PHARMACOLOGY PHL 313 Chapter 8 Muscles Relaxants Skeletal

- Slides: 21

PHARMACOLOGY PHL 313 Chapter 8 Muscles Relaxants
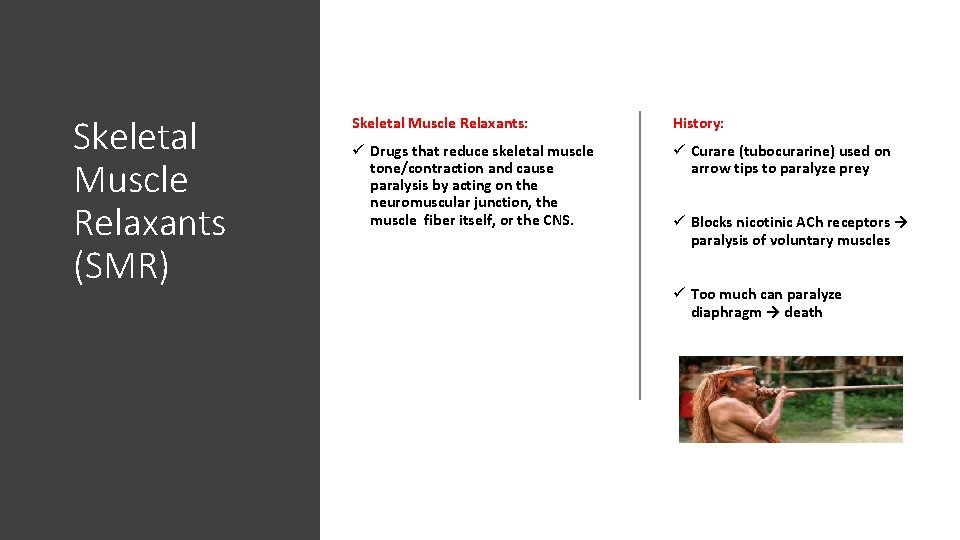
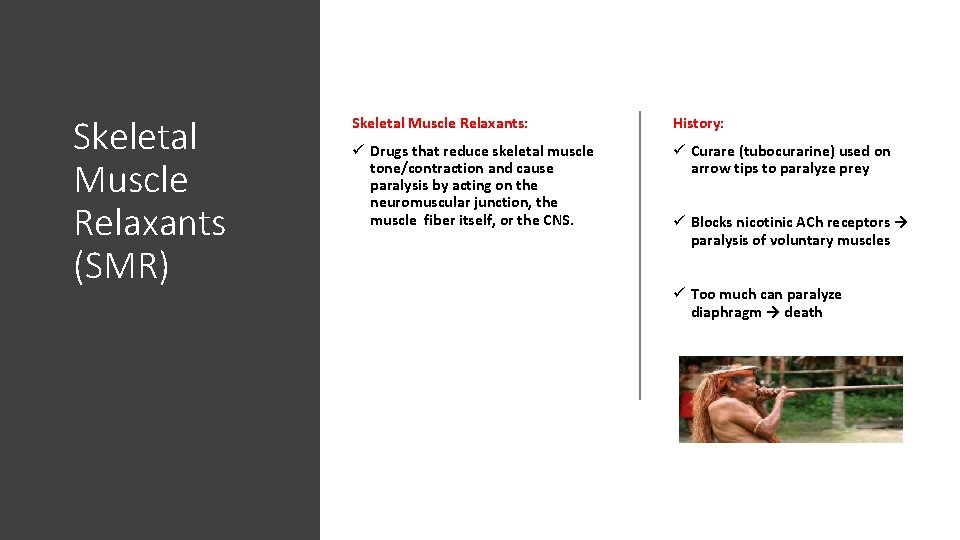
Skeletal Muscle Relaxants (SMR) Skeletal Muscle Relaxants: History: ü Drugs that reduce skeletal muscle tone/contraction and cause paralysis by acting on the neuromuscular junction, the muscle fiber itself, or the CNS. ü Curare (tubocurarine) used on arrow tips to paralyze prey ü Blocks nicotinic ACh receptors → paralysis of voluntary muscles ü Too much can paralyze diaphragm → death
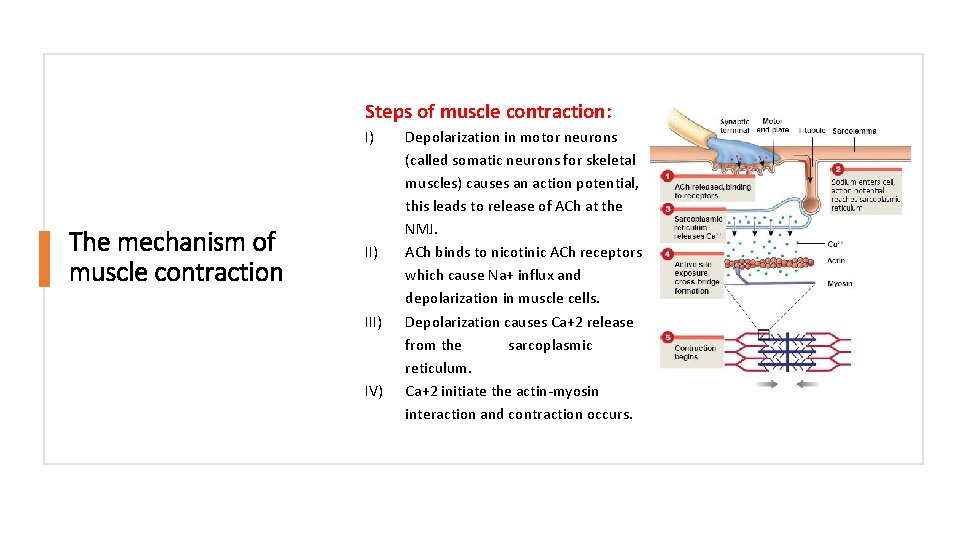
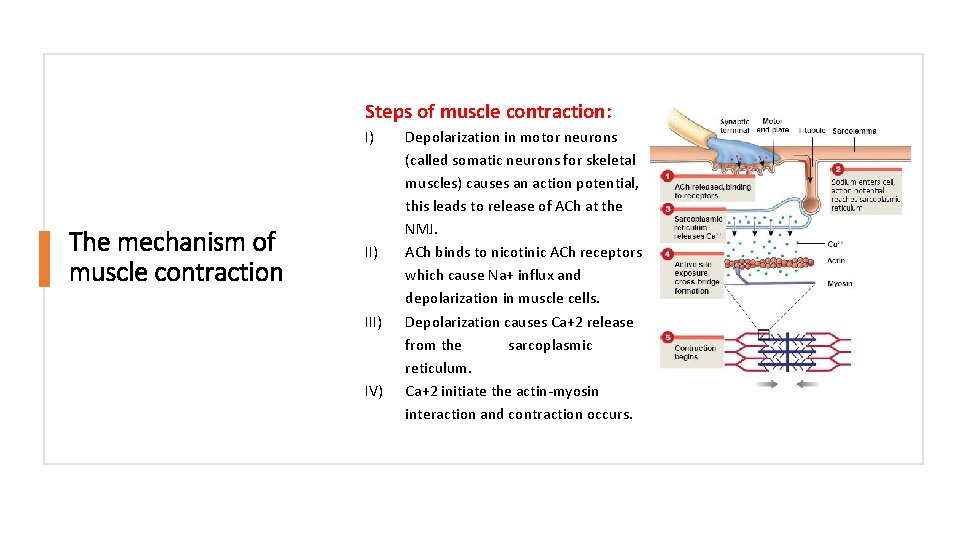
Steps of muscle contraction: I) The mechanism of muscle contraction II) IV) Depolarization in motor neurons (called somatic neurons for skeletal muscles) causes an action potential, this leads to release of ACh at the NMJ. ACh binds to nicotinic ACh receptors which cause Na+ influx and depolarization in muscle cells. Depolarization causes Ca+2 release from the sarcoplasmic reticulum. Ca+2 initiate the actin-myosin interaction and contraction occurs.
Uses of Skeletal Muscle Relaxants (SMR) Used in: A- To facilitate surgery: C- Ocular surgery: ü Mechanical ventilation ü Competitive blockers to paralyze extraocular muscles ü Relax body parts for surgery (chest, abdomen. . . etc) B- Treat spastic conditions ü Associated with neurodegenerative disorders (e. g. MS, Parkinson’s…etc) ü Status epilepticus ü Sport injuries
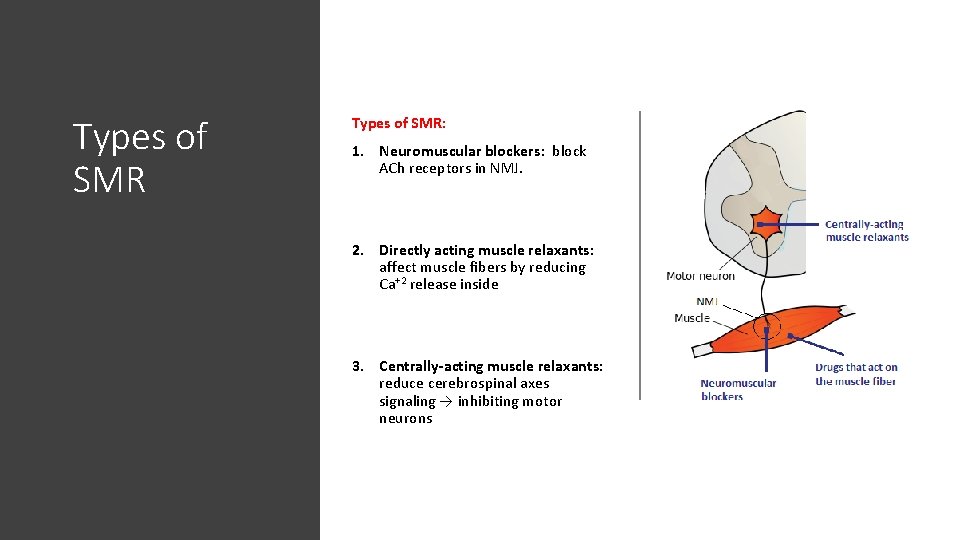
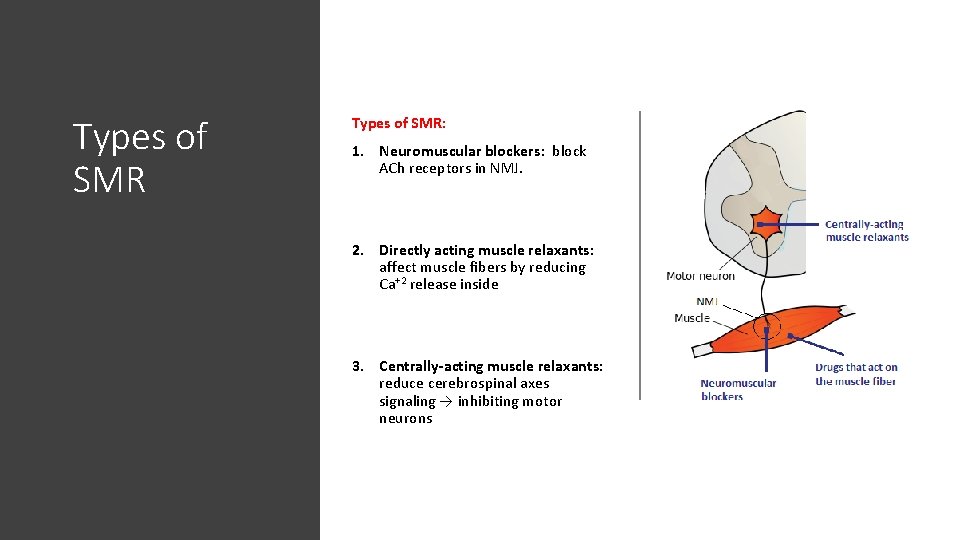
Types of SMR: 1. Neuromuscular blockers: block ACh receptors in NMJ. 2. Directly acting muscle relaxants: affect muscle fibers by reducing Ca+2 release inside 3. Centrally-acting muscle relaxants: reduce cerebrospinal axes signaling → inhibiting motor neurons .
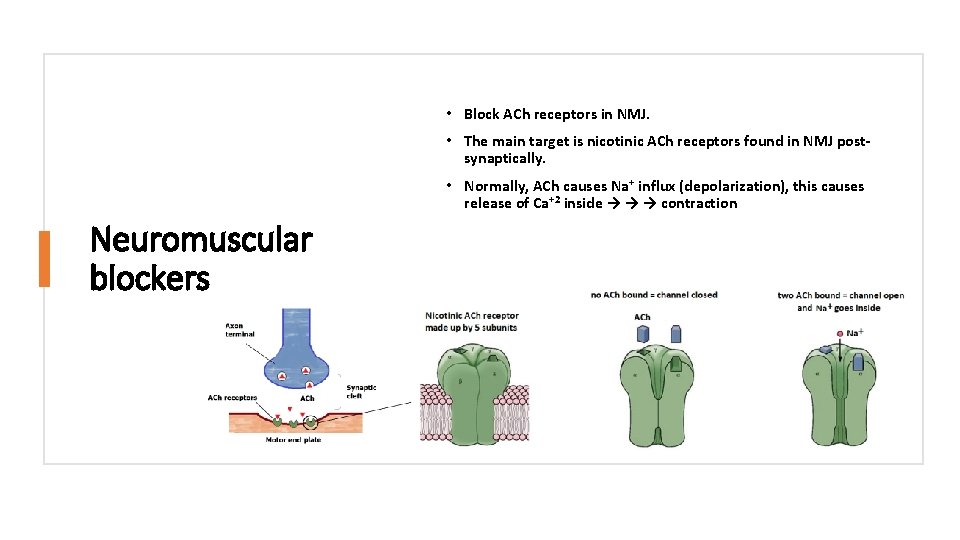
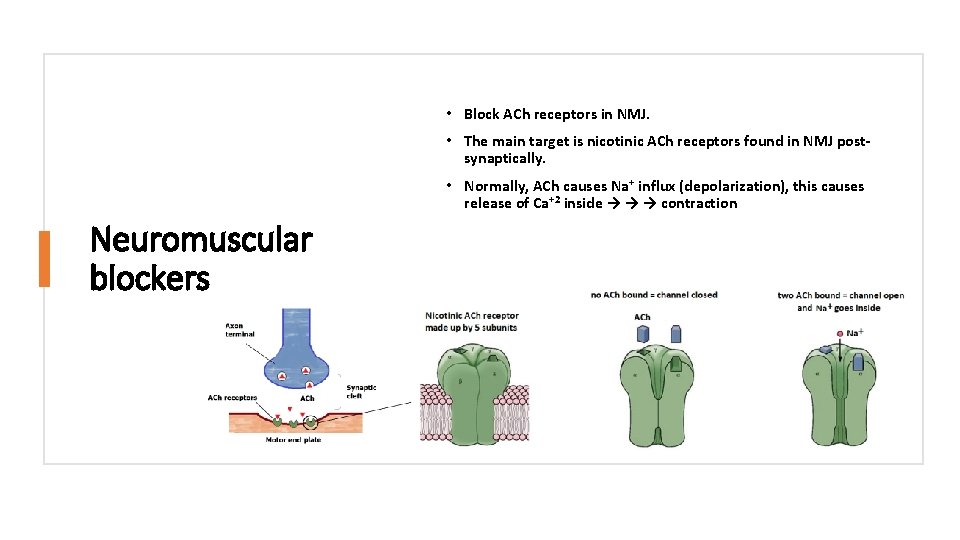
• Block ACh receptors in NMJ. • The main target is nicotinic ACh receptors found in NMJ postsynaptically. • Normally, ACh causes Na+ influx (depolarization), this causes release of Ca+2 inside → → → contraction Neuromuscular blockers
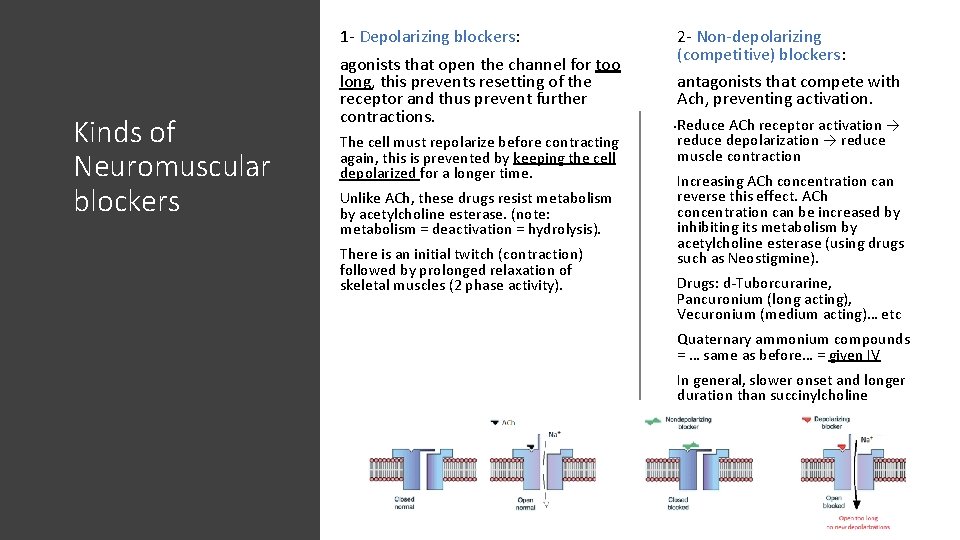
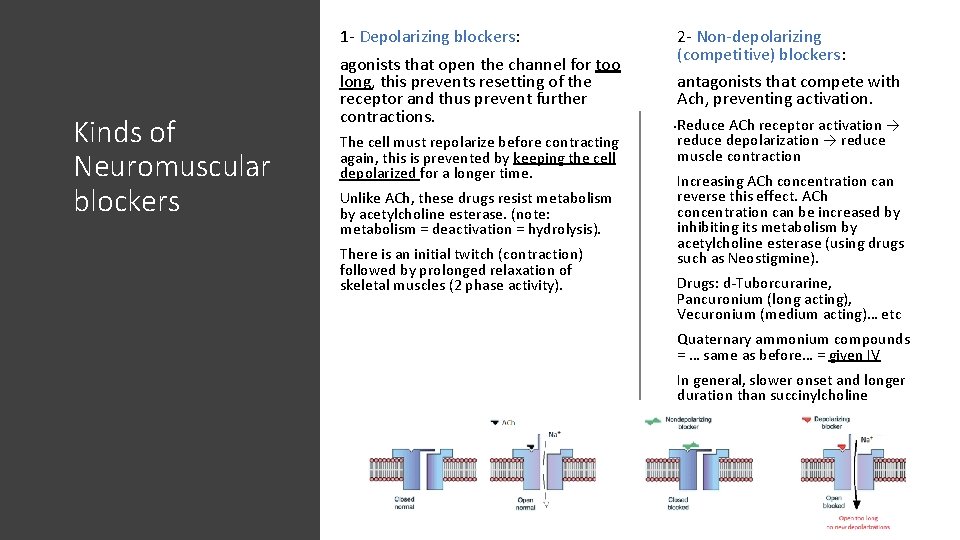
1 - Depolarizing blockers: Kinds of Neuromuscular blockers agonists that open the channel for too long, this prevents resetting of the receptor and thus prevent further contractions. The cell must repolarize before contracting again, this is prevented by keeping the cell depolarized for a longer time. Unlike ACh, these drugs resist metabolism by acetylcholine esterase. (note: metabolism = deactivation = hydrolysis). There is an initial twitch (contraction) followed by prolonged relaxation of skeletal muscles (2 phase activity). 2 - Non-depolarizing (competitive) blockers: antagonists that compete with Ach, preventing activation. . Reduce ACh receptor activation → reduce depolarization → reduce muscle contraction Increasing ACh concentration can reverse this effect. ACh concentration can be increased by inhibiting its metabolism by acetylcholine esterase (using drugs such as Neostigmine). Drugs: d-Tuborcurarine, Pancuronium (long acting), Vecuronium (medium acting)… etc Quaternary ammonium compounds = … same as before… = given IV In general, slower onset and longer duration than succinylcholine
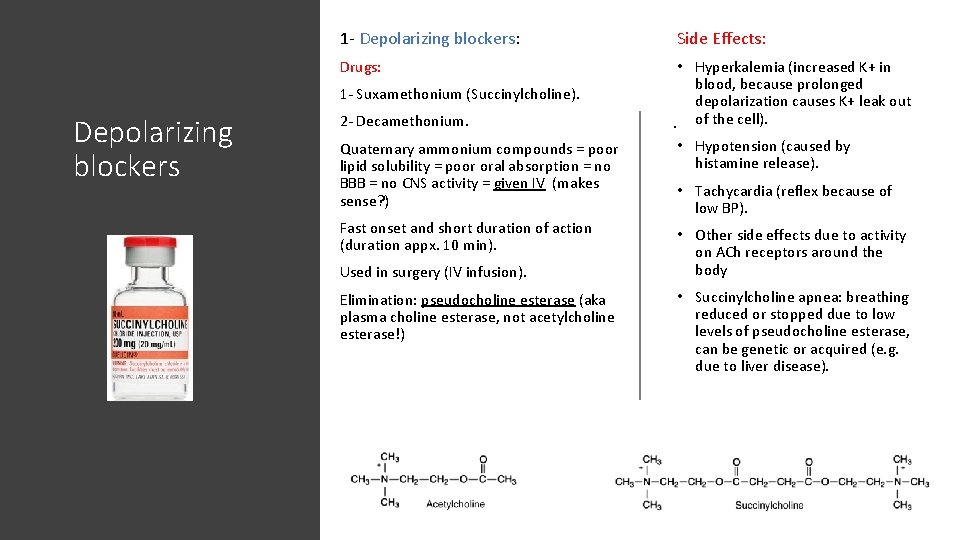
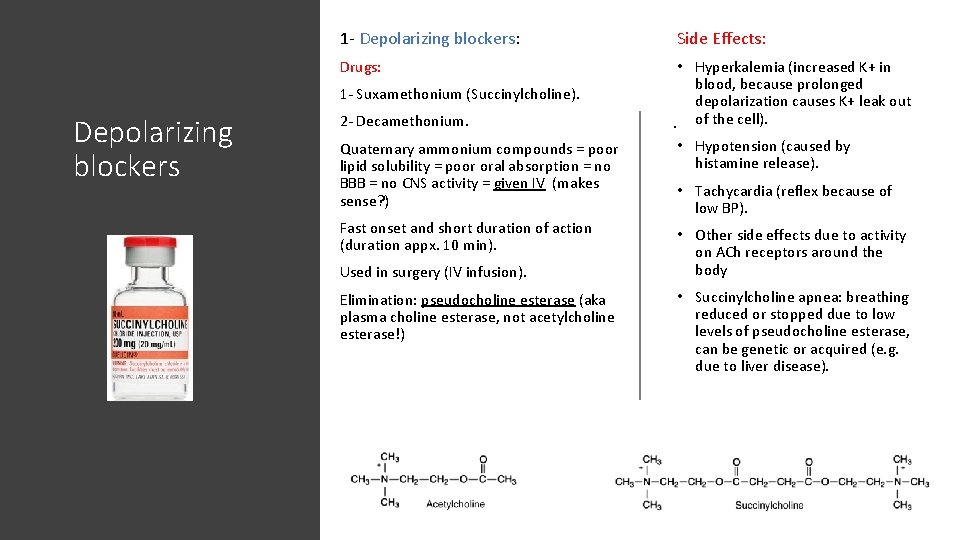
1 - Depolarizing blockers: Side Effects: Drugs: • Hyperkalemia (increased K+ in blood, because prolonged depolarization causes K+ leak out. of the cell). 1 - Suxamethonium (Succinylcholine). Depolarizing blockers 2 - Decamethonium. Quaternary ammonium compounds = poor lipid solubility = poor oral absorption = no BBB = no CNS activity = given IV (makes sense? ) • Hypotension (caused by histamine release). Fast onset and short duration of action (duration appx. 10 min). • Other side effects due to activity on ACh receptors around the body Used in surgery (IV infusion). Elimination: pseudocholine esterase (aka plasma choline esterase, not acetylcholine esterase!) • Tachycardia (reflex because of low BP). • Succinylcholine apnea: breathing reduced or stopped due to low levels of pseudocholine esterase, can be genetic or acquired (e. g. due to liver disease).
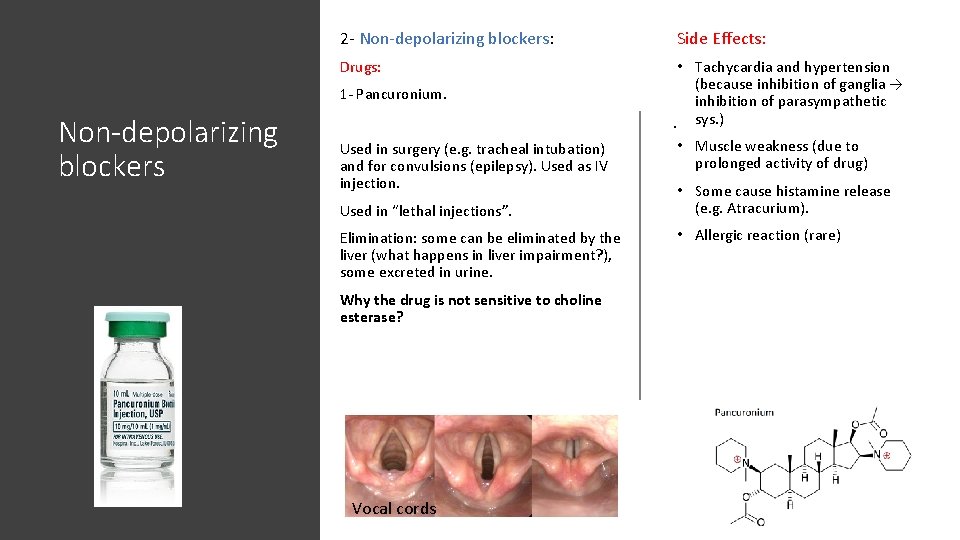
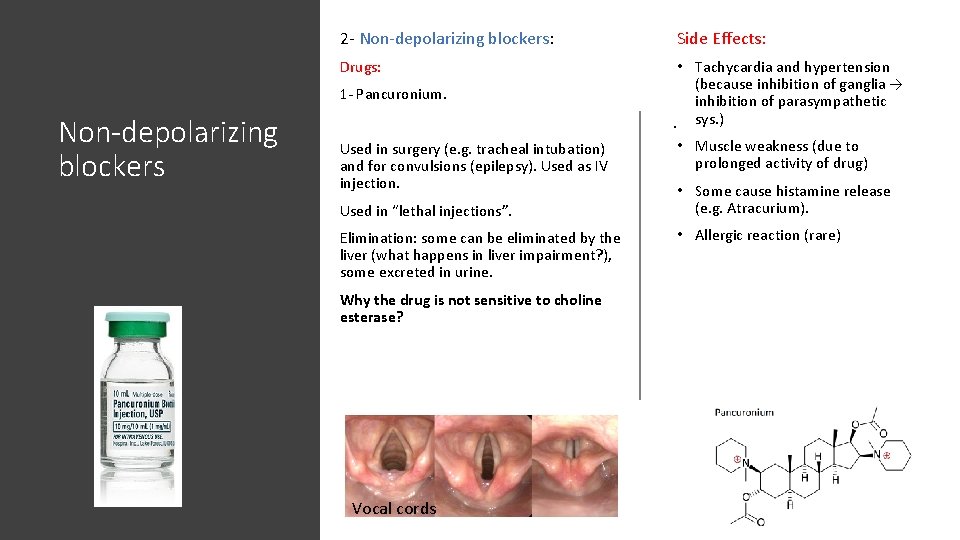
2 - Non-depolarizing blockers: Side Effects: Drugs: • Tachycardia and hypertension (because inhibition of ganglia → inhibition of parasympathetic. sys. ) 1 - Pancuronium. Non-depolarizing blockers Used in surgery (e. g. tracheal intubation) and for convulsions (epilepsy). Used as IV injection. Used in “lethal injections”. Elimination: some can be eliminated by the liver (what happens in liver impairment? ), some excreted in urine. Why the drug is not sensitive to choline esterase? Vocal cords • Muscle weakness (due to prolonged activity of drug) • Some cause histamine release (e. g. Atracurium). • Allergic reaction (rare)
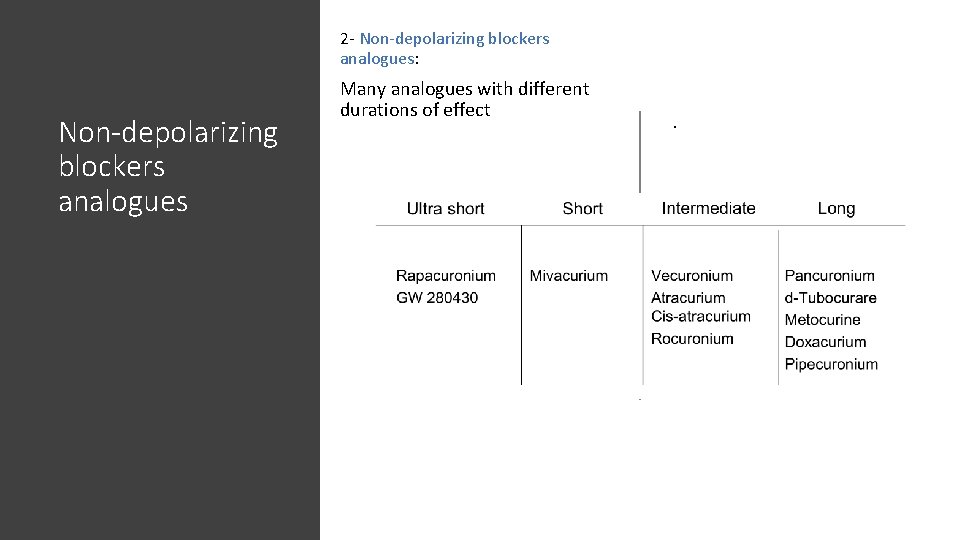
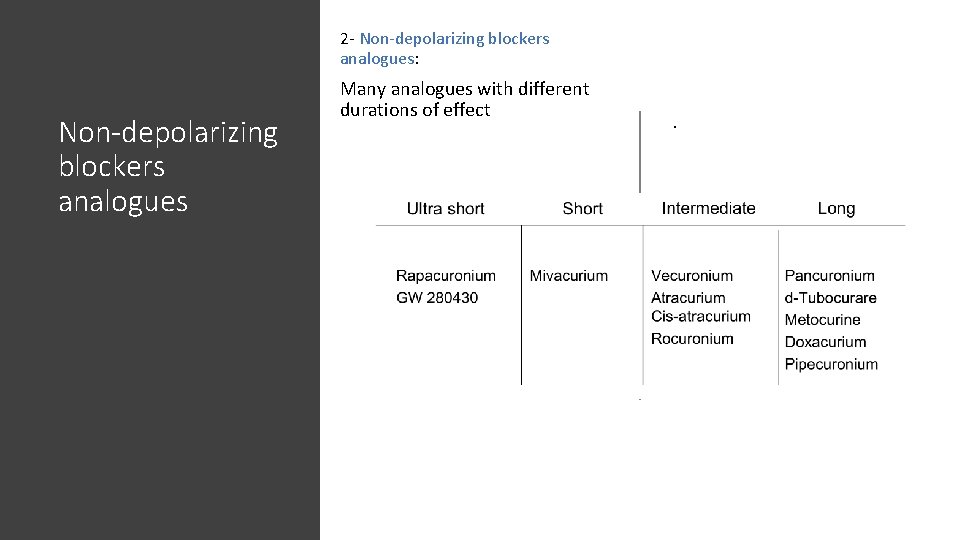
2 - Non-depolarizing blockers analogues: Non-depolarizing blockers analogues Many analogues with different durations of effect .
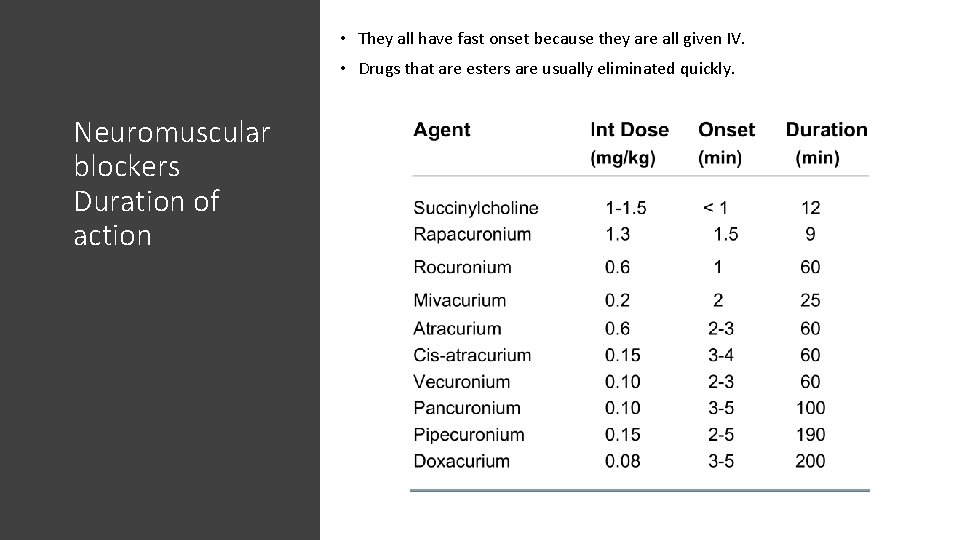
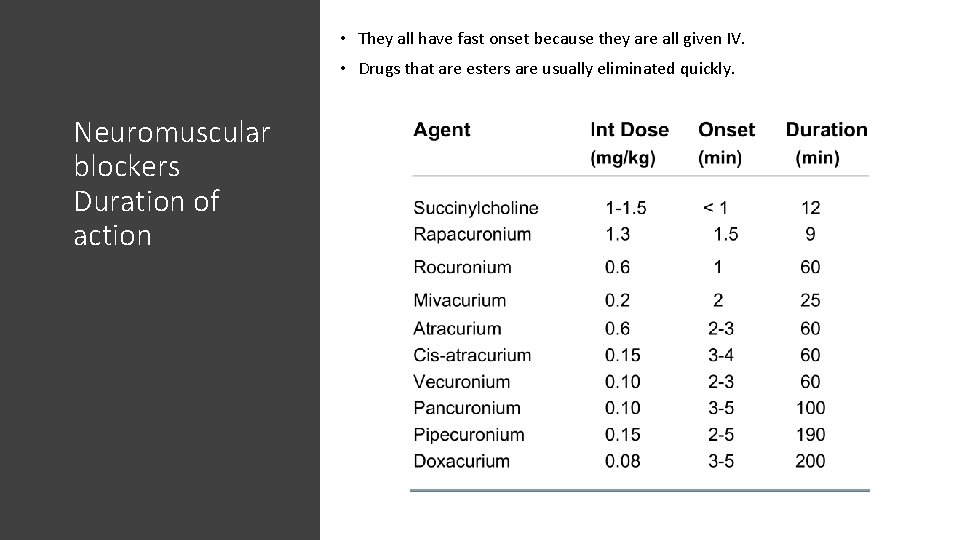
• They all have fast onset because they are all given IV. • Drugs that are esters are usually eliminated quickly. Neuromuscular blockers Duration of action .
Neuromuscular blockers interactions with other drugs In general, these are expected to interact with drugs that target ACh and its receptors. Such as acetylcholine esterase inhibitors (Neostigmine, Physostigmine… etc), causing a decreased blocking effect. They interact with: • With drugs that affect Ca+2 release (e. g. Verapamil) causing potentiation of effect. • With general anesthetics. • With drugs that affect cardiovascular system (heart rate, blood pressure). • With drugs that affect liver and renal function (e. g. ↓ liver metabolism = ↑ activity of Pancuronium). • With aminoglycosides (e. g. Streptomycin) because they reduce ACh release (causing potentiation).
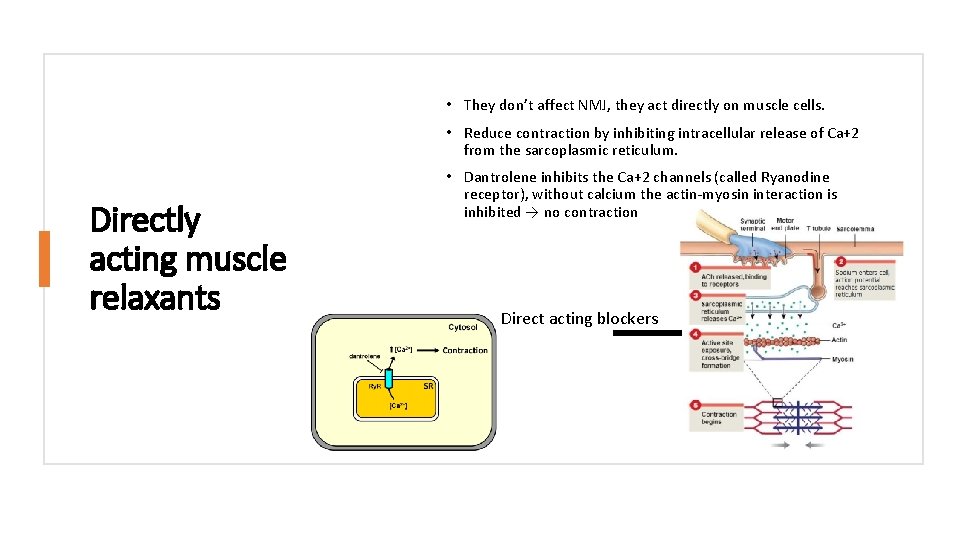
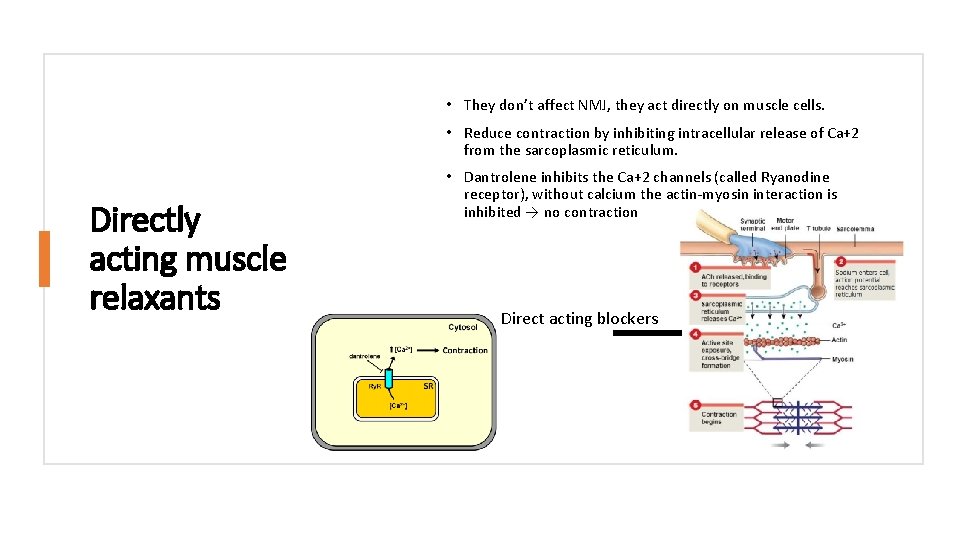
• They don’t affect NMJ, they act directly on muscle cells. • Reduce contraction by inhibiting intracellular release of Ca+2 from the sarcoplasmic reticulum. Directly acting muscle relaxants • Dantrolene inhibits the Ca+2 channels (called Ryanodine receptor), without calcium the actin-myosin interaction is inhibited → no contraction Direct acting blockers
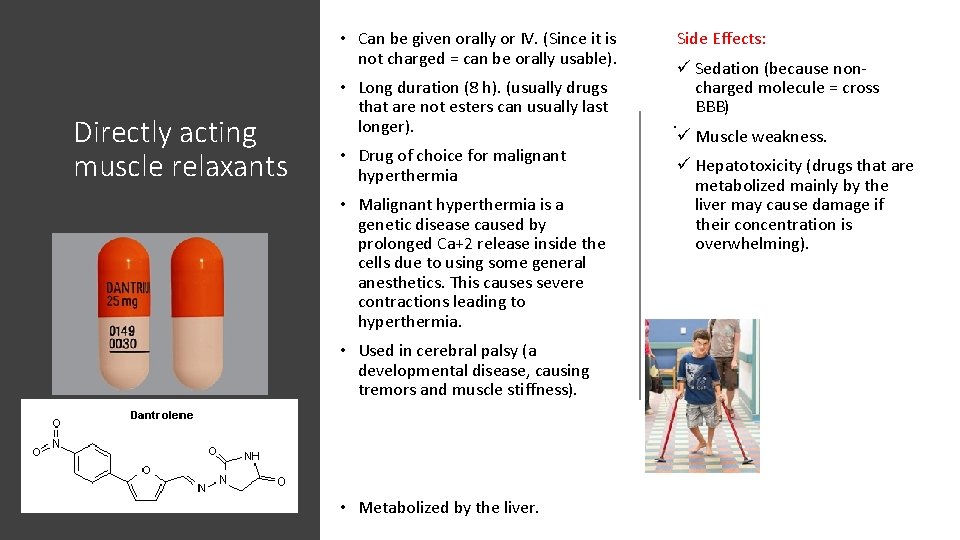
• Can be given orally or IV. (Since it is not charged = can be orally usable). Directly acting muscle relaxants • Long duration (8 h). (usually drugs that are not esters can usually last longer). • Drug of choice for malignant hyperthermia • Malignant hyperthermia is a genetic disease caused by prolonged Ca+2 release inside the cells due to using some general anesthetics. This causes severe contractions leading to hyperthermia. • Used in cerebral palsy (a developmental disease, causing tremors and muscle stiffness). • Metabolized by the liver. Side Effects: . ü Sedation (because noncharged molecule = cross BBB) ü Muscle weakness. ü Hepatotoxicity (drugs that are metabolized mainly by the liver may cause damage if their concentration is overwhelming).
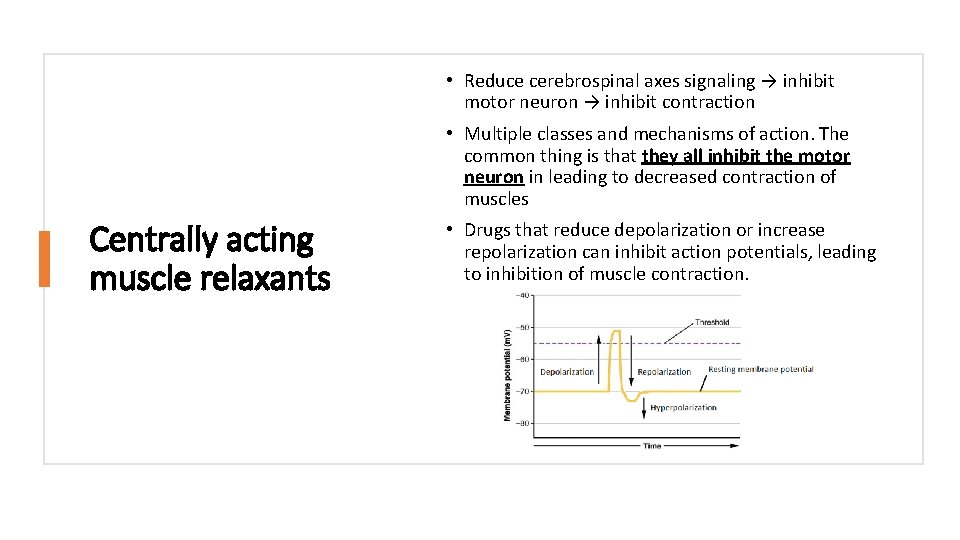
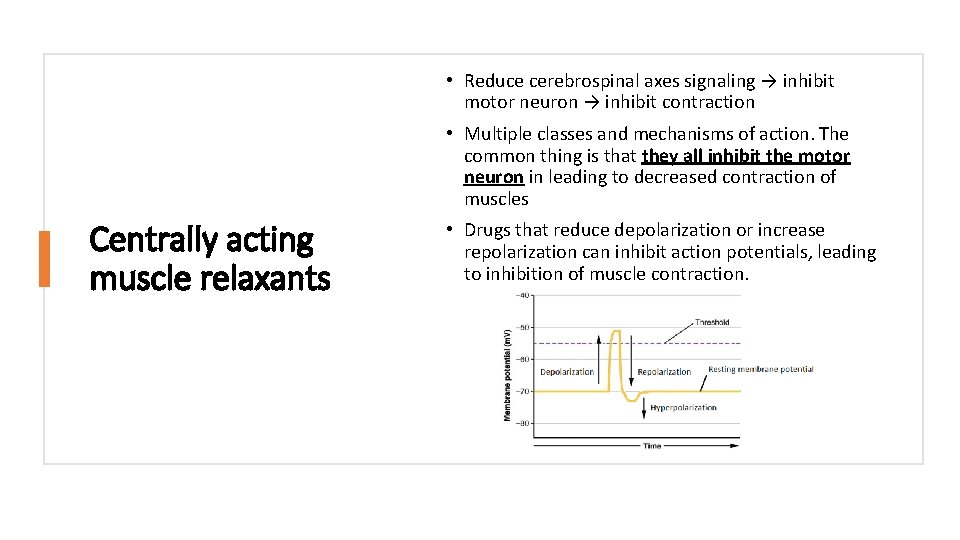
• Reduce cerebrospinal axes signaling → inhibit motor neuron → inhibit contraction • Multiple classes and mechanisms of action. The common thing is that they all inhibit the motor neuron in leading to decreased contraction of muscles Centrally acting muscle relaxants • Drugs that reduce depolarization or increase repolarization can inhibit action potentials, leading to inhibition of muscle contraction.
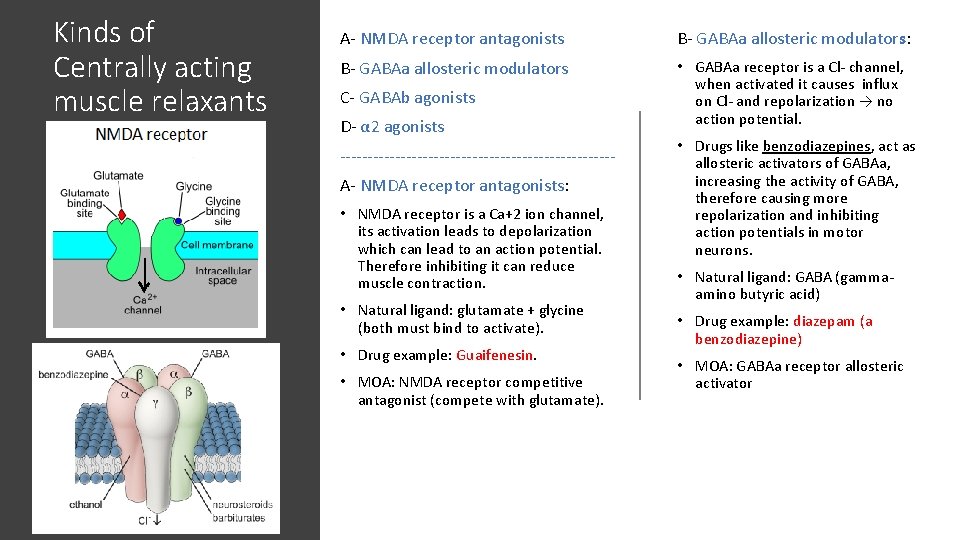
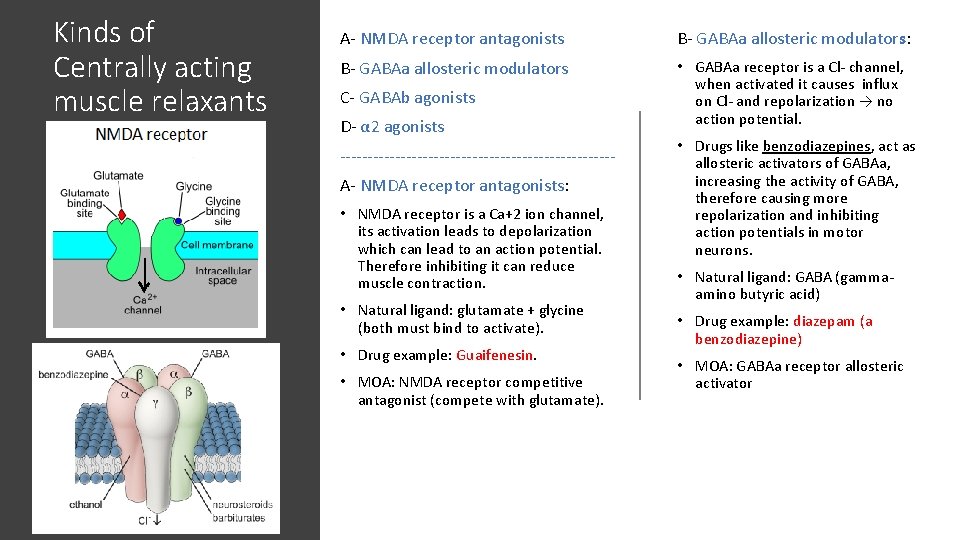
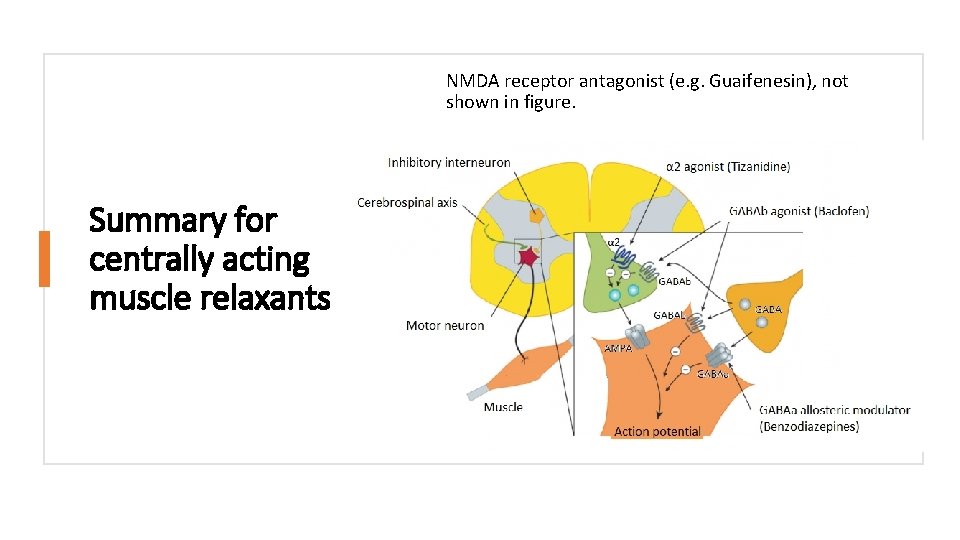
Kinds of Centrally acting muscle relaxants A- NMDA receptor antagonists B- GABAa allosteric modulators: B- GABAa allosteric modulators • GABAa receptor is a Cl- channel, when activated it causes influx on Cl- and repolarization → no action potential. C- GABAb agonists D- α 2 agonists -------------------------A- NMDA receptor antagonists: • NMDA receptor is a Ca+2 ion channel, its activation leads to depolarization which can lead to an action potential. Therefore inhibiting it can reduce muscle contraction. • Natural ligand: glutamate + glycine (both must bind to activate). • Drug example: Guaifenesin. • MOA: NMDA receptor competitive antagonist (compete with glutamate). • Drugs like benzodiazepines, act as allosteric activators of GABAa, increasing the activity of GABA, therefore causing more repolarization and inhibiting action potentials in motor neurons. • Natural ligand: GABA (gammaamino butyric acid) • Drug example: diazepam (a benzodiazepine) • MOA: GABAa receptor allosteric activator
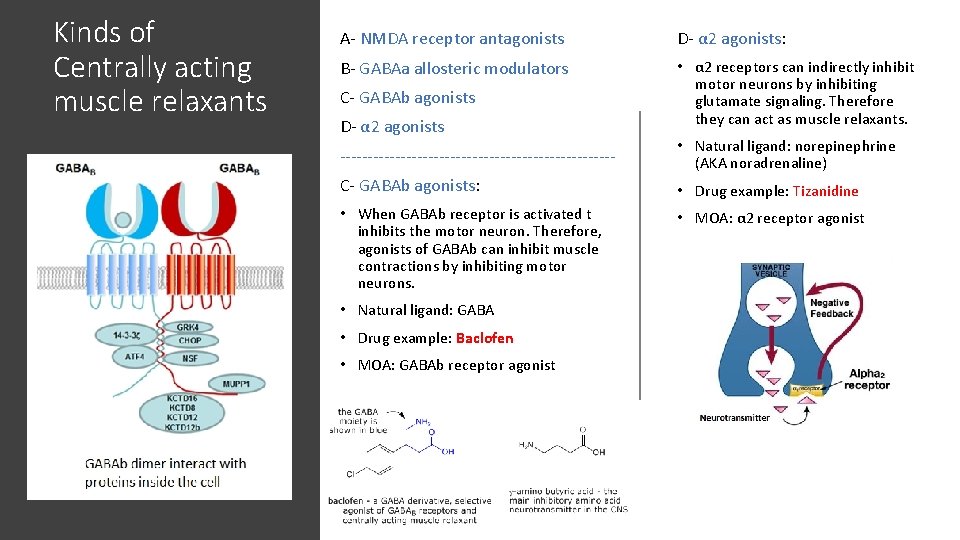
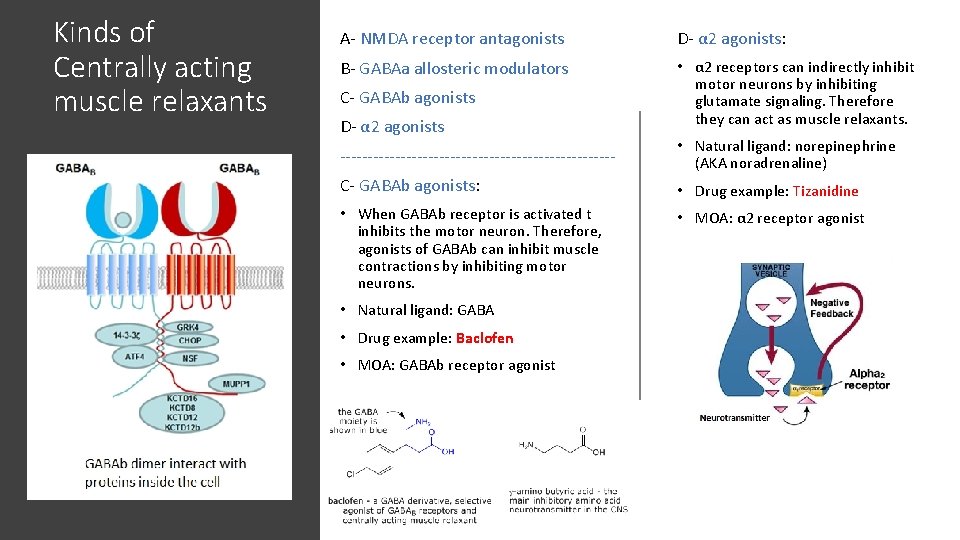
Kinds of Centrally acting muscle relaxants A- NMDA receptor antagonists D- α 2 agonists: B- GABAa allosteric modulators • α 2 receptors can indirectly inhibit motor neurons by inhibiting glutamate signaling. Therefore they can act as muscle relaxants. C- GABAb agonists D- α 2 agonists ------------------------- • Natural ligand: norepinephrine (AKA noradrenaline) C- GABAb agonists: • Drug example: Tizanidine • When GABAb receptor is activated t inhibits the motor neuron. Therefore, agonists of GABAb can inhibit muscle contractions by inhibiting motor neurons. • MOA: α 2 receptor agonist • Natural ligand: GABA • Drug example: Baclofen • MOA: GABAb receptor agonist
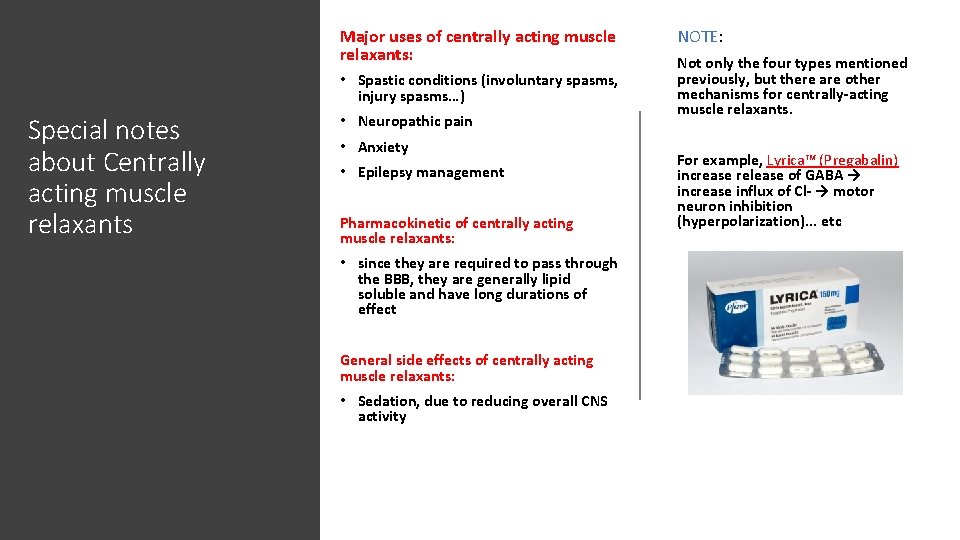
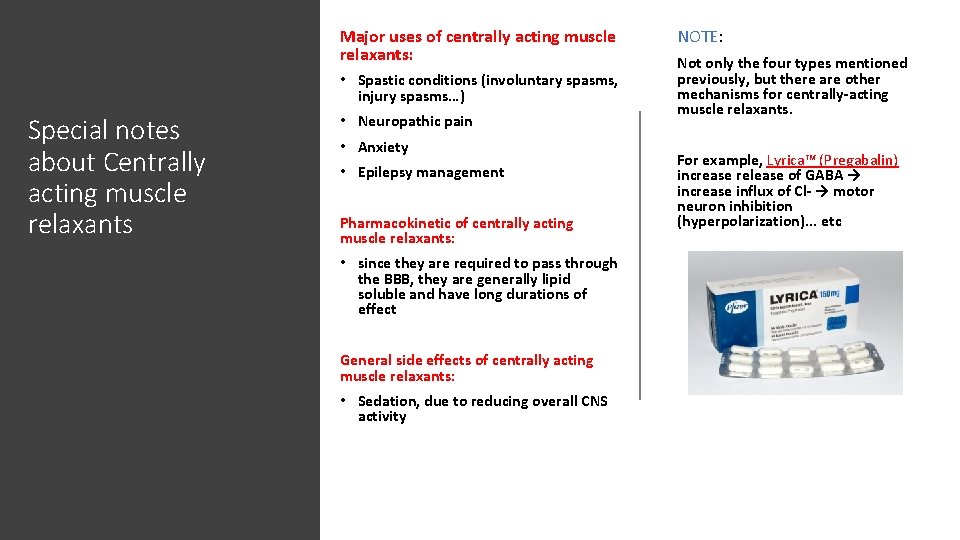
Major uses of centrally acting muscle relaxants: • Spastic conditions (involuntary spasms, injury spasms…) Special notes about Centrally acting muscle relaxants • Neuropathic pain • Anxiety • Epilepsy management Pharmacokinetic of centrally acting muscle relaxants: • since they are required to pass through the BBB, they are generally lipid soluble and have long durations of effect General side effects of centrally acting muscle relaxants: • Sedation, due to reducing overall CNS activity NOTE: Not only the four types mentioned previously, but there are other mechanisms for centrally-acting muscle relaxants. For example, Lyrica™ (Pregabalin) increase release of GABA → increase influx of Cl- → motor neuron inhibition (hyperpolarization). . . etc
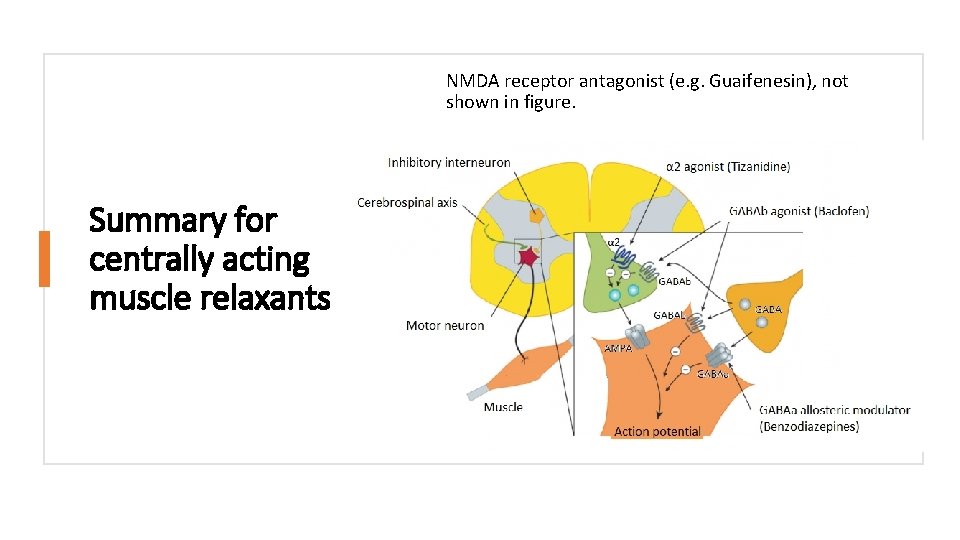
NMDA receptor antagonist (e. g. Guaifenesin), not shown in figure. Summary for centrally acting muscle relaxants
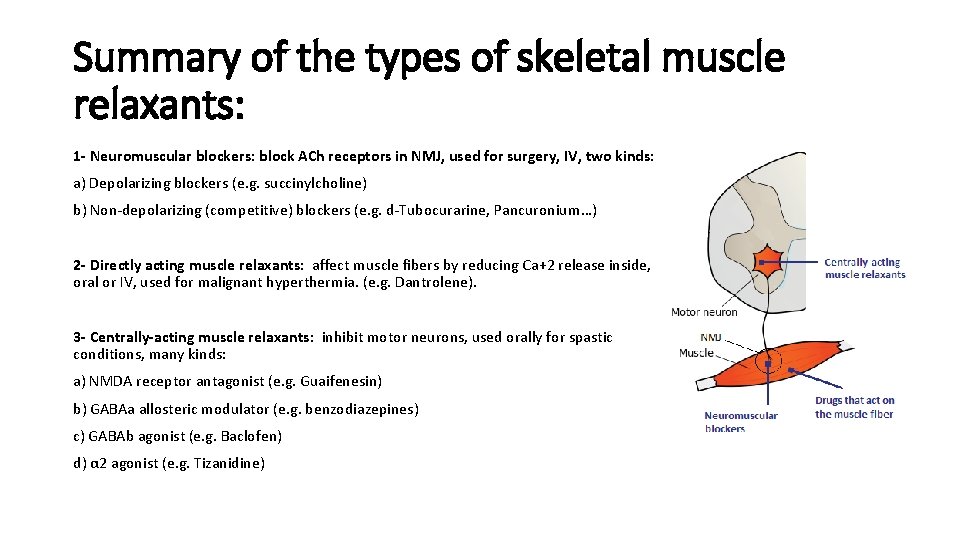
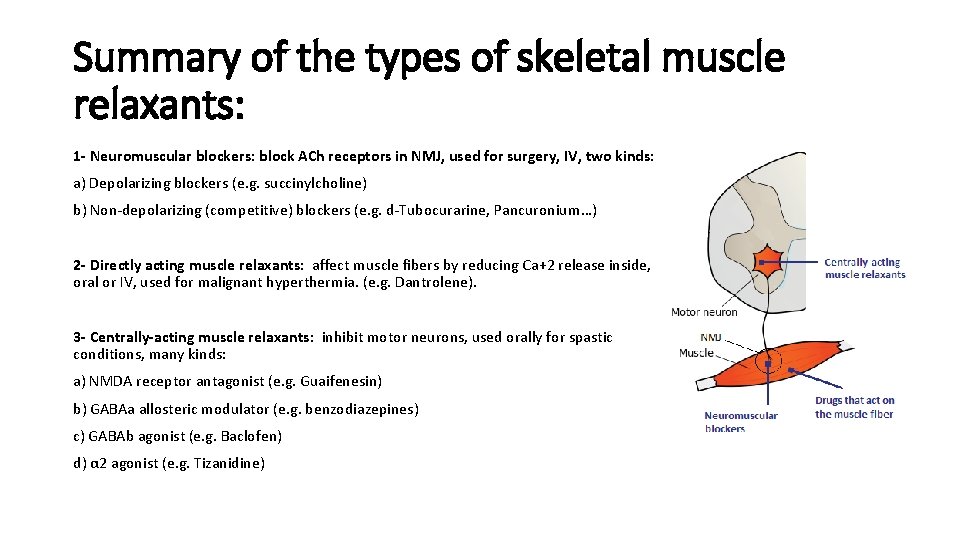
Summary of the types of skeletal muscle relaxants: 1 - Neuromuscular blockers: block ACh receptors in NMJ, used for surgery, IV, two kinds: a) Depolarizing blockers (e. g. succinylcholine) b) Non-depolarizing (competitive) blockers (e. g. d-Tubocurarine, Pancuronium…) 2 - Directly acting muscle relaxants: affect muscle fibers by reducing Ca+2 release inside, oral or IV, used for malignant hyperthermia. (e. g. Dantrolene). 3 - Centrally-acting muscle relaxants: inhibit motor neurons, used orally for spastic conditions, many kinds: a) NMDA receptor antagonist (e. g. Guaifenesin) b) GABAa allosteric modulator (e. g. benzodiazepines) c) GABAb agonist (e. g. Baclofen) d) α 2 agonist (e. g. Tizanidine)
THANK YOU SPECIAL THANKS TO DR M. ALAMRI FOR THE SLIDES ANY QUESTIONS
 Centrally acting skeletal muscle relaxants
Centrally acting skeletal muscle relaxants Dantrolene
Dantrolene Muscle relaxant classification
Muscle relaxant classification Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Skeletal muscle relaxants classification
Skeletal muscle relaxants classification Muscle relaxant classification
Muscle relaxant classification Phl to rdd
Phl to rdd Phl moodle
Phl moodle Microscopic anatomy of skeletal muscle
Microscopic anatomy of skeletal muscle Major muscle
Major muscle Skeletal muscles anterior view
Skeletal muscles anterior view Organization of muscle fibers
Organization of muscle fibers Fascicle
Fascicle White glistening bands attaching skeletal muscles
White glistening bands attaching skeletal muscles Skeletal and muscular system
Skeletal and muscular system Platys muscle shape
Platys muscle shape Major superficial skeletal muscles
Major superficial skeletal muscles Gap junction in smooth muscle
Gap junction in smooth muscle Skeletal muscles
Skeletal muscles Naming of muscles
Naming of muscles Name of muscle
Name of muscle Action of muscle relaxants
Action of muscle relaxants