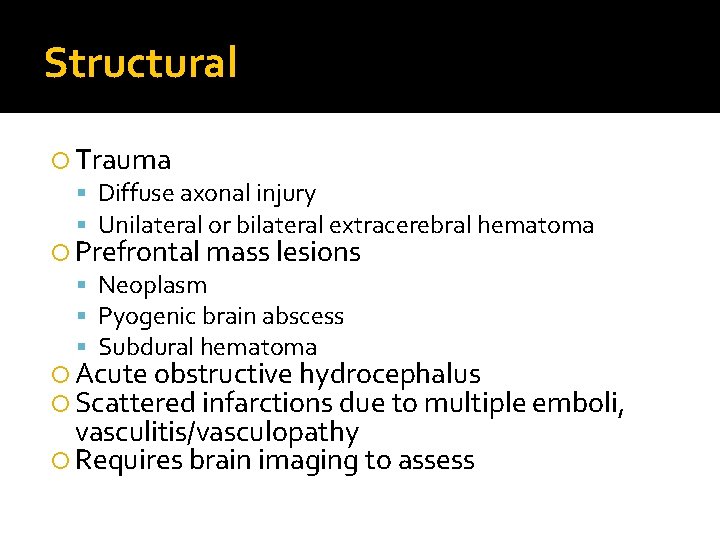
Structural Trauma Diffuse axonal injury Unilateral or bilateral extracerebral hematoma Prefrontal mass lesions Neoplasm Pyogenic brain abscess Subdural hematoma Acute obstructive hydrocephalus Scattered infarctions due to multiple emboli, vasculitis/vasculopathy Requires brain imaging to assess
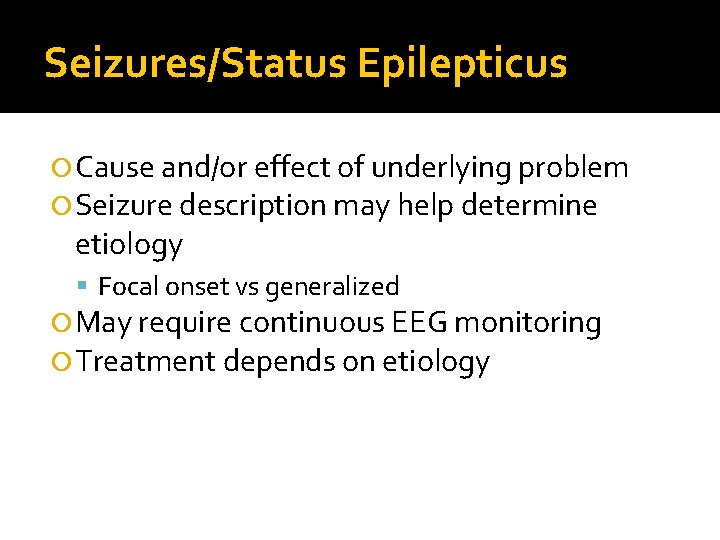
Seizures/Status Epilepticus Cause and/or effect of underlying problem Seizure description may help determine etiology Focal onset vs generalized May require continuous EEG monitoring Treatment depends on etiology
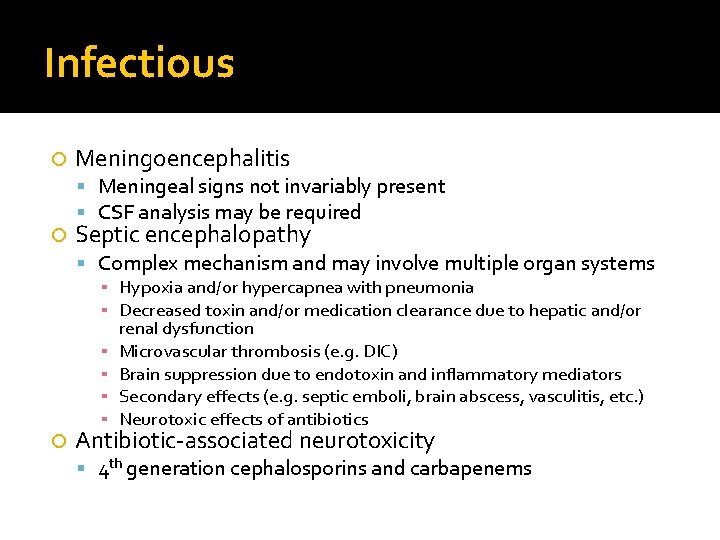
Infectious Meningoencephalitis Meningeal signs not invariably present CSF analysis may be required Septic encephalopathy Complex mechanism and may involve multiple organ systems ▪ Hypoxia and/or hypercapnea with pneumonia ▪ Decreased toxin and/or medication clearance due to hepatic and/or ▪ ▪ renal dysfunction Microvascular thrombosis (e. g. DIC) Brain suppression due to endotoxin and inflammatory mediators Secondary effects (e. g. septic emboli, brain abscess, vasculitis, etc. ) Neurotoxic effects of antibiotics Antibiotic-associated neurotoxicity 4 th generation cephalosporins and carbapenems
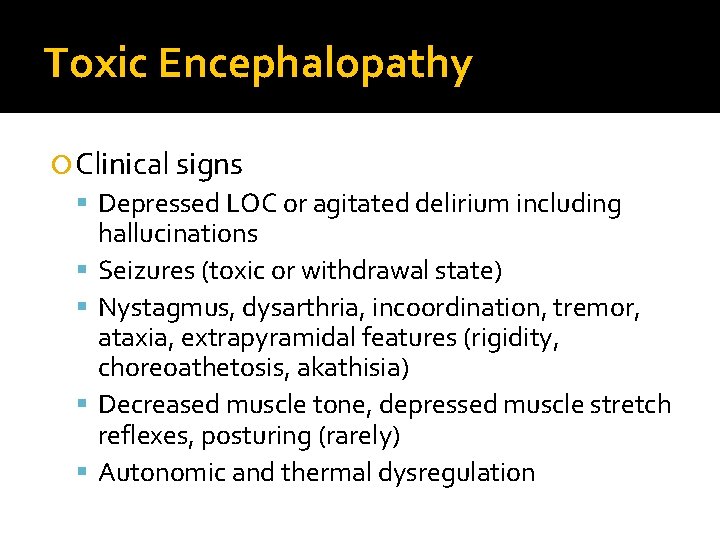
Toxic Encephalopathy Clinical signs Depressed LOC or agitated delirium including hallucinations Seizures (toxic or withdrawal state) Nystagmus, dysarthria, incoordination, tremor, ataxia, extrapyramidal features (rigidity, choreoathetosis, akathisia) Decreased muscle tone, depressed muscle stretch reflexes, posturing (rarely) Autonomic and thermal dysregulation
Toxic Encephalopathy Offending agents ETOH and illicits Sedative-hypnotics and narcotic analgesics ▪ Benzos and barbs may cause acute respiratory failure ▪ Flumazenil (caution as may cause seizures) ▪ Opiates (pinpoint pupils, respiratory depression—naloxone) Neuroleptics (neuroleptic malignant syndrome) ▪ Rigidity, hyperpyrexia, elevated CK and transaminases, leukocytosis ▪ Dopamine agonist and dantrolene Anti-seizure medication ▪ ▪ ▪ Cerebellar syndrome Levetiracetam (agitated delirium) Valproic acid (hyperammonemia) Acute phenytoin exposure (ophthalmoplegia, extrapyramidal signs) Barbiturates (cardiotoxicity, hypothermia) Antidepressants (serotonin syndrome) ▪ Similar to NMS with tremor, myoclonus, and/or hyperreflexia Anticholinergic medication (H 1 and H 2 blockers) Immunosuppressants ▪ CSA and tacrolimus (PRES—visual changes, seizures, impaired consciousness, MRI findings) Iodinated contrast-induced encephalopathy (PRES)
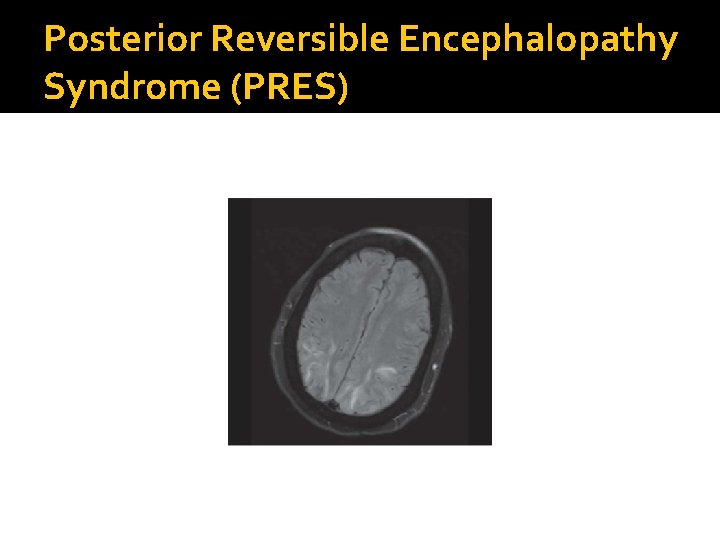
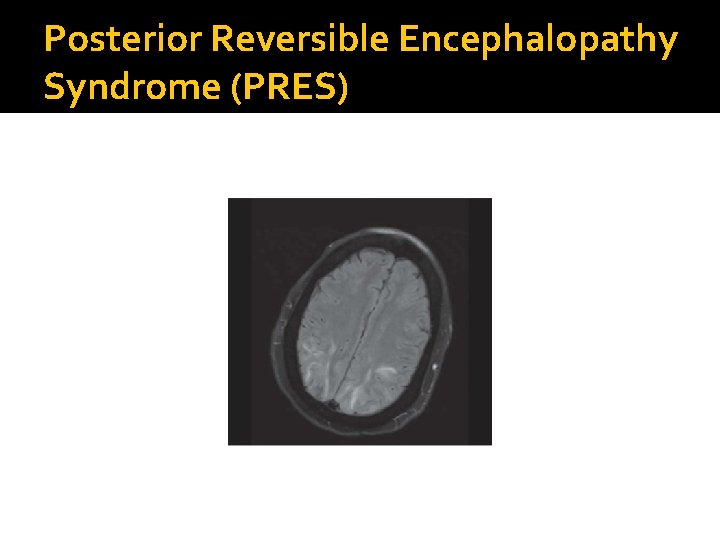
Posterior Reversible Encephalopathy Syndrome (PRES)
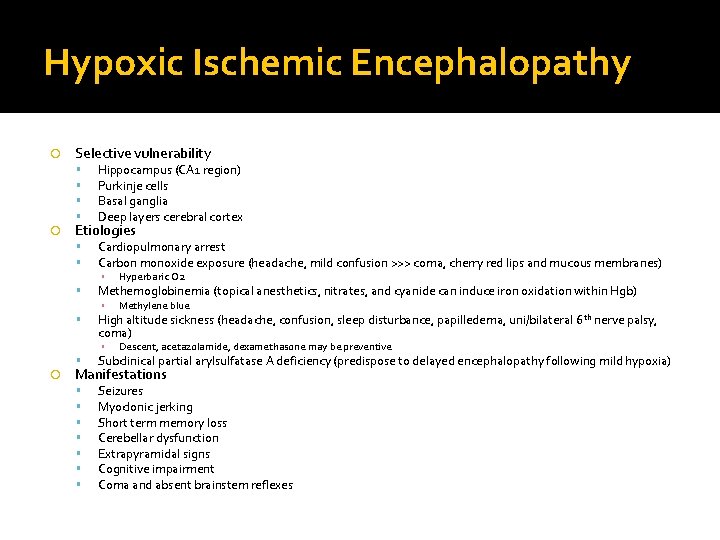
Hypoxic Ischemic Encephalopathy Selective vulnerability Hippocampus (CA 1 region) Purkinje cells Basal ganglia Deep layers cerebral cortex Cardiopulmonary arrest Carbon monoxide exposure (headache, mild confusion >>> coma, cherry red lips and mucous membranes) Methemoglobinemia (topical anesthetics, nitrates, and cyanide can induce iron oxidation within Hgb) Etiologies ▪ ▪ Methylene blue High altitude sickness (headache, confusion, sleep disturbance, papilledema, uni/bilateral 6 th nerve palsy, coma) ▪ Hyperbaric O 2 Descent, acetazolamide, dexamethasone may be preventive Subclinical partial arylsulfatase A deficiency (predispose to delayed encephalopathy following mild hypoxia) Seizures Myoclonic jerking Short term memory loss Cerebellar dysfunction Extrapyramidal signs Cognitive impairment Coma and absent brainstem reflexes Manifestations
 Dr sean ruland
Dr sean ruland Promotion from assistant to associate professor
Promotion from assistant to associate professor Robert ruland
Robert ruland Cornelia m. ruland
Cornelia m. ruland Robert ruland
Robert ruland Mncd slums
Mncd slums Status mental psikiatri
Status mental psikiatri Jarvis chapter 5 mental status assessment
Jarvis chapter 5 mental status assessment Overvalued ideas
Overvalued ideas Grimasen adalah
Grimasen adalah Mental status examination purpose
Mental status examination purpose Loose thought process
Loose thought process Perubahan status mental
Perubahan status mental Linear thought process mental status
Linear thought process mental status Mental status
Mental status Mental status examination
Mental status examination