MENZIES SCHOOL OF HEALTH RESEARCH Evaluation of the

- Slides: 7
MENZIES SCHOOL OF HEALTH RESEARCH Evaluation of the Central Australian Medical Retrieval and Consultation Centre
What’s the problem? • Remote Central Australia is geographically large and has a sparse population; • Burden of disease and mortality rates increase with increasing remoteness; • Need for effective primary health care; • Need for effective and timely emergency services; • February 2018 dedicated Medical Retrieval and Consultation Centre (MRa. CC) established: • Streamline communications, reflecting best practice in retrieval medicine, improve quality of emergency care.
What difference will our research make? • Changes in the timeliness of specialist emergency advice and retrieval; • Impact of MRa. CC on remote clinicians and efficiency for remote clinicians; • Changes in efficiency for ED FACEMs; • Changes in outcomes for patients; • Quantify the cost and cost-effectiveness of the MRa. CC model compared to the previous GP-led model.
Collaborators • Prof John Wakerman, MSHR • Dr Deborah Russell, MSHR • Dr Michelle Fitts, MSHR • Zania Liddle, MSHR • Dr Supriya Mathew, MSHR • Dr Richard Johnson, CAHS • Dr Petra Niclasen, CAHS • Dr David Reeve, CAHS • Dr Bridget Honan, CAHS • Dr Yuejen Zhao, TEHS • Dr Danielle Green, TEHS
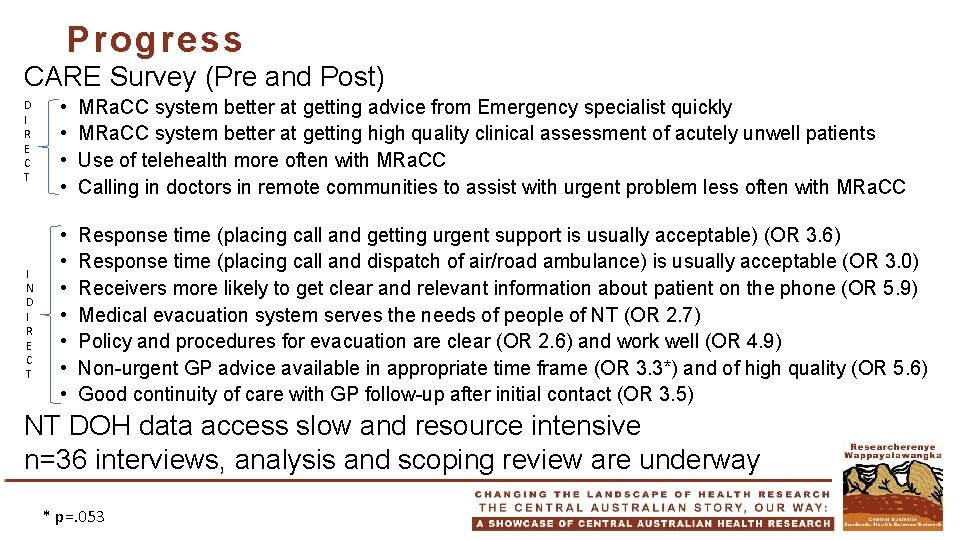
Progress CARE Survey (Pre and Post) D I R E C T I N D I R E C T • • MRa. CC system better at getting advice from Emergency specialist quickly MRa. CC system better at getting high quality clinical assessment of acutely unwell patients Use of telehealth more often with MRa. CC Calling in doctors in remote communities to assist with urgent problem less often with MRa. CC • • Response time (placing call and getting urgent support is usually acceptable) (OR 3. 6) Response time (placing call and dispatch of air/road ambulance) is usually acceptable (OR 3. 0) Receivers more likely to get clear and relevant information about patient on the phone (OR 5. 9) Medical evacuation system serves the needs of people of NT (OR 2. 7) Policy and procedures for evacuation are clear (OR 2. 6) and work well (OR 4. 9) Non-urgent GP advice available in appropriate time frame (OR 3. 3*) and of high quality (OR 5. 6) Good continuity of care with GP follow-up after initial contact (OR 3. 5) NT DOH data access slow and resource intensive n=36 interviews, analysis and scoping review are underway * p=. 053
Lessons learned üSignificant changes in timeliness of advice in emergencies üSignificant changes in quality of emergency care üImpact on quality of PHC üImpact on efficiency for FACEMs ? Impact on efficiency for remote clinicians ? Impact on streamlining and timeliness of PHC advice ? Outcomes for patients ? Cost and cost-effectiveness