AACEM and AAAEM Panel Discussion Emergency Department Patient

- Slides: 14
AACEM and AAAEM Panel Discussion Emergency Department Patient Flow Maximizing Patient Throughput and Addressing Patient Satisfaction J. Scheulen, Johns Hopkins L. Davis-Moon, Thomas Jefferson 10/19/2021 1
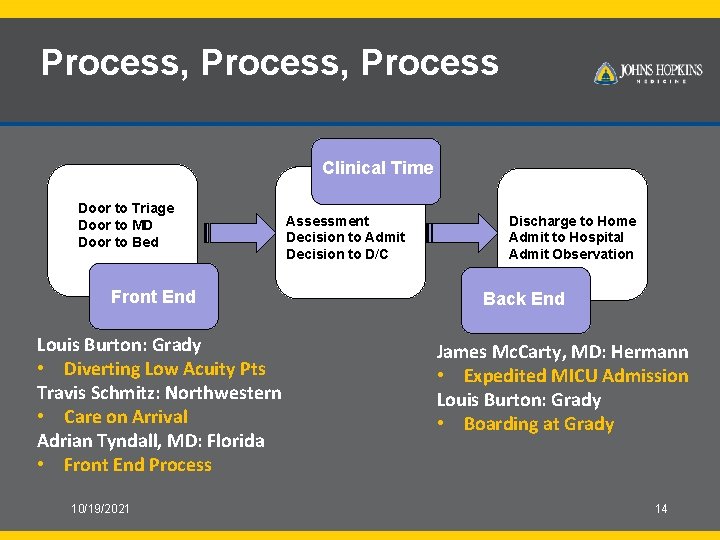
Patient Throughput Panel Discussants • Travis Schmitz, Northwestern – Care on Arrival • Louis Burton, Grady – Low acuity patient re-direction • Adrian Tyndall, MD, Florida – Front end operational changes • James Mc. Carty MD, Hermann Hospital – Expedited MICU Admission • Louis Burton, Grady – Boarding---What’s that? ? • Jim Scheulen, Johns Hopkins – Simulation Modeling ED Operations • Ted Christopher, MD, Thomas Jefferson – Patient Satisfaction 10/19/2021 2
EMERGENCY DEPARTMENT PATIENT THROUGHPUT 10/19/2021 3
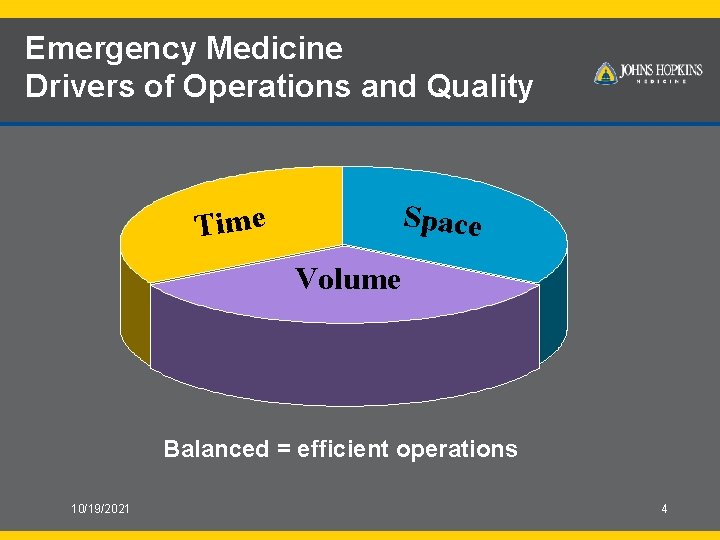
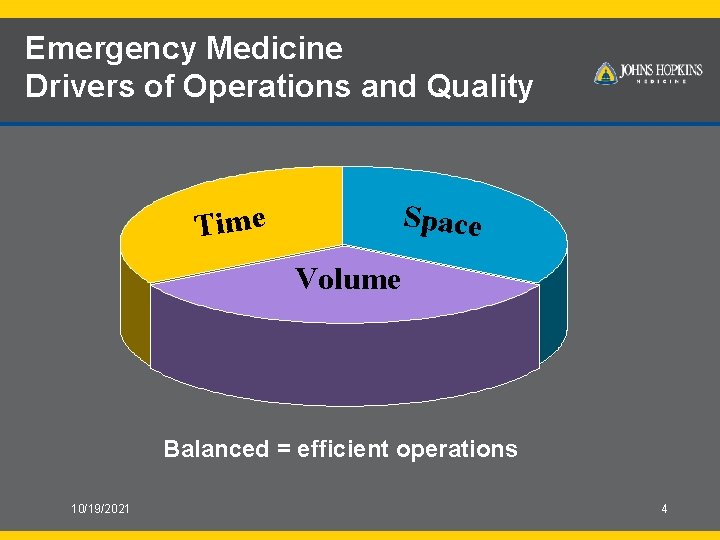
Emergency Medicine Drivers of Operations and Quality Space Time Volume Balanced = efficient operations 10/19/2021 4
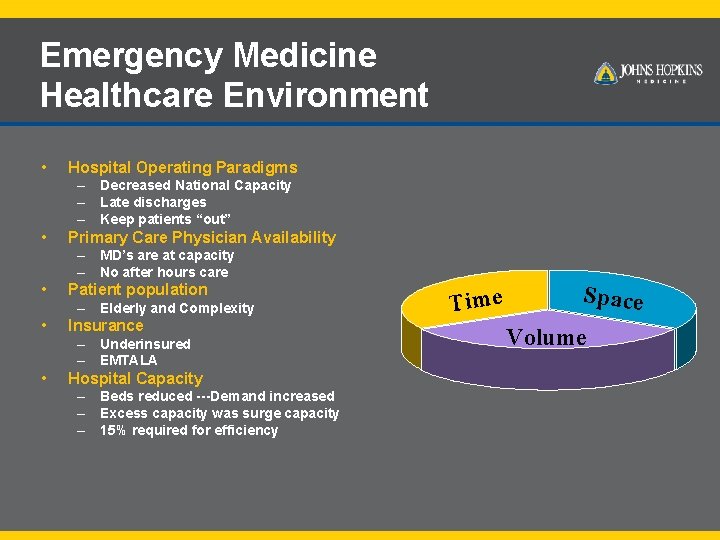
Emergency Medicine Healthcare Environment • Hospital Operating Paradigms – Decreased National Capacity – Late discharges – Keep patients “out” • Primary Care Physician Availability – MD’s are at capacity – No after hours care • Patient population – Elderly and Complexity • Insurance – Underinsured – EMTALA • Hospital Capacity – Beds reduced ---Demand increased – Excess capacity was surge capacity – 15% required for efficiency Time Space Volume
Emergency Medicine Service Expectations Drive thru if possible!!! • • 24 Hour Service Minimal Waiting Time Demand Based Service Different Expectations AND A Different Standard – It’s okay to wait days for my MD but not hours in ED • Convenience and Episodic Care
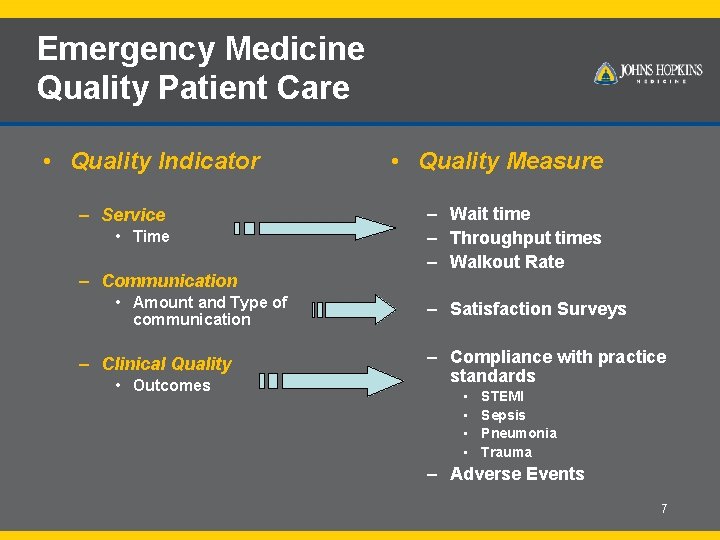
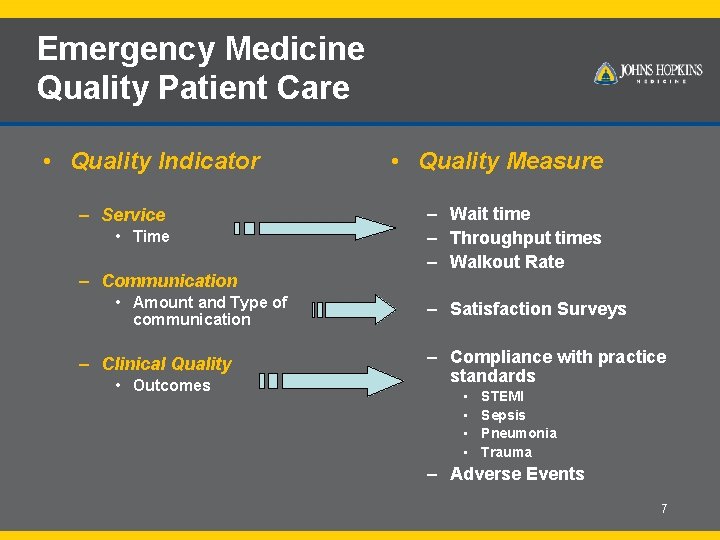
Emergency Medicine Quality Patient Care • Quality Indicator – Service • Time – Communication • Amount and Type of communication – Clinical Quality • Outcomes • Quality Measure – Wait time – Throughput times – Walkout Rate – Satisfaction Surveys – Compliance with practice standards • • STEMI Sepsis Pneumonia Trauma – Adverse Events 7

Time is central to Quality = Time Emergency Medicine 10/19/2021 8
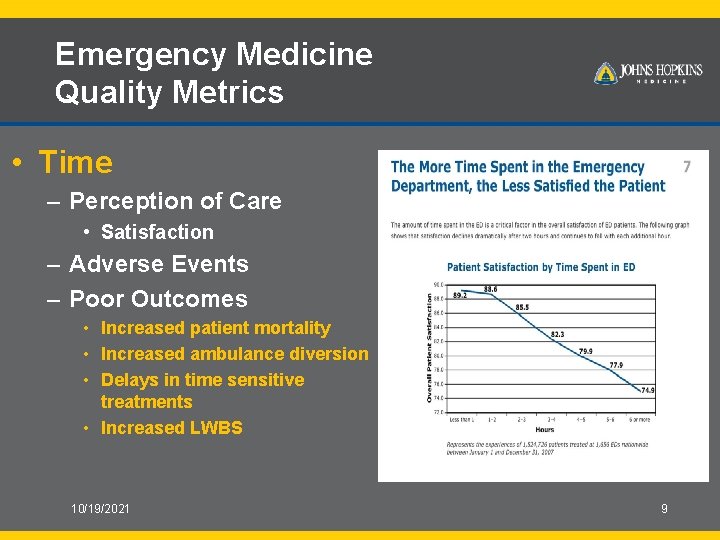
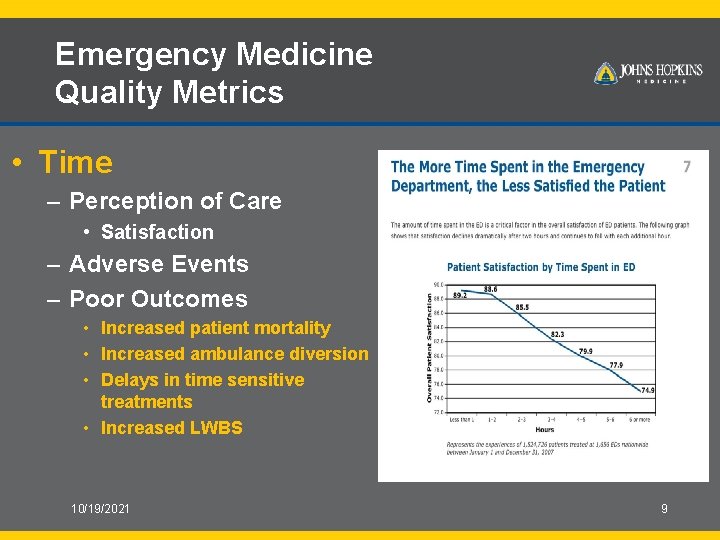
Emergency Medicine Quality Metrics • Time – Perception of Care • Satisfaction – Adverse Events – Poor Outcomes • Increased patient mortality • Increased ambulance diversion • Delays in time sensitive treatments • Increased LWBS 10/19/2021 9
Emergency Medicine All about Process Segmenting Patient Flow in the ED Process Time Moderate Acuity Level 3 Med/Surg Dx and Rx Likely Discharge Complex medical Dx and Rx Possible Admission Main ED Clinical Decision Unit
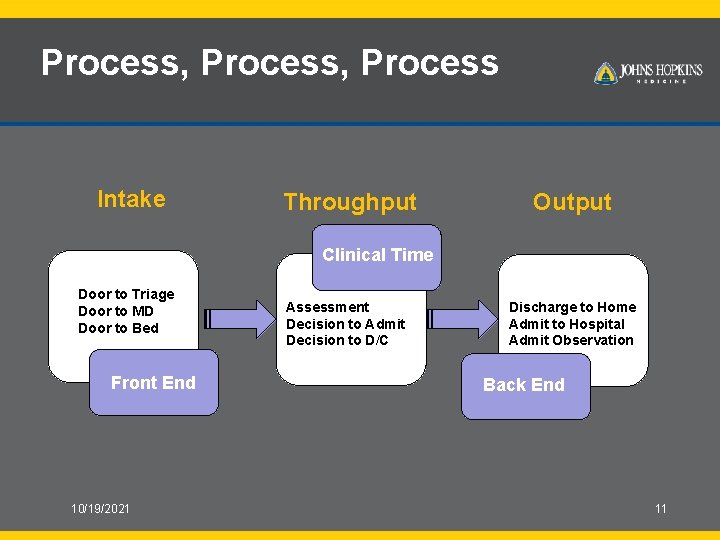
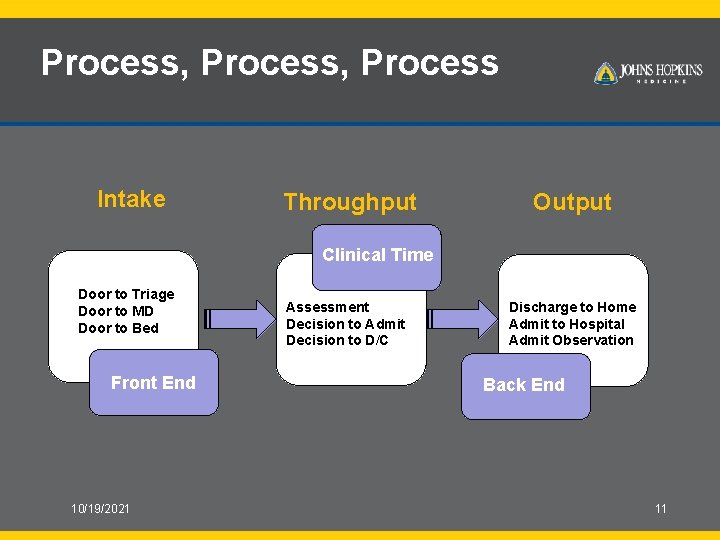
Process, Process Intake Throughput Output Clinical Time Door to Triage Door to MD Door to Bed Front End 10/19/2021 Assessment Decision to Admit Decision to D/C Discharge to Home Admit to Hospital Admit Observation Back End 11
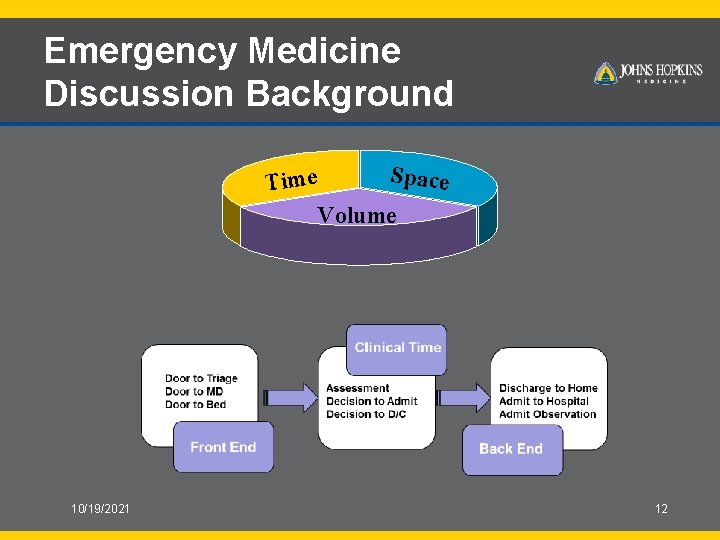
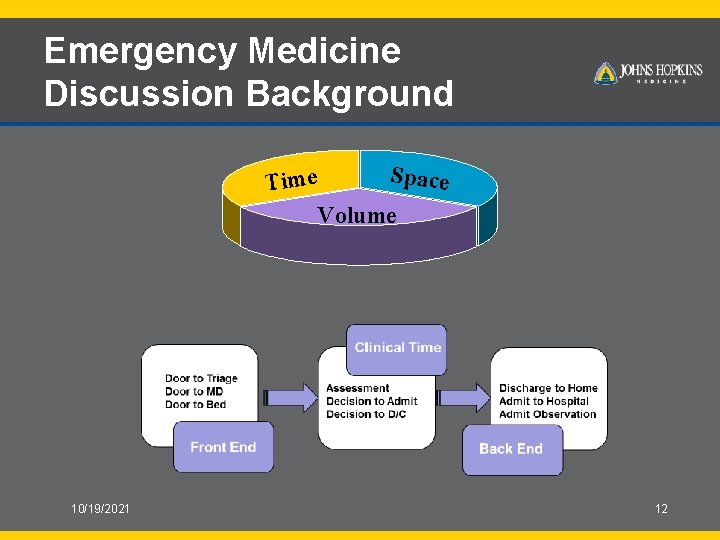
Emergency Medicine Discussion Background Space Time Volume 10/19/2021 12
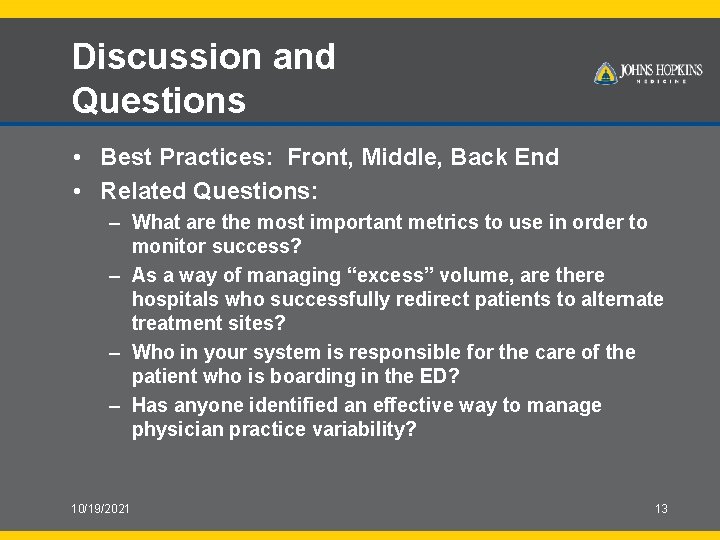
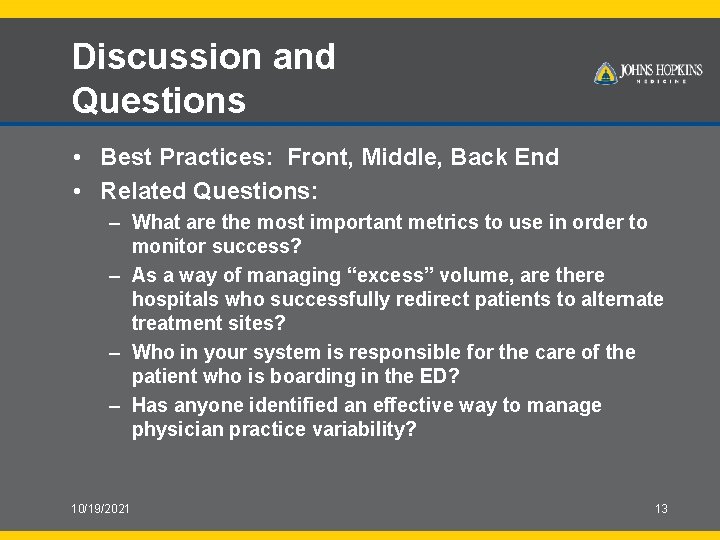
Discussion and Questions • Best Practices: Front, Middle, Back End • Related Questions: – What are the most important metrics to use in order to monitor success? – As a way of managing “excess” volume, are there hospitals who successfully redirect patients to alternate treatment sites? – Who in your system is responsible for the care of the patient who is boarding in the ED? – Has anyone identified an effective way to manage physician practice variability? 10/19/2021 13
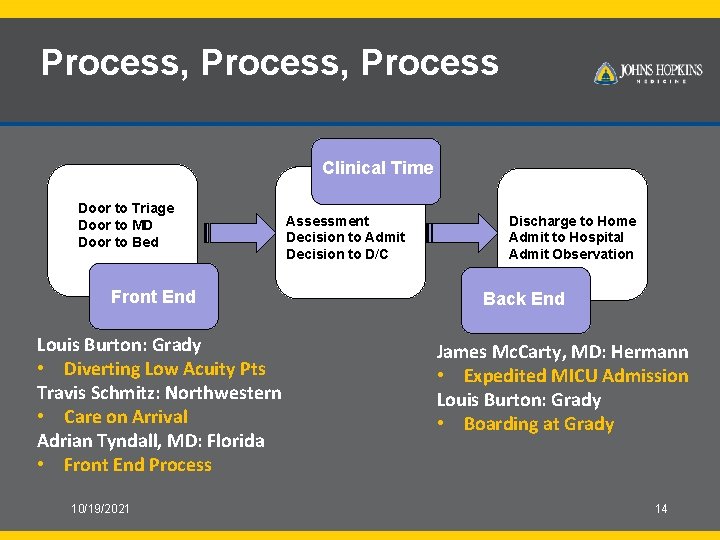
Process, Process Clinical Time Door to Triage Door to MD Door to Bed Front End Louis Burton: Grady • Diverting Low Acuity Pts Travis Schmitz: Northwestern • Care on Arrival Adrian Tyndall, MD: Florida • Front End Process 10/19/2021 Assessment Decision to Admit Decision to D/C Discharge to Home Admit to Hospital Admit Observation Back End James Mc. Carty, MD: Hermann • Expedited MICU Admission Louis Burton: Grady • Boarding at Grady 14
 Continuous panel vs discontinuous panel
Continuous panel vs discontinuous panel Zıt panel tekniği
Zıt panel tekniği Objectives of labelling
Objectives of labelling Panel discussion definition
Panel discussion definition Sharon soper
Sharon soper Group discussion topics in tamil
Group discussion topics in tamil Patient panel size
Patient panel size Types of lifting and moving patients
Types of lifting and moving patients Discussion of simple distillation
Discussion of simple distillation Patient 2 patient
Patient 2 patient Emergency room nurse orientation
Emergency room nurse orientation Whittington emergency department
Whittington emergency department Northwick park emergency department
Northwick park emergency department Sfgh emergency department
Sfgh emergency department How to reorder artboards in illustrator
How to reorder artboards in illustrator