Vision Healthy people families and communities VP Quarterly



- Slides: 37
Vision: Healthy people, families and communities. VP Quarterly Report on Strategies Q 3 – 2015/16 VP: David Mc. Cutcheon – Physician Services & Integrated Health Services Multi-year Plans: - Wait 1/Access to Specialists and Diagnostics Multi-year Plan - Appropriateness Multi-year Plan - Physician Engagement Multi-year Plan - Medicine Service Line Multi-year Plan

Portfolio Overview • Medicine Service Line – – Emergency Department / EMS Critical Care & Cardiosciences Units Medicine Inpatient Units Medicine KOT • Physician Services – – Senior Medical Office Department Heads Practitioner Staff Affairs Practitioner Advisory Committee
Wait 1 Multi-year Plan
Wait 1/ Access to Specialist & Diagnostics Multi-year Plan 2015 -16 Provincial Outcome • By March 31 2019, there will be a 50% decrease in wait time for appropriate referral from primary care provider to all specialists or diagnostics. – By March 31, 2016, the provincial framework for an appropriate referral to specialists or diagnostics will be implemented in at least four new clinical areas within two service lines.
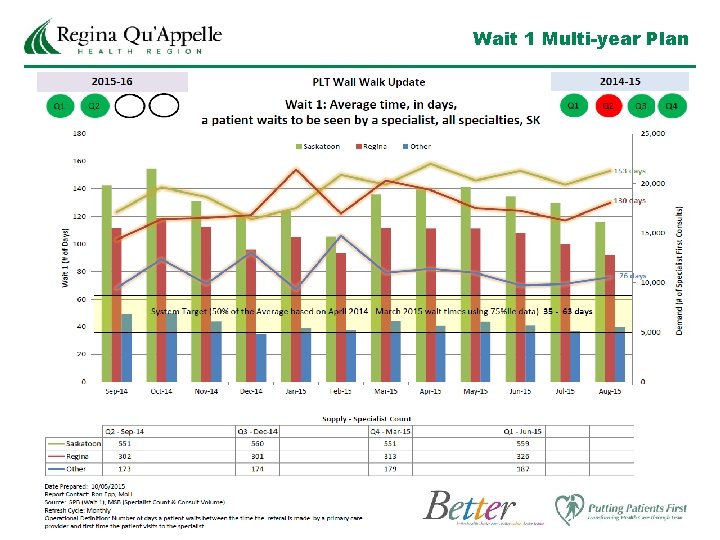
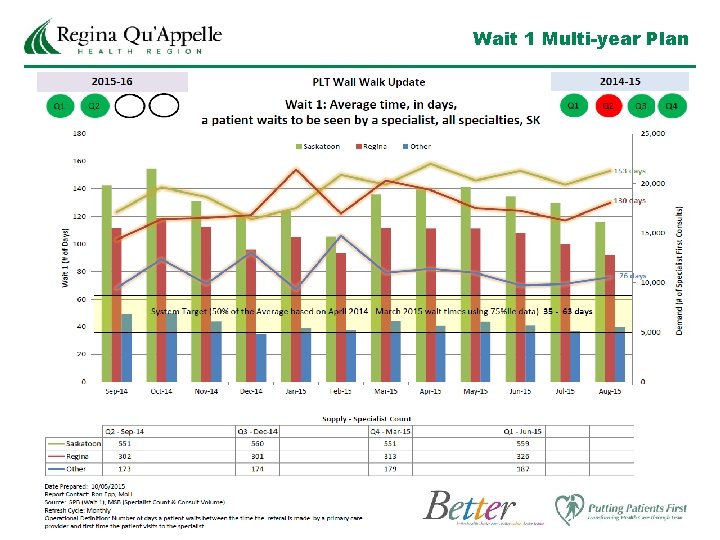
Wait 1 Multi-year Plan
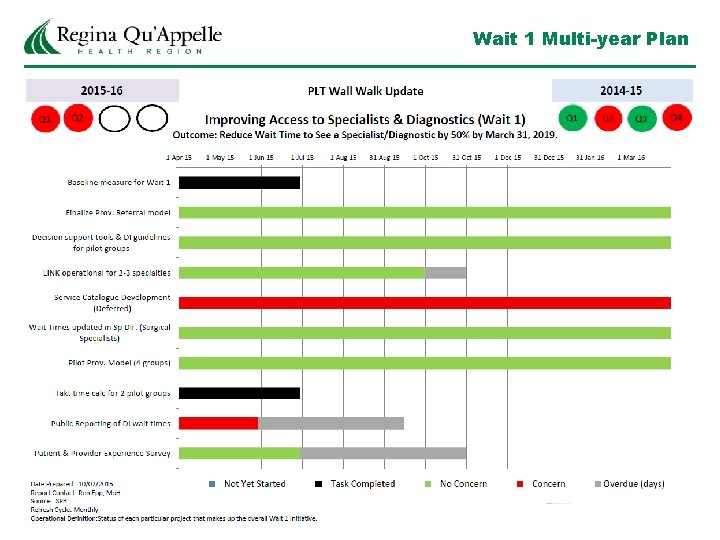
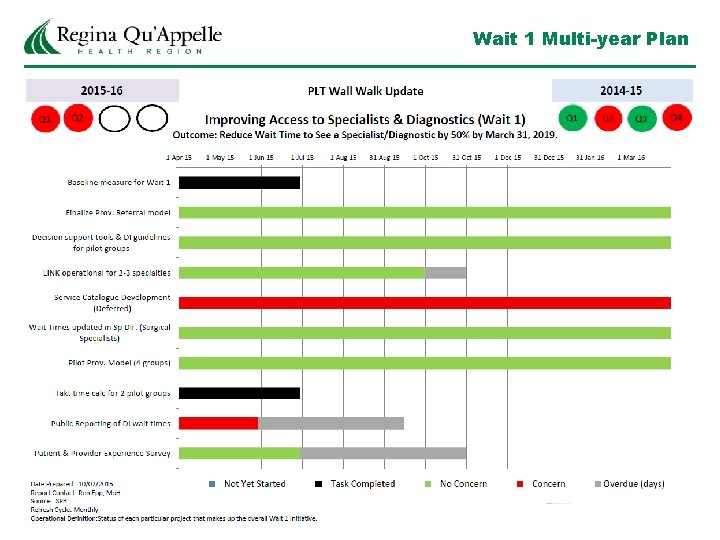
Wait 1 Multi-year Plan
Status of Strategy Implementation Successes/What is working • Program is on target for eight of the ten parameters • Saskatchewan began posting current and historical wait times for Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) wait times on Saskatchewan. ca on October 22, 2015. • The Hip and Knee Treatment and Research Centre has begun surveying patient satisfaction in Q 1 and will begin using an online survey tool later this fall. This tool was developed so that it can easily be adapted to measure patient satisfaction in other service lines.
Status of Strategy Implementation – Challenges & Risks Challenges/Gaps/Risks • Orthopedic Pooled referrals • Challenge to the process by Saskatchewan Family Doctors at the SMA regional assembly. • Challenge reiterated by RQHR Department of Family Medicine. • Decision by the Orthopedic Section to withdraw from the process was made. • Therefore Wait 1 times will be much more difficult to assess.
Appropriateness Of Care “Better Care, Made Easier” Multi-year Plan
Appropriateness Of Care Multi-year Plan 2015/16 Provincial Outcome & Improvement Targets (Note: New language still under review) • By March 31, 2018, 80% of clinicians in 3 selected clinical areas within two or more service lines will be utilizing agree upon best practices. – By March 31, 2017, there will be at least 2 clinical areas that have deployed care standards at the provincial level.
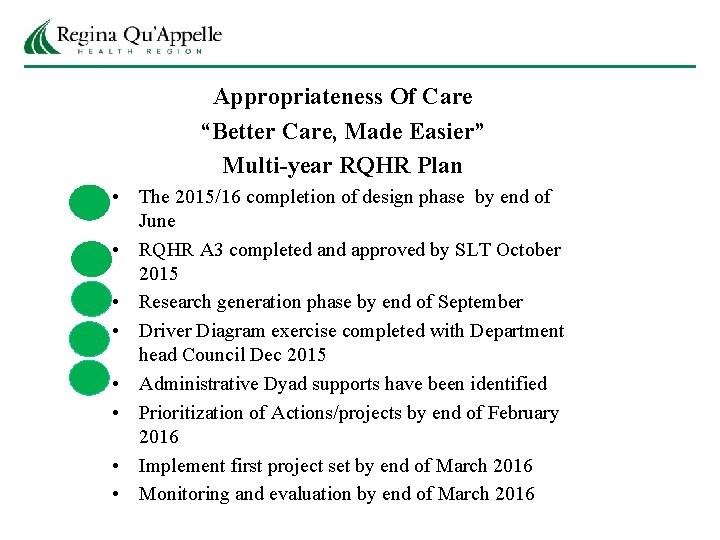
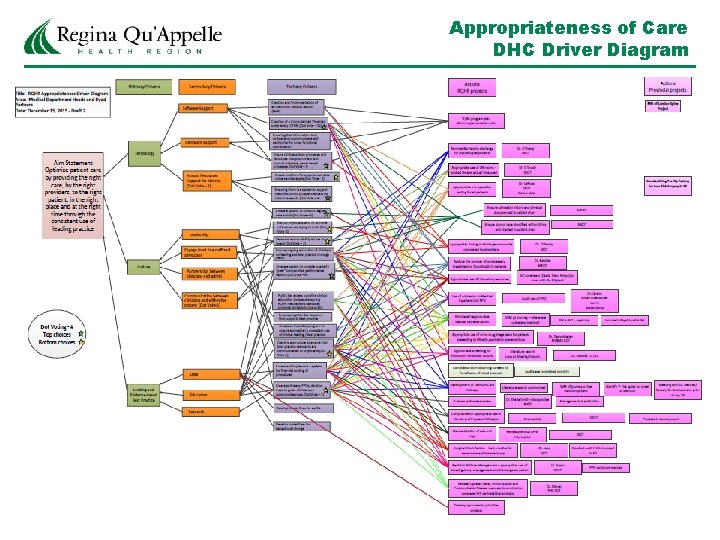
Appropriateness Of Care “Better Care, Made Easier” Multi-year RQHR Plan • The 2015/16 completion of design phase by end of June • RQHR A 3 completed and approved by SLT October 2015 • Research generation phase by end of September • Driver Diagram exercise completed with Department head Council Dec 2015 • Administrative Dyad supports have been identified • Prioritization of Actions/projects by end of February 2016 • Implement first project set by end of March 2016 • Monitoring and evaluation by end of March 2016
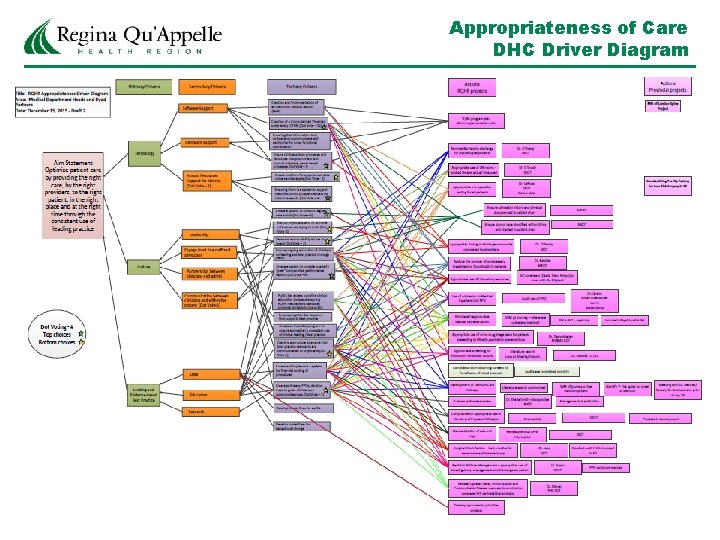
Appropriateness of Care DHC Driver Diagram
Appropriateness of Care RQHR Strategies Researched best practices and organizational initiatives lead to these 6 strategies 1 Replication of Intermountain Health strategies 2 Choosing Wisely 3 Review of RQHR PPO strategy 4 Review of current RQHR Clinical Guidelines/Pathways 5 Appropriate resource use 6 Other : Surgery – indication; extent; procedure : Records Management
Appropriateness of Care RQHR Projects • Appropriate use of Laboratory resources – Laboratory Medicine • Avoid inappropriate bladder catheterization – Medicine, GIM, FM • Surgical Site Infection – best practice for caesareans and hysterectomy – Obstetrics &Gynecology • Reduce the number of unnecessary investigations for critically ill patients – Critical Care • Appropriate pre-operative testing for all patients – Anesthesia/Surgery (Provincial initiative – RQHR actively participating)
Appropriateness of Care RQHR Projects (cont. ) • Use of admission to Medical Inpatient Unit PPO – FM, Hospitalist, GIM • Compliance with obtaining consent for Transfusion of blood products – Laboratory Medicine • Development of Delirium Care Pathway – Emergency Medicine (possibility of a Provincial Plan rollout) • Complete Travel, Immunization and Communicable Disease manuals; immunization coverage; HIV perinatal transmission – PPHS • Appropriate use of urine drug triage tests for patients presenting to ER with psychiatric presentations - Psychiatry

Appropriateness of Care RQHR Projects (cont. ) • Appropriate screening for Pulmonary Embolism – Emergency Medicine, Radiology • Compliance for appropriate use of Stroke and Prostate Pathways – Surgery and Radiology • Standardization of sets and trays – Ortho and Neuro surgery • Appropriate timing of discharge summaries completed by physicians; admission history and physical documented in patient chart; plan of care identified within 24 hrs and charted in patient chart – all departments
Physician Engagement Multi-year Plan
Physician Engagement Multi-year Plan RQHR OUTCOME • Biennially, the physician engagement survey will be completed with an engagement score of 55% in 2016 • By 2017, RQHR will reach an average employee and physician engagement score of 80%.
Physician Engagement Multi-year Plan The elements of the Multi-year Plan are: • Communication Plan – Providing timely information (Monthly) – Involvement in decision making – Listening – Resolving important issues affecting medical staff – Early Pregnancy Program • Collaboration Plan – Oversight Group Strategy: GIM – Development of Compacts: RAHD and in Orthopaedics; pending for Family Medicine • Accountability plan – Performance development – Complaints management – Bylaw and rules enforcement – final draft completed – Leadership development
Status of Strategy Implementation Successes/What is working - The development of a GIM oversight committee has promoted better communication between PH & RGH and provided a forum to implement and drive positive change - Department/Section retreats have been instrumental in discussing and creating solutions to current issues and strategizing for the future (20 Appropriateness of Care projects have been identified) - Physicians being empowered in their dyad and physician leadership roles (ACU) - Physician participation in the development of new service models that focuses on the patient (MSU, ACU and Psychiatry Hospitalist program) - The 2 nd Quarterly Physician Newsletter has been well received
Status of Strategy Implementation – Challenges & Risks Challenges/Gaps/Risks - The Department of Family Medicine structure needs to be redesigned to provide better support and communication to community based family physicians; Section of Family Medicine Obstetrics being created. -Departments of Surgery and Medicine need further support to be able to affectively deliver on the expectations of the organization. As a result, communication and/or dissemination of information is sometimes stalled. -The Department of Surgery is using an Executive Meeting Strategy to endeavor to improve communication. This strategy is also being proposed for the Department of Family Medicine
Physician Engagment Next Steps - Implement a new structure for the Department of Family Medicine - Development of a business plan to remunerate DHs in accordance with the ACFP model - Coordinate with HR for the 2016 Bi-annual staff and physician engagement survey - Continue to engage physicians in those Lean initiatives with clinical relevance - Continue the implementation of the Appropriateness of Care Agenda

Medicine Service Line Multi-year Plan
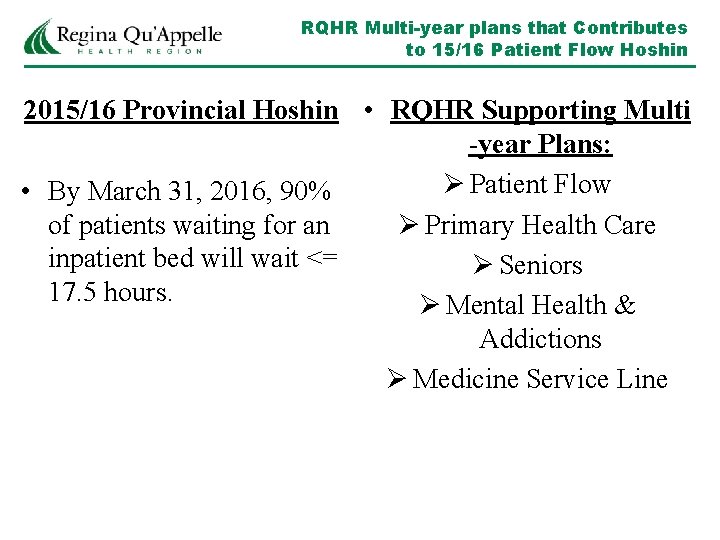
RQHR Multi-year plans that Contributes to 15/16 Patient Flow Hoshin 2015/16 Provincial Hoshin • RQHR Supporting Multi -year Plans: Ø Patient Flow • By March 31, 2016, 90% of patients waiting for an Ø Primary Health Care inpatient bed will wait <= Ø Seniors 17. 5 hours. Ø Mental Health & Addictions Ø Medicine Service Line
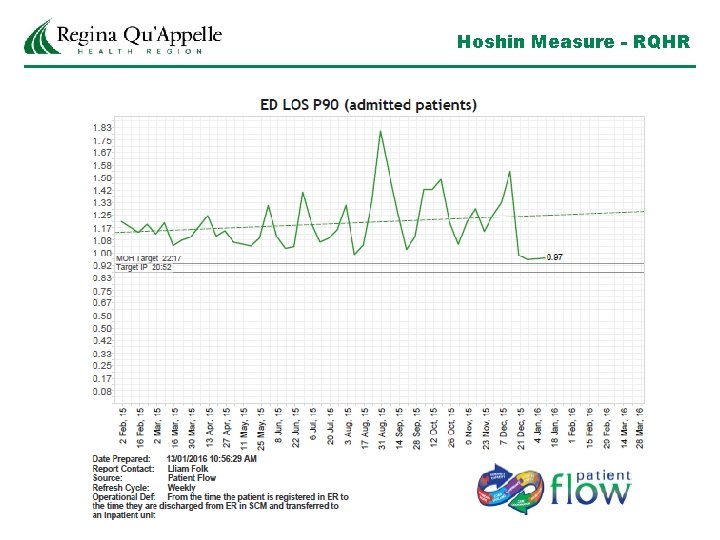
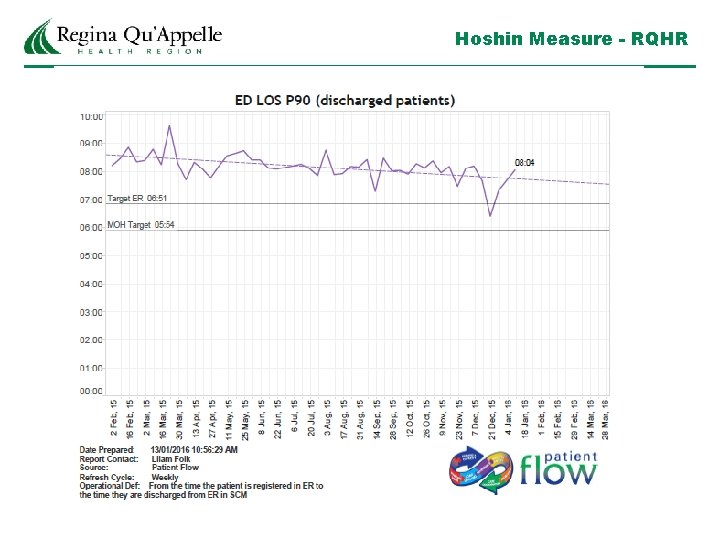
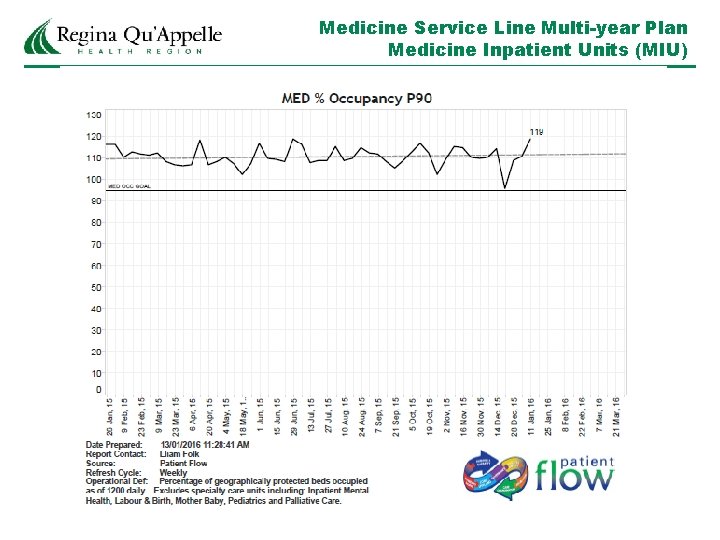
Medicine Service Line Multi-year Plan 2015/16 Provincial Outcome & Improvement Targets for Patient Flow By March 31, 2017 (funding dependent) updated target • 20% reduction in 90 th%ile ED Length of Stay (LOS) for admitted and Non-admitted patients. • 20% reduction in 90 th%ile Time Waiting for and Inpatient Bed (TWIB). • Decrease or no Increase in 30/60 day readmission rates to acute care. • Decrease or no increase in 7 day ED Revisit rates.
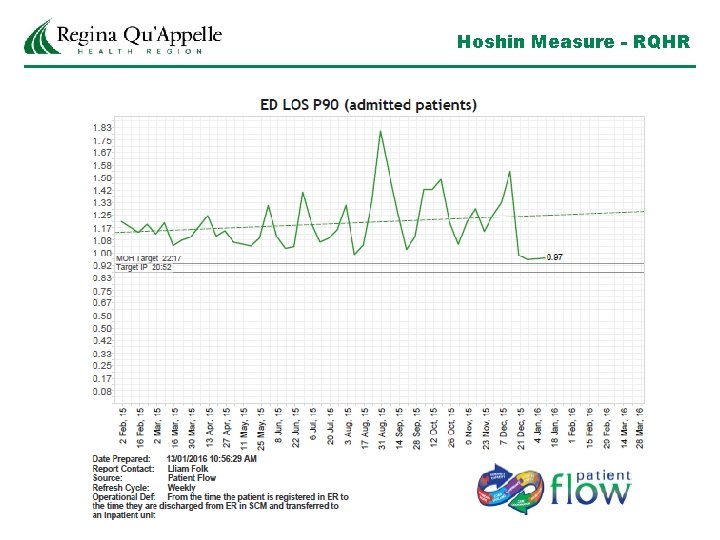
Hoshin Measure - RQHR
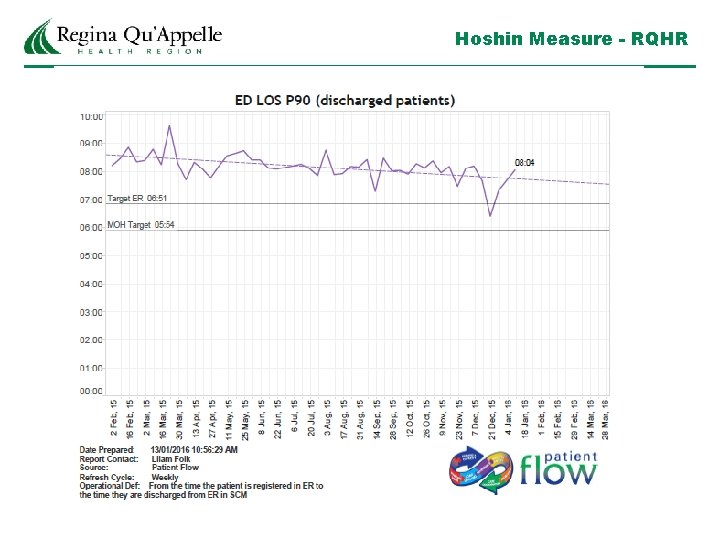
Hoshin Measure - RQHR
Medicine Service Line Multi-year Plan Medicine Inpatient Units (MIU) Medicine Inpatient Units Goal of 95%-0 -0: The work will focus on: 1) Advancing a high quality daily plan of care for each patient. 2) Identifying and removing barriers to advancing the care plan 3) Preventing iatrogenic effects of hospitalization for seniors 4) Preventing harm to all hospitalized patients (i. e. falls, med errors, infection transmission) 5) Driving to goal of admitting patients to the unit from the ER within 30 minutes of decision to admit (assuming bed ready and available)
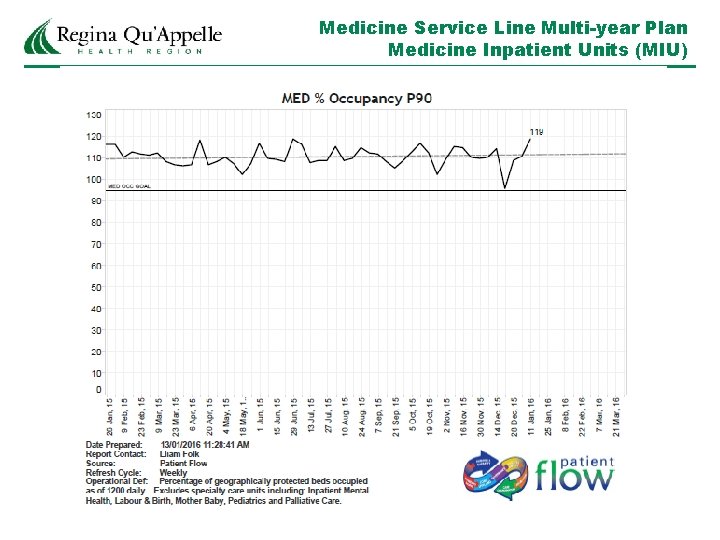
Medicine Service Line Multi-year Plan Medicine Inpatient Units (MIU)
Medicine Service Line Multi-year Plan Medicine Inpatient Units (MIU) Principle Strategies 1)Implement Accountable Care Unit - Model Line is unit 4 A at Pasqua Hospital (6 -12 month pilot). Replication to follow to all MIUs - Structured Interdisciplinary Bedside Rounds (SIBR) with unit based physicians - The rounds follow a standard process to advance the plan of each patient’s care - Appropriateness and patient safety issues are addressed within the process - Concurrent planning for discharge is incorporated - Patient and identified family members are participants in the rounds 2)Seniors Friendly Hospital - 33% of seniors over the age of 85 admitted to RQHR die. - Care issues include: - functional decline - medication toxicity - altered consciousness(delirium) - care transition - malnutrition/dehydration - polypharmacy - Gentle Persuasive Approach has been demonstrated to be the most effective strategy. Trainers were certified in mid-November and training for staff will be starting on March 1, 2016.
Medicine Service Line Multi-year Plan Critical Care and Cardio Sciences • Occupancy goal – 85% • Cardiac diagnostic scheduling in the process of being updated by Physician Partners • Medical Surveillance Unit transition to closed Hospitalist unit began Jan 15, 2016 ( mimic many components of ACU – SIBR and bedside rounding) • RFP posted for Electronic ECG system which will streamline information flow and access to cath lab • Evaluation of new in house orientation program to maximize training an minimize lag time in onboarding staff • ICU will trial roll out of IV pumps Feb 16/16. Regional roll out weeks of March 8 – and March 14/16
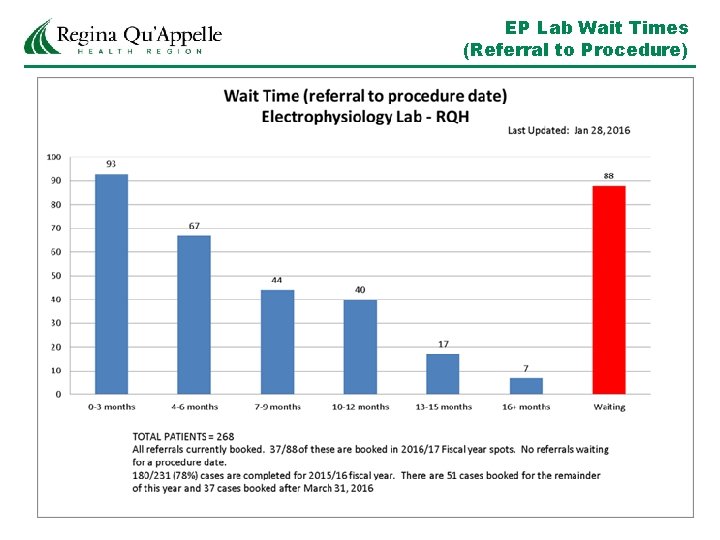
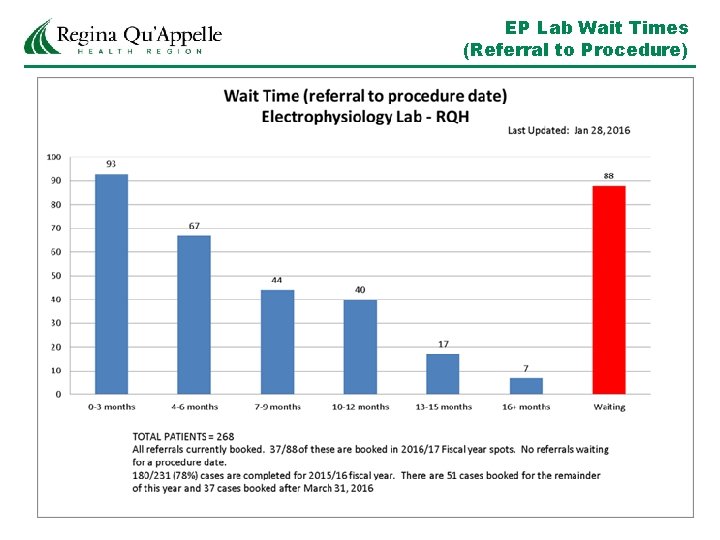
EP Lab Wait Times (Referral to Procedure)
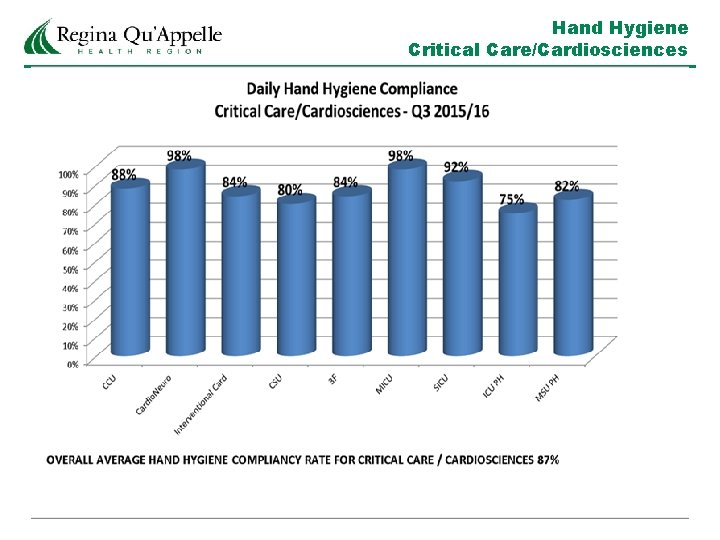
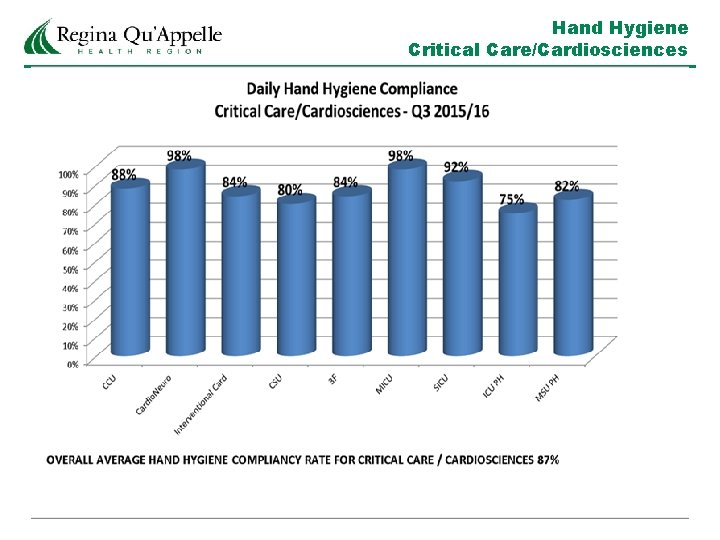
Hand Hygiene Critical Care/Cardiosciences
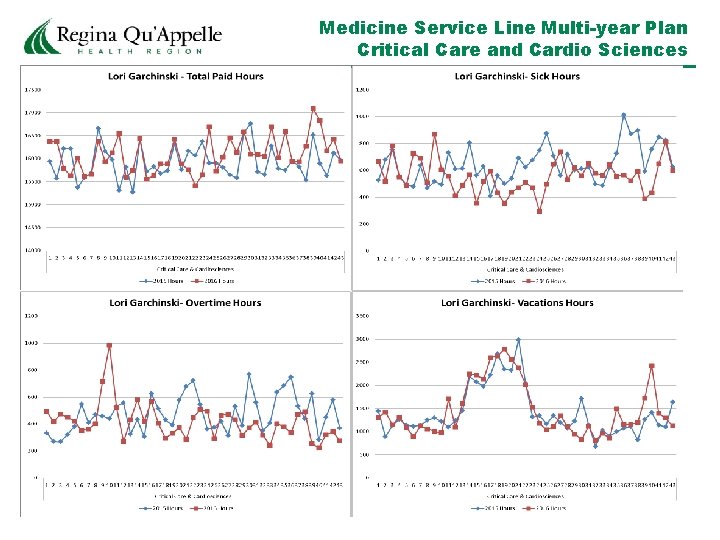
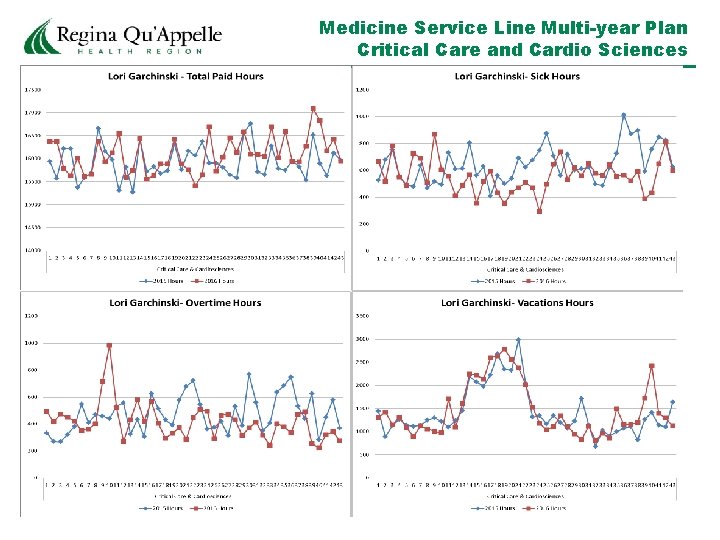
Medicine Service Line Multi-year Plan Critical Care and Cardio Sciences
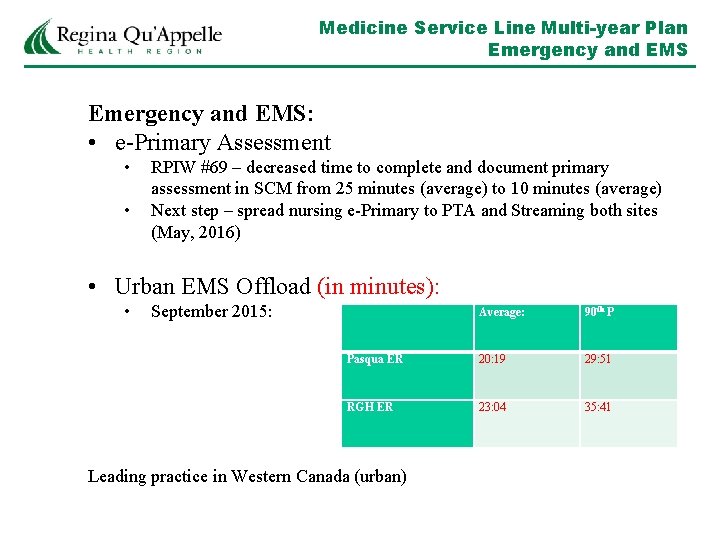
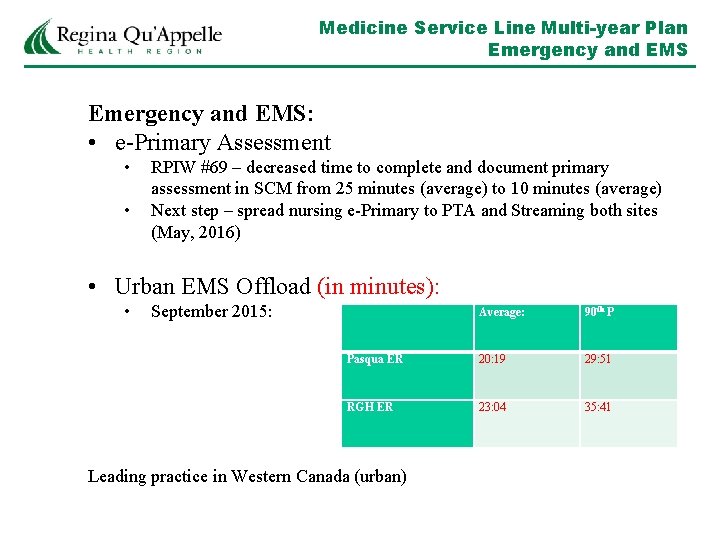
Medicine Service Line Multi-year Plan Emergency and EMS: • e-Primary Assessment • • RPIW #69 – decreased time to complete and document primary assessment in SCM from 25 minutes (average) to 10 minutes (average) Next step – spread nursing e-Primary to PTA and Streaming both sites (May, 2016) • Urban EMS Offload (in minutes): • September 2015: Average: 90 th P Pasqua ER 20: 19 29: 51 RGH ER 23: 04 35: 41 Leading practice in Western Canada (urban)
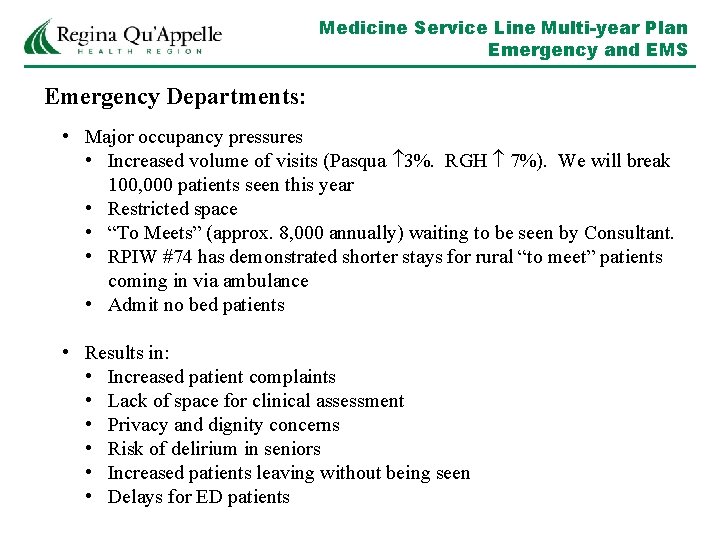
Medicine Service Line Multi-year Plan Emergency and EMS Emergency Departments: • Major occupancy pressures • Increased volume of visits (Pasqua 3%. RGH 7%). We will break 100, 000 patients seen this year • Restricted space • “To Meets” (approx. 8, 000 annually) waiting to be seen by Consultant. • RPIW #74 has demonstrated shorter stays for rural “to meet” patients coming in via ambulance • Admit no bed patients • Results in: • Increased patient complaints • Lack of space for clinical assessment • Privacy and dignity concerns • Risk of delirium in seniors • Increased patients leaving without being seen • Delays for ED patients
Medicine Service Line Multi-year Plan Emergency and EMS Emergency Departments: • Innovation • Use of community paramedics as part of PHC teams supporting complex patients at home, thus avoiding ED admission • Continued work and refinement on Patient Triage & Assessment process at RGH • Implementation of emergency physician e-charting (targeted for Pasqua go-live: spring, 2016) • Developing new Vacation management process (recommendation from RPIW #87) • “Unit Council” pilot at RGH (6 peer-elected staff to support leadership in the department and ensure front-line voice in decision -making) • Commenced work on core preceptor group for new orientees • Introduction of EARS (Early Assessment & Response Vital Signs Record) – March, 2016.
 Healthy forests healthy communities poster contest
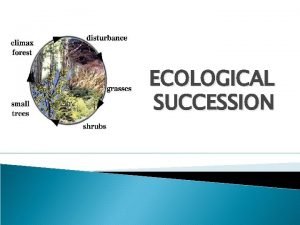
Healthy forests healthy communities poster contest What are the steps of primary succession
What are the steps of primary succession Little families
Little families Prop 206 arizona pros and cons
Prop 206 arizona pros and cons Bronx partners for healthy communities
Bronx partners for healthy communities Santa ana building healthy communities
Santa ana building healthy communities Identify four skills that families need to stay healthy
Identify four skills that families need to stay healthy Dc healthy families
Dc healthy families Healthy families new york
Healthy families new york Healthy food healthy mind journal
Healthy food healthy mind journal Healthy soil healthy life poster ideas
Healthy soil healthy life poster ideas Healthy nurse healthy nation
Healthy nurse healthy nation People living together in communities
People living together in communities The community i belong
The community i belong Russell quarterly economic and market review
Russell quarterly economic and market review Russell quarterly economic and market review
Russell quarterly economic and market review Healthy people 2020 goals
Healthy people 2020 goals Healthy people 2020 goals
Healthy people 2020 goals Healthy people 2020 goals
Healthy people 2020 goals Healthy people 2020 diabetes
Healthy people 2020 diabetes People in media vs people as media example
People in media vs people as media example Structured light
Structured light Quarterly business review examples
Quarterly business review examples Access quarterly package
Access quarterly package Quarterly gantt chart
Quarterly gantt chart Quarterly business review templates
Quarterly business review templates Kpi development template
Kpi development template Early childhood research quarterly impact factor
Early childhood research quarterly impact factor Quarterly business review templates
Quarterly business review templates Quarterly business review
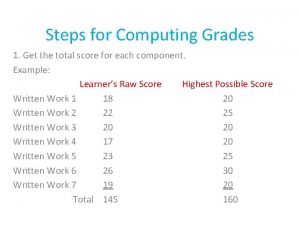
Quarterly business review Raw grade to transmuted
Raw grade to transmuted Fidelity quarterly market update q1 2018
Fidelity quarterly market update q1 2018 Experian
Experian Wv doc quarterly package program
Wv doc quarterly package program In the usa the big cia
In the usa the big cia Characteristics of ttl logic family
Characteristics of ttl logic family Compare and contrast the bach and marsalis families
Compare and contrast the bach and marsalis families Compare and contrast the bach and marsalis families
Compare and contrast the bach and marsalis families