The Culture of Health Care Ethics and Professionalism

- Slides: 25

The Culture of Health Care Ethics and Professionalism Lecture a This material (Comp 2 Unit 8) was developed by Oregon Health & Science University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU 24 OC 000015. This material was updated in 2016 by Bellevue College under Award Number 90 WT 0002. This work is licensed under the Creative Commons Attribution-Non. Commercial-Share. Alike 4. 0 International License. To view a copy of this license, visit http: //creativecommons. org/licenses/by-nc-sa/4. 0/.
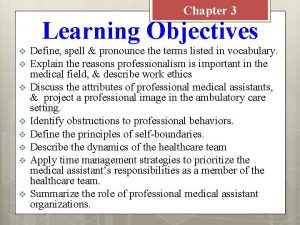
Ethics and Professionalism Learning Objectives • Discuss foundational concepts in medical ethics and professionalism (Lecture a). • Examine the relationships among ethical ideals, professionalism, and legal duties (Lecture a, b). • Apply the general principles of ethics and professionalism to specific topics (Lecture c, d). • Examine ethical issues in health informatics (Lecture d). 3
What Is Meant by Ethics and Professionalism? • Ethics is the study of what people think is right and wrong • Professionalism means that a person acts in a way that meets the standards of his or her profession – Training and skills – Ethical principles 4
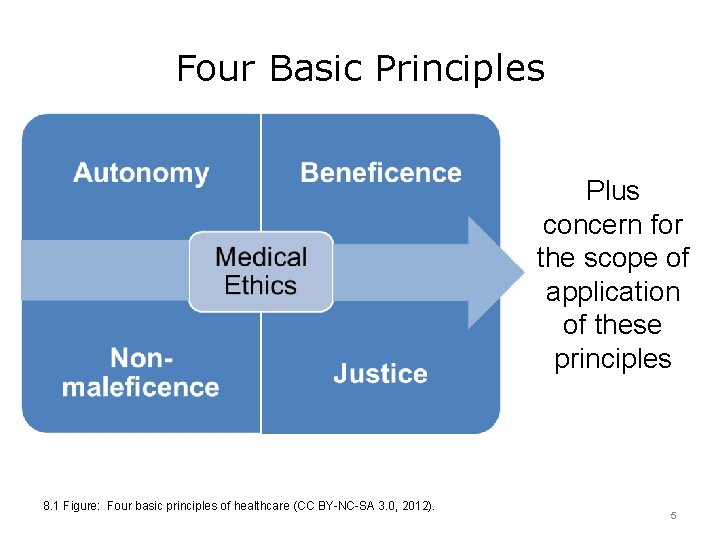
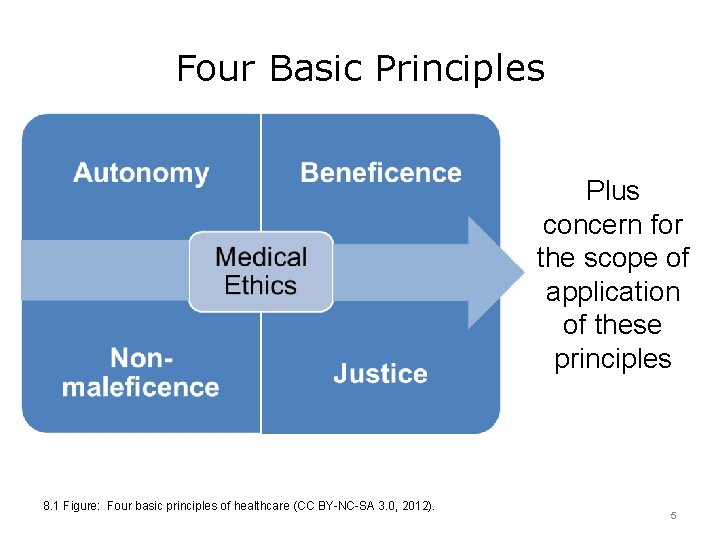
Four Basic Principles Plus concern for the scope of application of these principles 8. 1 Figure: Four basic principles of healthcare (CC BY-NC-SA 3. 0, 2012). 5
Respect for Autonomy • Autonomy = Self-governance • Respect for autonomy = Patients have the right to make their own decisions without undue influence – Health care decisions are voluntary • Foundation of “informed consent” 6
Beneficence • The idea that actions of health care providers should benefit people – Prevent problems that may occur – Treat problems that have occurred • Widely accepted as an appropriate goal of health care • Applied at individual level and populationwide level 7
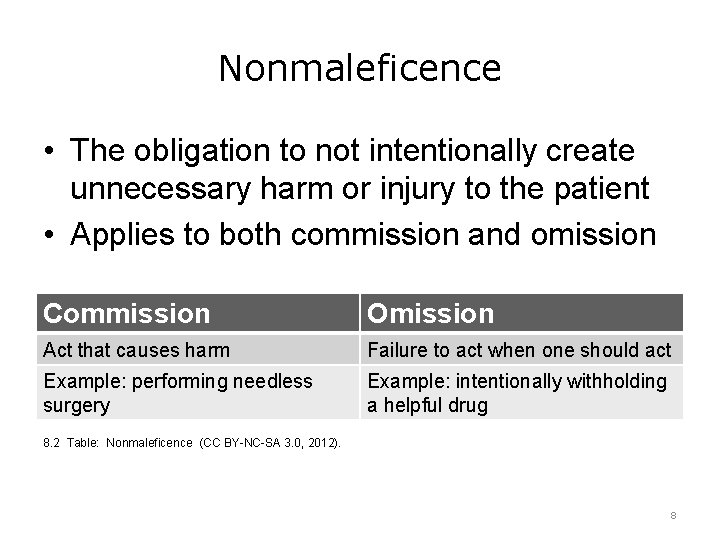
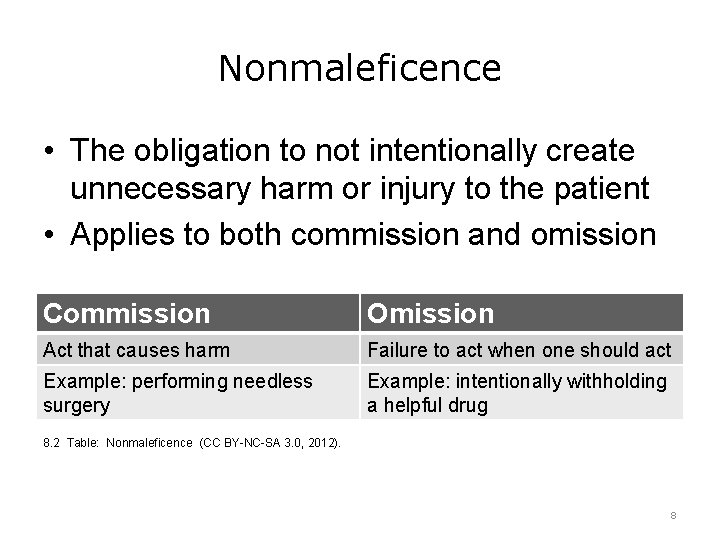
Nonmaleficence • The obligation to not intentionally create unnecessary harm or injury to the patient • Applies to both commission and omission Commission Omission Act that causes harm Failure to act when one should act Example: performing needless surgery Example: intentionally withholding a helpful drug 8. 2 Table: Nonmaleficence (CC BY-NC-SA 3. 0, 2012). 8
Justice • Justice in the medical ethics setting means fairness • Includes the concepts that – All people have the right to be treated equally – If there is not enough to go around, what is available should be distributed fairly 9
“Concern for the Scope of Their Action” • Who are health care professionals responsible to? – Everyone in their community? – Everyone in the country? • How far does respect for autonomy go? – Do animals have rights? – Does the environment have rights? 10
The Principles in Action • Respect for autonomy – Informed consent – Medical confidentiality • Beneficence and nonmaleficence – Requires that treatments be designed to maximize benefits and minimize risks • Justice – The risks of medical research should not fall disproportionally on one group of people 11
Prima facie Duties • Prima facie = “At first view, ” or self-evident • Each ethical principle is binding unless it conflicts with another principle • When the principles conflict, a person must decide which one to act on • The theory of the four principles does not give guidance about which one to choose or how to prioritize them 12
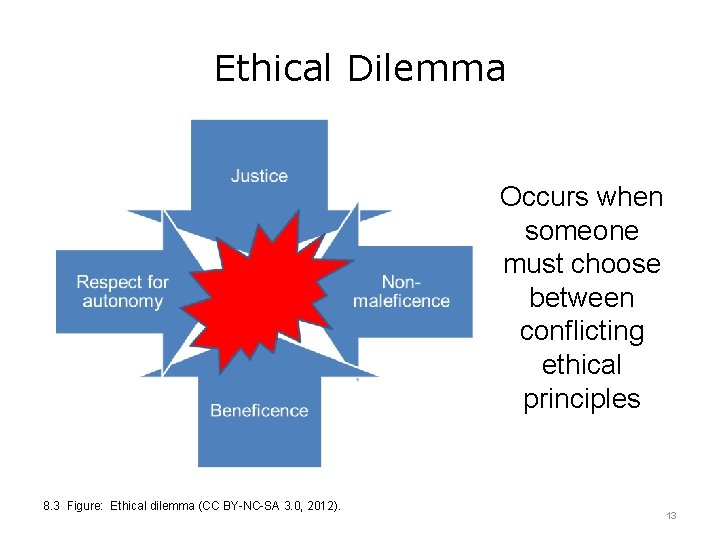
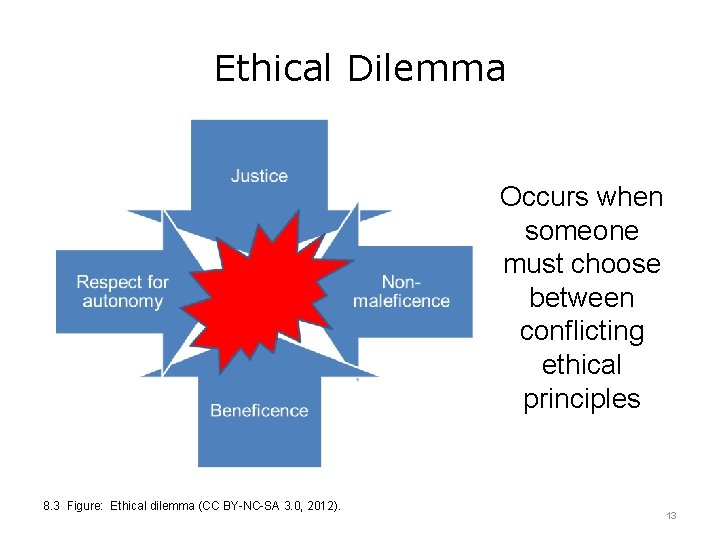
Ethical Dilemma Occurs when someone must choose between conflicting ethical principles 8. 3 Figure: Ethical dilemma (CC BY-NC-SA 3. 0, 2012). 13
Obligation and Aspiration • Obligation = Minimum standard necessary to meet professional obligation – Provide competent medical care to individual patients – Make sure patients understand the risks and benefits of treatment • Aspiration = Standard that one should strive to achieve but is not always attainable – Providing equal worldwide access to health care – Find cures for currently incurable conditions 14
Ethics Committee • Group of people who meet to discuss ethical dilemmas • All accredited hospitals must have a process for resolving ethical questions • Membership is usually diverse and may include – Doctors and nurses – Other health care professionals – Social workers and lawyers – Religious professionals – Members of the community 15
Codes of Ethics • Examples: – American Medical Association – American Nursing Association – International Council of Nurses – American Health Information Management Association – American Medical Informatics Association 16
Hippocratic Oath • Historical foundation of medical ethics • States a moral obligation to maximize benefits of treatment and minimize harms of treatment • Much of the original oath is not relevant today • Modernized versions of the oath are used at some, but not all, medical schools 17
Professionalism • Profession = An occupation that – Requires special knowledge and training – Has standards for behavior • Health care professional = A person who, by training and experience, has the knowledge to provide some aspect of health care delivery • Professionalism means – Acting in a way that meets standards – Knowing ethical obligations and trying to meet them 18
Core Medical Professional Responsibilities • • • Professional competence Honesty with patients Patient confidentiality Appropriate relations with patients Improving quality of care American Board of Internal Medicine, 2005; Cassel, 2009 19
Core Medical Professional Responsibilities Continued • • • Improving access to care Fair distribution of limited resources Scientific knowledge Managing conflicts of interest Maintaining professional responsibilities American Board of Internal Medicine, 2005; Cassel, 2009 20
Ethics and Professionalism Summary – Lecture a • People in the health care profession have duties based in the four core principles of medical ethics: – Respect for autonomy – Beneficence – Nonmaleficence – Justice • Health care professionals must consider how broadly their ethical duties extend (“scope of their action”) • Professionalism requires that people in the health care industry act in accord with certain standards 21
Ethics and Professionalism References – Lecture a References American Board of Internal Medicine. (2005). Physician charter. Retrieved from http: //abimfoundation. org/what-we-do/medical-professionalism-and-the-physiciancharter/physician-charter Antiel, R. M. , Kinghorn, W. A. , & Reed, D. A. (2013, July). Professionalism: Etiquette or habitus? . In Mayo Clinic Proceedings, 88 (7), 651. Mayo Foundation for Medical Education and Research. Aulisio, M. P, Arnold R. M. (2008). Helping to address value conflicts or uncertainties: Role of the ethics committee. Chest, 134, 417– 424. Cassel, C. K. (2009). 21 st century medical professionalism: Renewing the social contract. Retrieved from http: //www. slideshare. net/ABIMFoundation/medical-professinalism-renewing-social-contract CMPA, (2012) Physician professionalism. Is it still relevant? Retrieved from https: //www. cmpaacpm. ca/-/physician-professionalism-is-it-still-relevant. Ethics & Compliance Initiative. (n. d. ). Ethics and compliance glossary. Retrieved from https: //www. ethics. org/resources/free-toolkit/toolkit-glossary. Gholami-Kordkheili, F. , Wild, V. , & Strech, D. (2013). The impact of social media on medical professionalism: A systematic qualitative review of challenges and opportunities. Journal of Medical Internet Research, 15(8), e 184. Retrieved from http: //www. jmir. org/2013/8/e 184/%23 ref 44 Gillon R. (1994). Medical ethics: Four principles plus attention to scope. BMJ, 309(6948), 184– 188. Gillon R. (2003). Ethics needs principles: Four can encompass the rest—and respect for autonomy should be “first among equals. ” Journal of Medical Ethics, 29(5), 307– 312. 22
Ethics and Professionalism References – Lecture a Continued Jennings, B. , Baily, M. A. , Bottrell, M. , Lynn, J. (Eds. ). (2007). Health care quality improvement: Ethical and regulatory issues. The Hastings Center. Retrieved from http: //www. thehastingscenter. org/uploaded. Files/Publications/Special_Reports/Health%20 Care%2 0 Quality%20 Improvement. pdf Kirk, L. M. (2007). Professionalism in medicine: definitions and considerations for teaching. Proceedings (Baylor University Medical Center), 20, 13– 16. Kong, W. M. (2015). What is good medical ethics? A clinician's perspective. Journal of Medical Ethics, 41(1), 79– 82. Retrieved from http: //jme. bmj. com/content/41/1/79. full Mc. Cormick, T. R. (2013). Ethics in medicine: Principles of bioethics. Seattle: University of Washington School of Medicine. Retrieved from http: //depts. washington. edu/bioethx/tools/princpl. html Meslin, E. M. , Alpert, S. A. , Carroll, A. E. , Odell, J. D. , Tierney, W. M. , & Schwartz, P. H. (2013). Giving patients granular control of personal health information: Using an ethics “Points to Consider” to informatics system designers. International Journal of Medical Informatics, 82(12), 1136– 1143. Retrieved from http: //www. sciencedirect. com/science/article/pii/S 1386505613001895 National Library of Medicine, History of Medicine Division. (2002). Greek medicine: The Hippocratic oath. Retrieved from http: //www. nlm. nih. gov/hmd/greek_oath. html Pearlman, R. A. (2013). Ethics in medicine: Ethics committees and ethics consultation. University of Washington School of Medicine. Retrieved from http: //depts. washington. edu/bioethx/topics/ethics. html 23
Ethics and Professionalism References – Lecture a Continued 2 Wynia, M. K. , Papadakis, M. A. , Sullivan, W. M. , & Hafferty, F. W. (2014). More than a list of values and desired behaviors: A foundational understanding of medical professionalism. Academic Medicine, 89(5), 712– 714. Tables, Charts, Figures 8. 1 Figure: Four basic principles of healthcare (CC BY-NC-SA 3. 0, 2012). 8. 2 Table: Non-Maleficence (CC BY-NC-SA 3. 0, 2012). 8. 3 Figure: Ethical dilemma (CC BY-NC-SA 3. 0, 2012). 24
The Culture of Health Care Ethics and Professionalism Lecture a This material was developed by Oregon Health & Science University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU 24 OC 000015. This material was updated in 2016 by Bellevue College under Award Number 90 WT 0002. 25
 Health and social component 3
Health and social component 3 Care value base health and social care
Care value base health and social care Primary secondary tertiary care definition
Primary secondary tertiary care definition Ac 61-98 plan of action
Ac 61-98 plan of action Professionalism and integrity
Professionalism and integrity Integrity and professionalism
Integrity and professionalism Compare micro-ethics and macro-ethics.
Compare micro-ethics and macro-ethics. Business communication chapter 2
Business communication chapter 2 Popular culture examples
Popular culture examples Continuous culture and batch culture
Continuous culture and batch culture American vs indian culture
American vs indian culture Uses of selenite f broth
Uses of selenite f broth Folk culture and popular culture venn diagram
Folk culture and popular culture venn diagram Popular culture examples
Popular culture examples Indole test
Indole test Folk culture and popular culture venn diagram
Folk culture and popular culture venn diagram Anaerobic culture method
Anaerobic culture method Describe lawn culture and surface plating
Describe lawn culture and surface plating Surface culture deep culture and esol
Surface culture deep culture and esol No professionalism
No professionalism Domain 4: professional responsibilities examples
Domain 4: professional responsibilities examples Professionalism workshop
Professionalism workshop What are the 3 key elements of professionalism
What are the 3 key elements of professionalism Having a courteous conscientious and respectful approach
Having a courteous conscientious and respectful approach Professionalism skills for workplace success
Professionalism skills for workplace success Professionalism definition
Professionalism definition