NICE managing medicines in adult social care Mindy
![NICE guidance • Managing medicines in care homes. Social Care guideline [SC 1] Published NICE guidance • Managing medicines in care homes. Social Care guideline [SC 1] Published](https://slidetodoc.com/presentation_image_h2/d2c6e0bcdd466cc804620c6e786bb59c/image-3.jpg)


- Slides: 18
NICE – managing medicines in adult social care Mindy Bhalla Pharmacist Specialist, Care Quality Commission Cherise Gyimah Care Homes Pharmacist, Croydon CCG and NICE Medicines and Prescribing Associate Melanie Weatherley Chair Lincolnshire Care Association 1
Overview • Key recommendations on medicines policies, medicines reconciliation, self–administration and audit • A summary of the regulations • An overview of the newly published quality standard medicines management for people receiving social care in the community (QS 171) – What is medicines support? Assessing and recording medicines support • How providers can support self-care in social care. 2
![NICE guidance Managing medicines in care homes Social Care guideline SC 1 Published NICE guidance • Managing medicines in care homes. Social Care guideline [SC 1] Published](https://slidetodoc.com/presentation_image_h2/d2c6e0bcdd466cc804620c6e786bb59c/image-3.jpg)
NICE guidance • Managing medicines in care homes. Social Care guideline [SC 1] Published March 2014 • Managing medicines for adults receiving social care in the community. NICE guideline [NG 67] Published March 2017 • Medicines management for people receiving social care in the community. Quality standard [QS 171] Published July 2018 3
Health and social care act 2008 • Set out regulations for providers to meet • CQC inspection to ensure providers are meeting regulated activities • Some regulations include fundamental standards; the standards below which care must never fall • Guidance on meeting the regulated activities is provided on the CQC website. 4
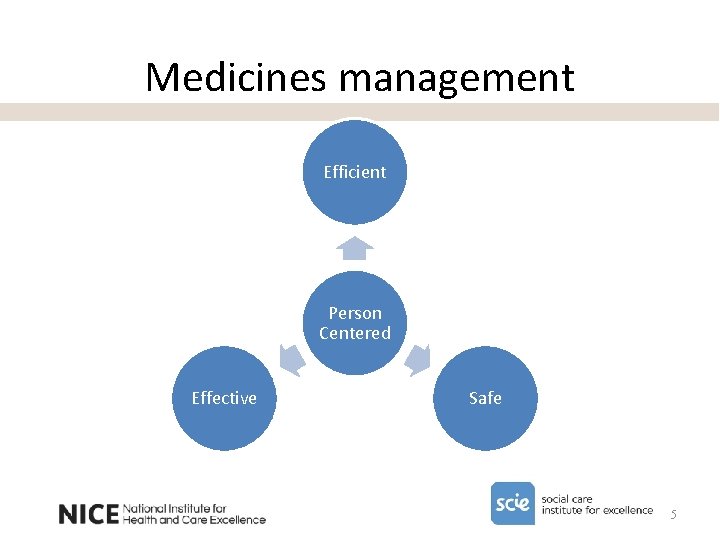
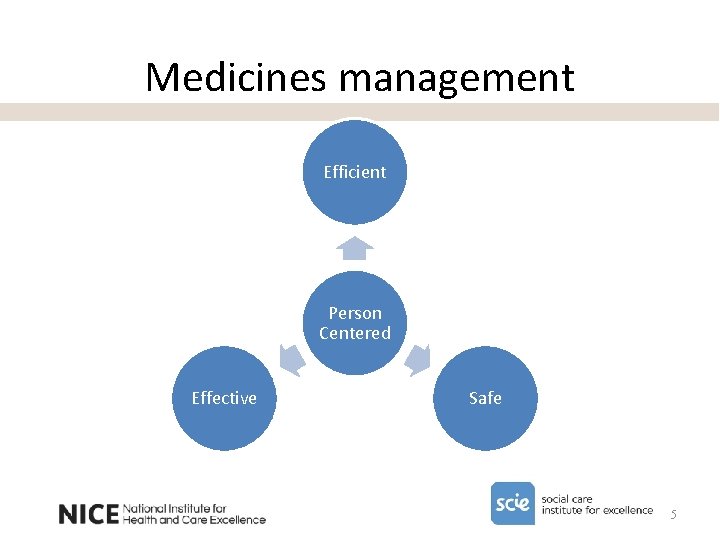
Medicines management Efficient Person Centered Effective Safe 5
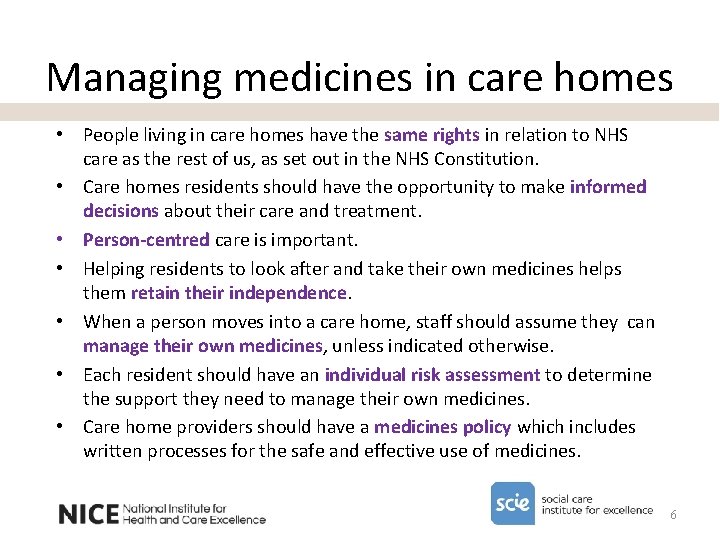
Managing medicines in care homes • People living in care homes have the same rights in relation to NHS care as the rest of us, as set out in the NHS Constitution. • Care homes residents should have the opportunity to make informed decisions about their care and treatment. • Person-centred care is important. • Helping residents to look after and take their own medicines helps them retain their independence. • When a person moves into a care home, staff should assume they can manage their own medicines, unless indicated otherwise. • Each resident should have an individual risk assessment to determine the support they need to manage their own medicines. • Care home providers should have a medicines policy which includes written processes for the safe and effective use of medicines. 6
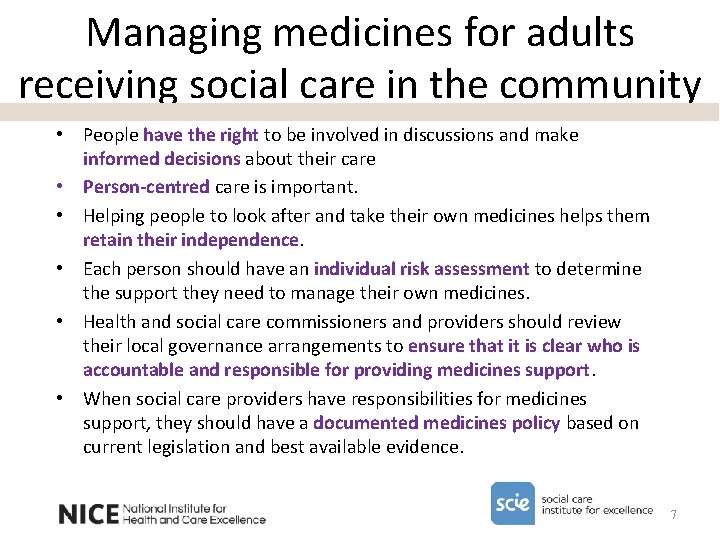
Managing medicines for adults receiving social care in the community • People have the right to be involved in discussions and make informed decisions about their care • Person-centred care is important. • Helping people to look after and take their own medicines helps them retain their independence. • Each person should have an individual risk assessment to determine the support they need to manage their own medicines. • Health and social care commissioners and providers should review their local governance arrangements to ensure that it is clear who is accountable and responsible for providing medicines support. • When social care providers have responsibilities for medicines support, they should have a documented medicines policy based on current legislation and best available evidence. 7
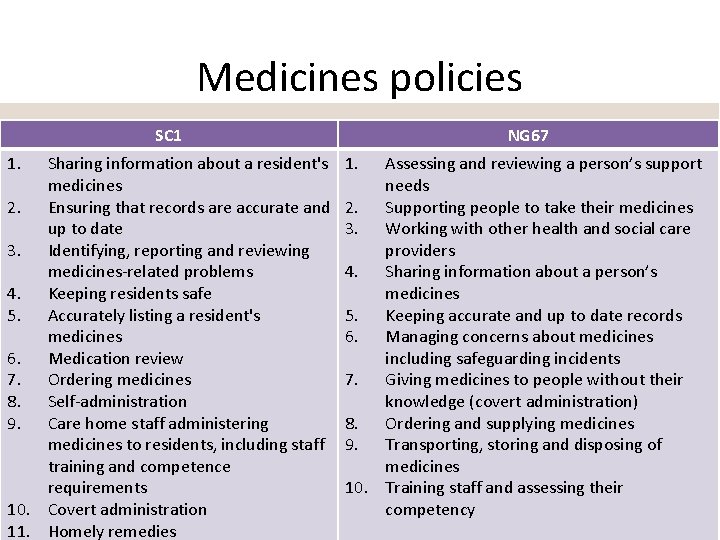
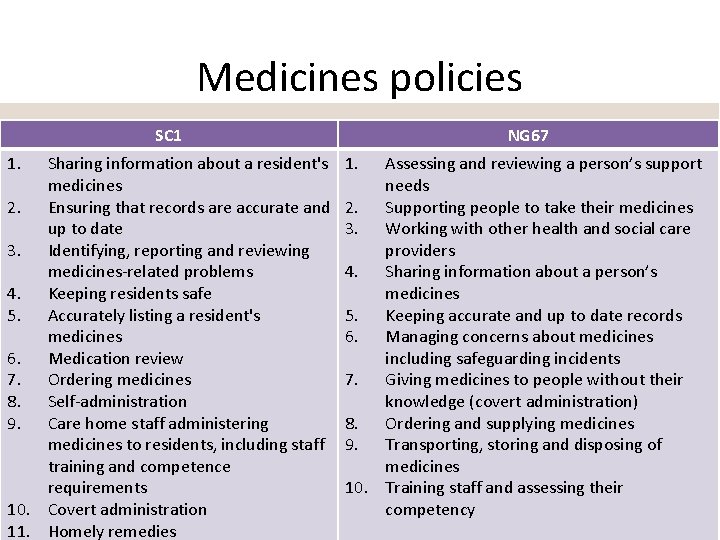
Medicines policies SC 1 1. Sharing information about a resident's medicines 2. Ensuring that records are accurate and up to date 3. Identifying, reporting and reviewing medicines-related problems 4. Keeping residents safe 5. Accurately listing a resident's medicines 6. Medication review 7. Ordering medicines 8. Self-administration 9. Care home staff administering medicines to residents, including staff training and competence requirements 10. Covert administration 11. Homely remedies NG 67 1. Assessing and reviewing a person’s support needs 2. Supporting people to take their medicines 3. Working with other health and social care providers 4. Sharing information about a person’s medicines 5. Keeping accurate and up to date records 6. Managing concerns about medicines including safeguarding incidents 7. Giving medicines to people without their knowledge (covert administration) 8. Ordering and supplying medicines 9. Transporting, storing and disposing of medicines 10. Training staff and assessing their competency 8


Medicines reconciliation • SC 1 The care home manager or person responsible for a resident's transfer into a care home should coordinate the accurate listing of all the resident's medicines as part of a full needs assessment and care plan and consider the resources needed for this to occur in a timely manner. (see recommendation 1. 7. 1) • NG 67 When social care providers have responsibilities for medicines support, they should have robust processes for communicating and sharing information about a person's medicines that take account of the person's expectations for confidentiality. (see recommendation 1. 4. 1) • NG 67 Social care providers with responsibilities for medicines support should have robust processes for handling changes to a person's medicines received verbally from a prescriber. (see recommendation 1. 4. 6) 10
Self administration • SC 1 Care home staff should assume that a resident can take and look after their medicines themselves (self-administer) unless a risk assessment has indicated otherwise. (see recommendation 1. 13. 1) • NG 67 Do NOT take responsibility for managing a person's medicines unless assessment indicates the need, and has been agreed as part of local governance arrangements. (see recommendation 1. 13. 1) • It is important for people living in care homes to maintain their independence, and that they can have as much involvement in taking their medicines as they want. • Care home providers should ensure they have a policy in place and that their process for self-administration of medicines (including controlled drugs) includes individual risk assessments, an assessment to ensure the appropriate support is provided, storage of medicines and record keeping. 11
Audit • A key responsibility for organisations providing care was highlighted in The Royal Pharmaceutical Society’s report (2012): – ensure systems and processes ‘focus on improving patient safety and patient outcomes’ and ‘consistently monitor and audit how effectively they transfer information about medicines’ 12
Self care • People who receive social care should be supported to access overthe-counter (OTC) products to enable them to self-care, with the appropriate safeguards put in place. • Access to OTC medicines to self-care is an issue of equality and providers should have policies in place to support people who wish to access OTC products in a timely manner. • This is different to the use of homely remedies. • Guidance for Clinical Commissioning Groups (CCGs) on conditions for which OTC medicines should not routinely be prescribed in primary care was published in March 2018. Providers need to liaise closely with clinicians to identify people who are affected and make appropriate arrangements. 13
Medicines support The person’s medicines support needs should be identified and assessed as part of the overall assessment of their needs and preferences for care and treatment. People undertaking this assessment must have the necessary knowledge, skills and experience to do so. The person (and their family) should be involved in all stages of the process. Before any medicines support is provided by a social care provider, commissioning and contractual arrangements need to be discussed, agreed and recorded as part of the local care planning process. This is to ensure that it is clear who is responsible and accountable for the decisions being made, and which providers will deliver each aspect of medicines support. 14
QS 171 Statement 1 Adults having an assessment for social care in the community have their medicines support needs included in the assessment. Statement 2 Adults receiving medicines support in the community from a social care provider have their general practice and supplying pharmacy informed that support has started. Statement 3 Adults receiving medicines support in the community from a social care provider have a record of the medicines support that they need in their care plan. Statement 4 Adults receiving medicines support in the community from a social care provider are given information on how to raise any medicinesrelated problems. 15
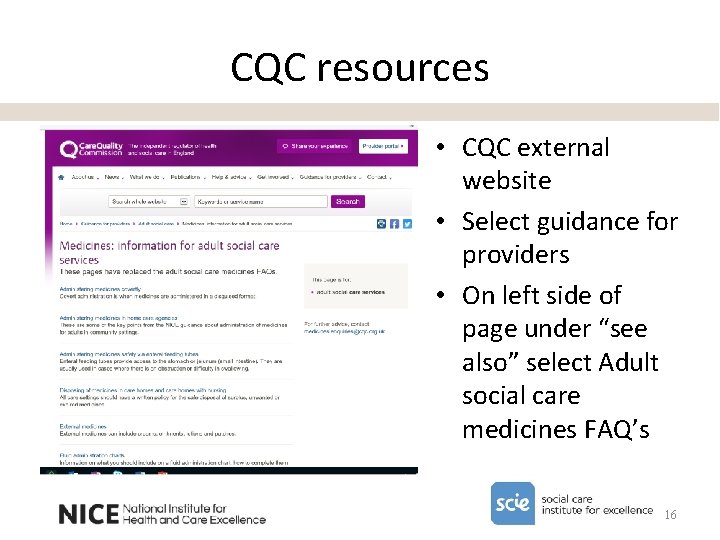
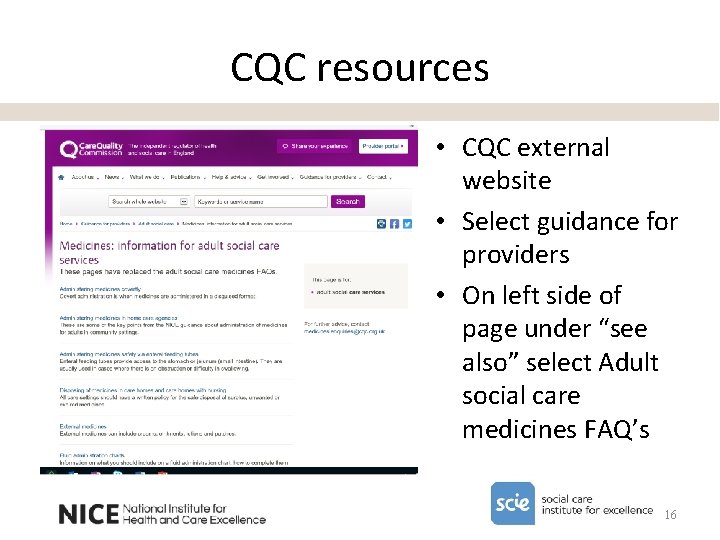
CQC resources • CQC external website • Select guidance for providers • On left side of page under “see also” select Adult social care medicines FAQ’s 16
NICE resources Sign up for the NICE social care newsletter http: //www. nice. org. uk/social-care-newsletter Access our range of quick guides https: //www. nice. org. uk/about/nice-communities/socialcare/quick-guides 17
Managing medicines quick guides 18
 Adult care sheffield
Adult care sheffield Adult social care kingston
Adult social care kingston 294/7
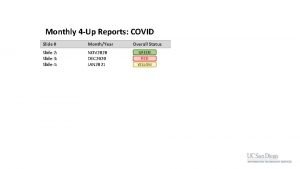
294/7 4up report
4up report Shape2sql
Shape2sql Mindy mayo
Mindy mayo Mindy ms md
Mindy ms md Mindy laughlin
Mindy laughlin Alfie kohn classroom management
Alfie kohn classroom management Types of care primary secondary tertiary
Types of care primary secondary tertiary Amber care bundle nice
Amber care bundle nice Unit 2 equality diversity and rights
Unit 2 equality diversity and rights Veterinary medicines directorate
Veterinary medicines directorate Glencoe health chapter 19 medicines and drugs
Glencoe health chapter 19 medicines and drugs George's marvellous medicine story
George's marvellous medicine story Medicines management programme
Medicines management programme Specially constructed stainless steel truck
Specially constructed stainless steel truck Niyog niyogan benefits
Niyog niyogan benefits European directorate for the quality of medicines
European directorate for the quality of medicines