Medtech in Transition Where Are We Now and

- Slides: 8

Medtech in Transition: Where Are We Now and What Lies Ahead State of Coverage With Evidence Development in 2017 and Future Directions Mitchell Sugarman Anchor Bay Consulting
Mitchell Sugarman, MBA • Disclosure Statement of Financial Interest I hold stock in multiple medical device and pharmaceutical companies I am a consultant for multiple medical device companies to provide expertise in health economics and reimbursement
Progress Towards Achieving Better Care, Smarter Spending, Healthier People Jan 26, 2015 By: Sylvia Mathews Burwell, HHS Secretary “Today, for the first time, we are setting clear goals – and establishing a clear timeline – for moving from volume to value in Medicare payments. ” http: //www. hhs. gov/blog/2015/01/26/progress-towards-better-care-smarter-spending-healthier-people. html Burwell SM. Setting value-based payment goals--HHS efforts to improve U. S. health care. N Engl J Med. 2015 Mar 5; 372(10): 897 -9. doi: 10. 1056/NEJMp 1500445. Epub 2015 Jan 26. PMID: 25622024
Coverage With Evidence Development (CED) • Coverage in the context of approved clinical studies or with the collection of additional clinical data • Allows for positive coverage when evidence is insufficient for a more favorable decision • Without CED, the item or service would be non-covered • May involve randomized controlled trials, observational studies, registries and claims data
Why CED? • Provide access to promising technology for which the evidence base may be immature. • Help identify the circumstances in which patients are most likely to benefit and potentially accelerate access to innovations • Will lead to the production of evidence complementary to existing medical evidence • The NCD process, in general, is a transparent one… – Requesters may meet with CMS and frequent, informal contact is possible. A tracking sheet is posted on the CMS website that allows interested individuals to participate in and monitor the progress of the review. A proposed decision is issued for public comment within six months of opening the NCD review. • …But improvements on CED process may be useful – The 30 -day comment period on proposed NCDs may be insufficient to fully incorporate stakeholder views and arrive at well-balanced CED requirements for specific therapies. Modifications that allow for broader stakeholder input would improve the process.
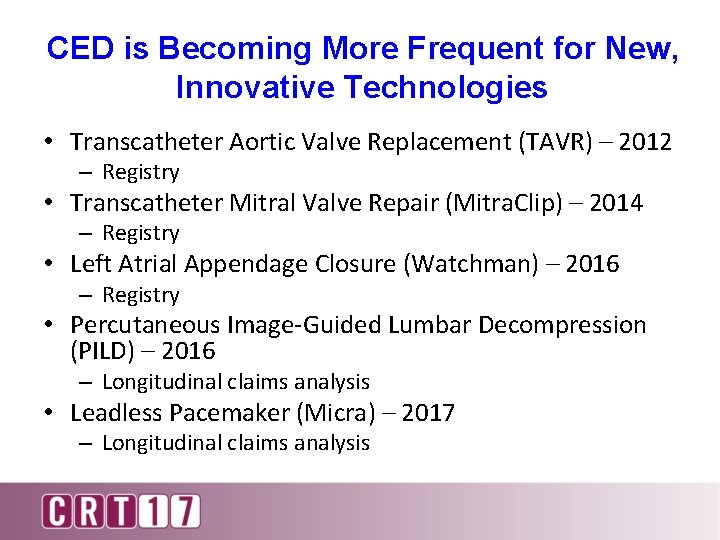
CED is Becoming More Frequent for New, Innovative Technologies • Transcatheter Aortic Valve Replacement (TAVR) – 2012 – Registry • Transcatheter Mitral Valve Repair (Mitra. Clip) – 2014 – Registry • Left Atrial Appendage Closure (Watchman) – 2016 – Registry • Percutaneous Image-Guided Lumbar Decompression (PILD) – 2016 – Longitudinal claims analysis • Leadless Pacemaker (Micra) – 2017 – Longitudinal claims analysis
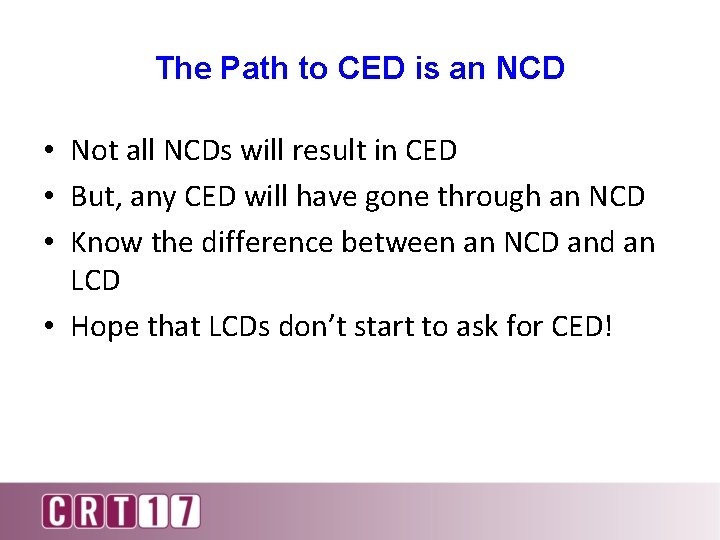
The Path to CED is an NCD • Not all NCDs will result in CED • But, any CED will have gone through an NCD • Know the difference between an NCD and an LCD • Hope that LCDs don’t start to ask for CED!
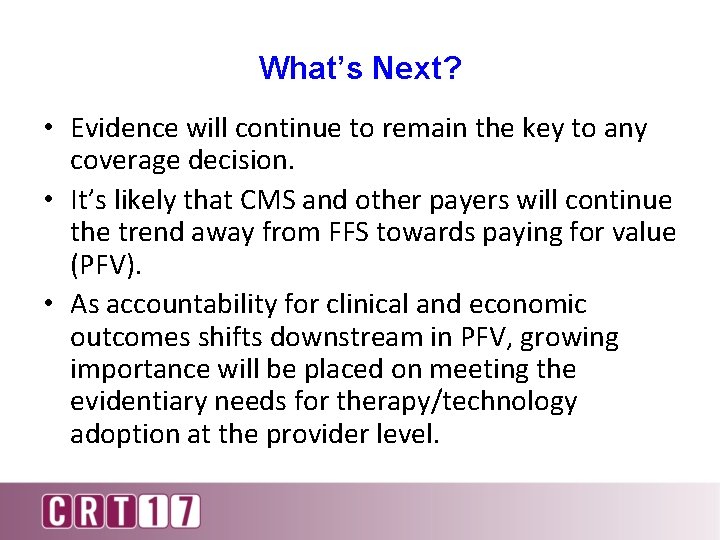
What’s Next? • Evidence will continue to remain the key to any coverage decision. • It’s likely that CMS and other payers will continue the trend away from FFS towards paying for value (PFV). • As accountability for clinical and economic outcomes shifts downstream in PFV, growing importance will be placed on meeting the evidentiary needs for therapy/technology adoption at the provider level.