The EPECO TM Education in Palliative and Endoflife







- Slides: 24
The EPEC-O TM Education in Palliative and End-of-life Care - Oncology Project The EPEC-O Curriculum is produced by the EPECTM Project with major funding provided by NCI, with supplemental funding provided by the Lance Armstrong Foundation.
E P E C EPEC – Oncology Education in Palliative and End-of-life Care – Oncology O Module 3 q Symptoms – Skin
Skin wounds. . . l Acute vs. chronic; likely to heal or not l Chemotherapy agent extravasation l Radiation damage l Decubitus ulcers l Malignant wounds

. . . Skin wounds Associated with l Pain l Depression l Anxiety l Poorer interpersonal interactions
Key points 1. Pathophysiology 2. Assessment 3. Management

Skin symptoms l Organ system l Highly innervated l Visible l Psychological, social, and spiritual l Interdisciplinary care l Symptom control

Chemotherapy extravasation: pathophysiology l Acute wound l Products of inflammation Redness Swelling Pain l Cell death Necrosis, open wound
Radiation: pathophysiology l Radiation damage l Acute wound l Products of inflammation l Cell death
Decubitus ulcers: pathophysiology l Pathophysiology Ischemia l Fat is protective
Malignant wounds: pathophysiology l Disrupted physiology l Products of inflammation l Neovascularization Bleeding l Necrosis Anaerobic and fungal infections
Assessment. . . l Acute versus chronic l By wound type
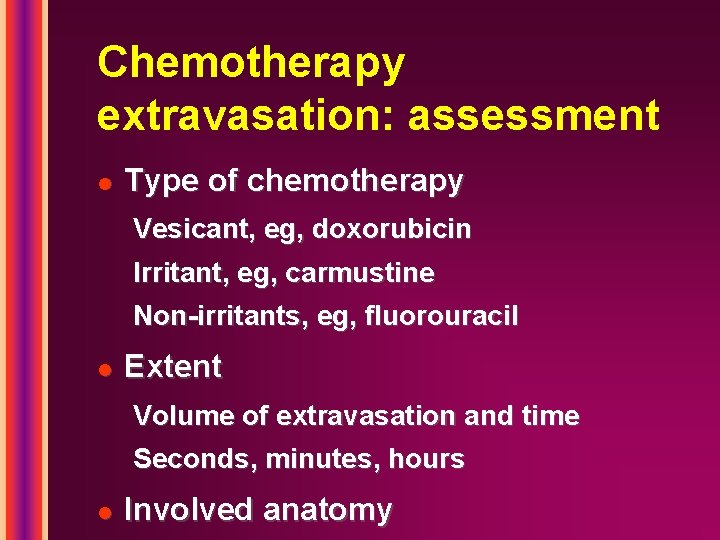
Chemotherapy extravasation: assessment l Type of chemotherapy Vesicant, eg, doxorubicin Irritant, eg, carmustine Non-irritants, eg, fluorouracil l Extent Volume of extravasation and time Seconds, minutes, hours l Involved anatomy
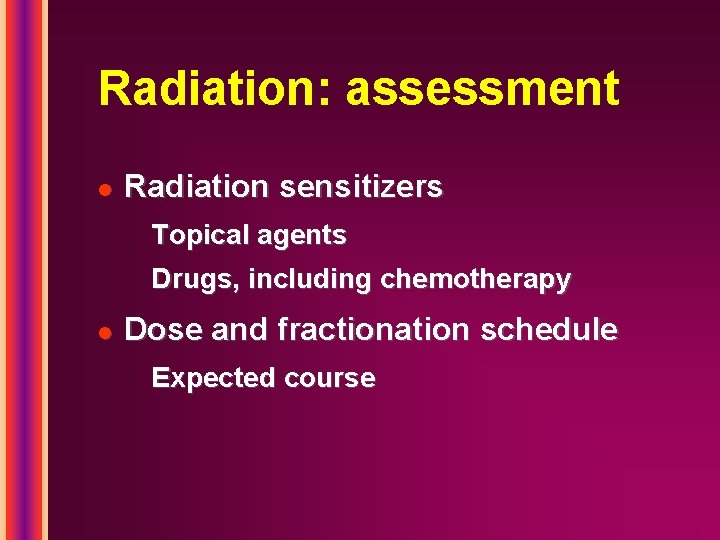
Radiation: assessment l Radiation sensitizers Topical agents Drugs, including chemotherapy l Dose and fractionation schedule Expected course
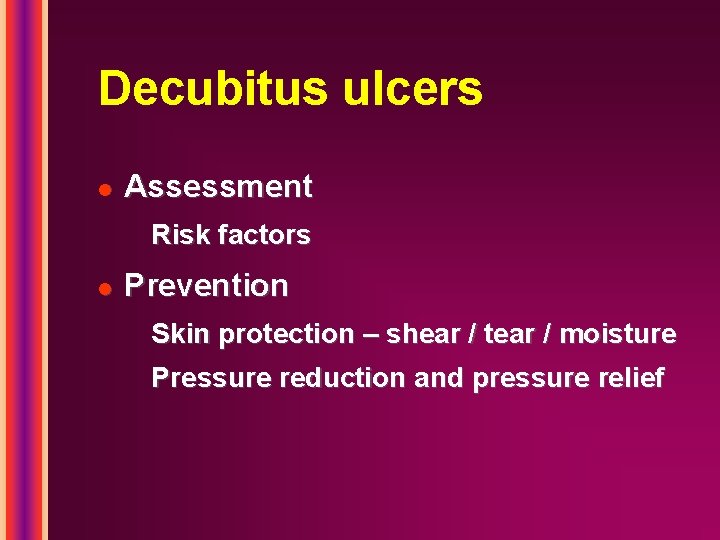
Decubitus ulcers l Assessment Risk factors l Prevention Skin protection – shear / tear / moisture Pressure reduction and pressure relief
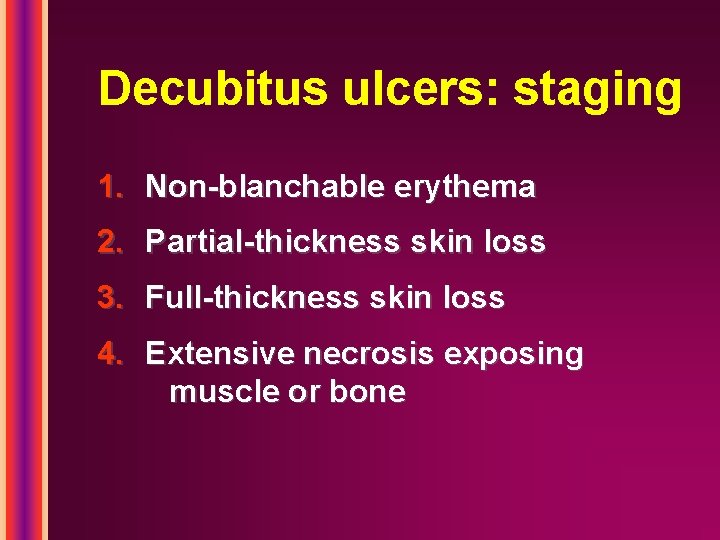
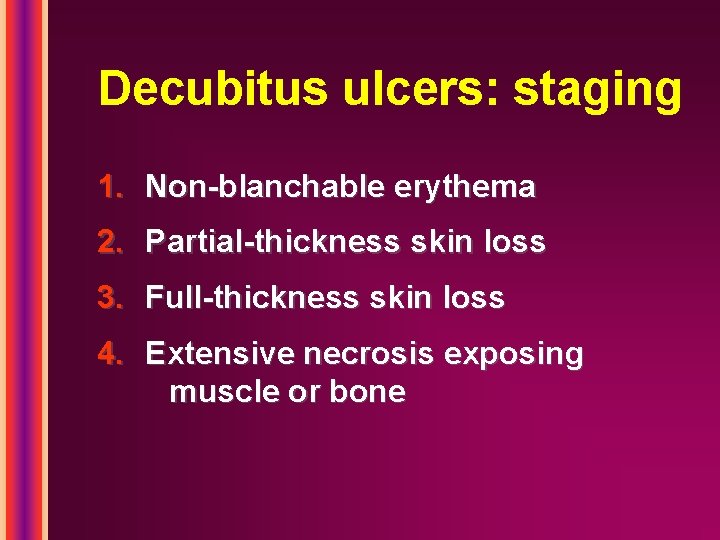
Decubitus ulcers: staging 1. Non-blanchable erythema 2. Partial-thickness skin loss 3. Full-thickness skin loss 4. Extensive necrosis exposing muscle or bone
Management l Acute versus chronic l By wound type

Necrotic wound: management l Debridement Surgical Enzymes and gels Mechanical Pain control l Cleansing
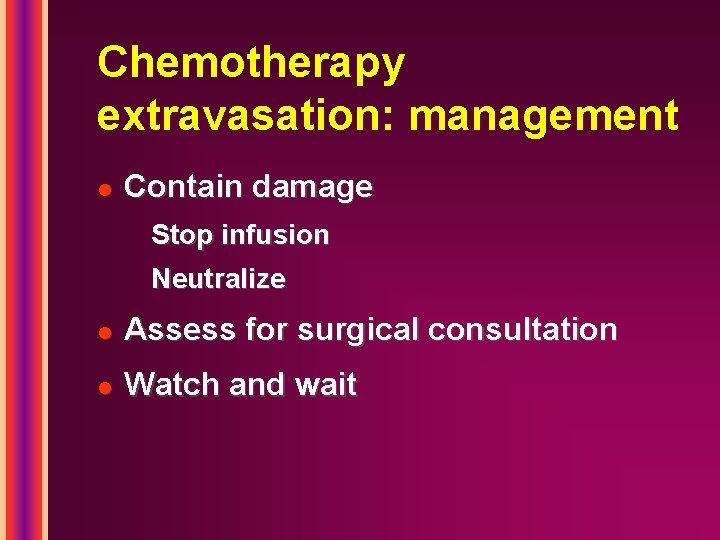
Chemotherapy extravasation: management l Contain damage Stop infusion Neutralize l Assess for surgical consultation l Watch and wait

Radiation: management l Promote healing Avoid cytotoxic agents Moist environment Treat infection Pain control
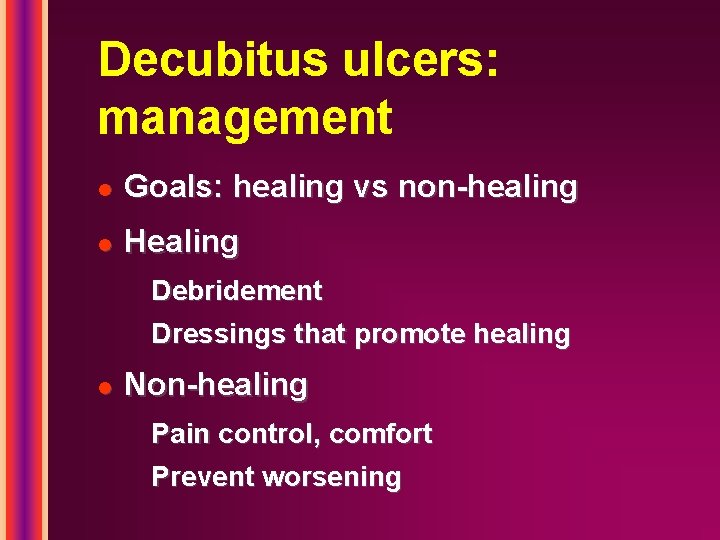
Decubitus ulcers: management l Goals: healing vs non-healing l Healing Debridement Dressings that promote healing l Non-healing Pain control, comfort Prevent worsening
Decubitus ulcers: dressing l Moist, interactive environment l Control infection l 6 types of dressing Foams Alginates Hydrogels Hydrocolloids Thin films Cotton gauze

Malignant wounds: management l Healing vs non-healing l Infections l Odors l Pain l Exudate l Bleeding

Odors l Topical and / or systemic antibiotics Metronidazole Silver sulfadiazine l Kitty litter l Activated charcoal l Vinegar l Burning candles
E P E C O Summary Use comprehensive assessment and pathophysiology-based therapy to treat the cause and improve the cancer experience
 Epeco
Epeco Epeco
Epeco Epeco
Epeco Epeco
Epeco Epec palliative care
Epec palliative care Epeco
Epeco Epeco
Epeco Franciscan palliative care
Franciscan palliative care Difference between metoclopramide and domperidone
Difference between metoclopramide and domperidone Esasr
Esasr Rug adl
Rug adl Hospice satisfaction survey
Hospice satisfaction survey Principles of palliative care
Principles of palliative care Palliative care vs hospice care
Palliative care vs hospice care Palliative care in nepal
Palliative care in nepal Palliative performance scale
Palliative performance scale Palliative performance scale
Palliative performance scale Palliative care assistant
Palliative care assistant European certificate in essential palliative care
European certificate in essential palliative care Parallel planning palliative care
Parallel planning palliative care Adjuvant neoadjuvant palliative
Adjuvant neoadjuvant palliative Validazione pos
Validazione pos Sas assessment tool
Sas assessment tool Log80 ausl romagna
Log80 ausl romagna Pcqc registry
Pcqc registry