Medicaids Changing Landscape Mississippi Association of Health Plans

- Slides: 18
Medicaid’s Changing Landscape Mississippi Association of Health Plans Annual Meeting Toby Douglas, SVP Medicaid Solutions October 19, 2016 1
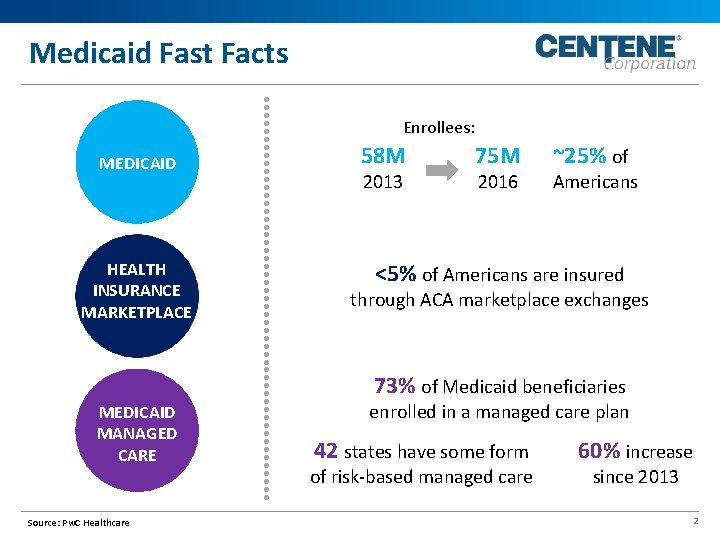
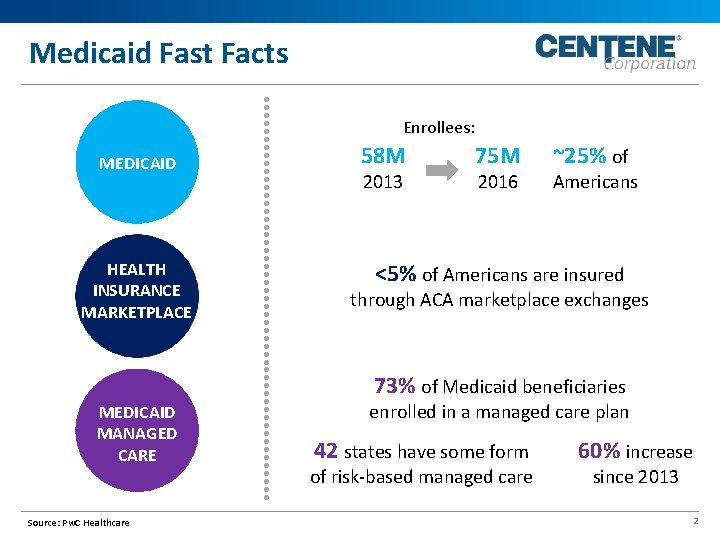
Medicaid Fast Facts Enrollees: MEDICAID HEALTH INSURANCE MARKETPLACE 58 M 2013 75 M 2016 ~25% of Americans <5% of Americans are insured through ACA marketplace exchanges 73% of Medicaid beneficiaries MEDICAID MANAGED CARE Source: Pw. C Healthcare enrolled in a managed care plan 42 states have some form of risk-based managed care 60% increase since 2013 2
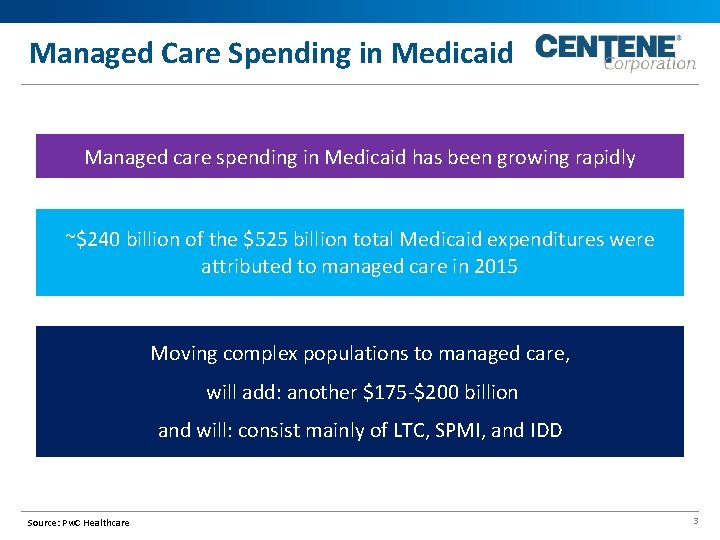
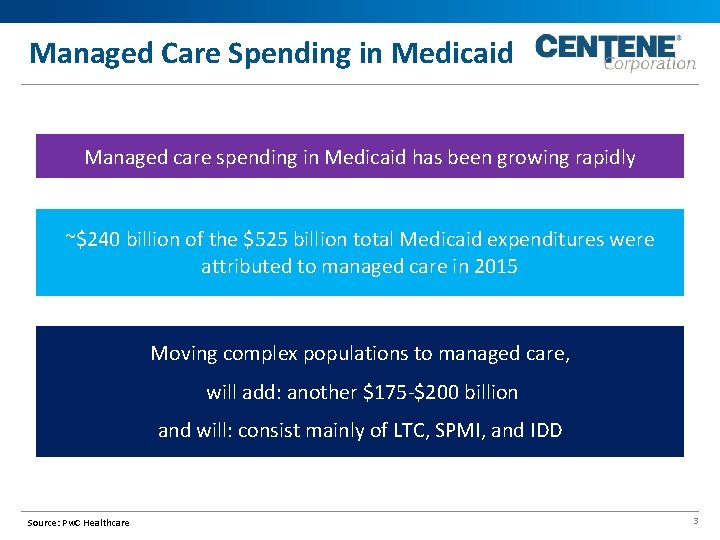
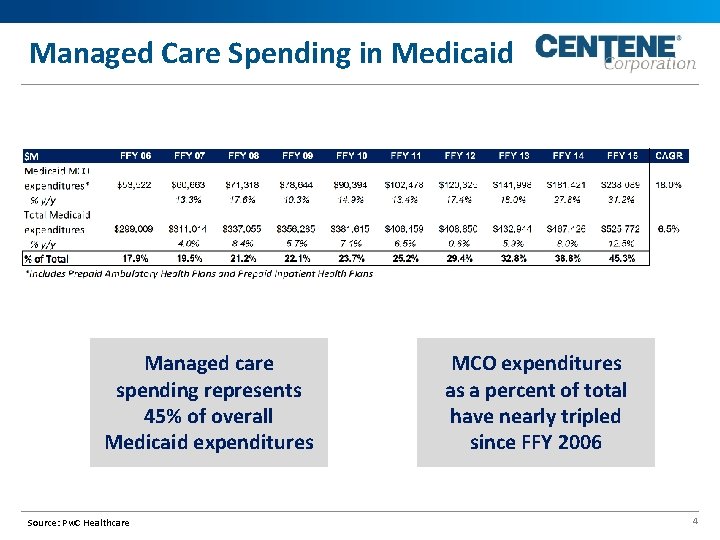
Managed Care Spending in Medicaid Managed care spending in Medicaid has been growing rapidly ~$240 billion of the $525 billion total Medicaid expenditures were attributed to managed care in 2015 Moving complex populations to managed care, will add: another $175 -$200 billion and will: consist mainly of LTC, SPMI, and IDD Source: Pw. C Healthcare 3
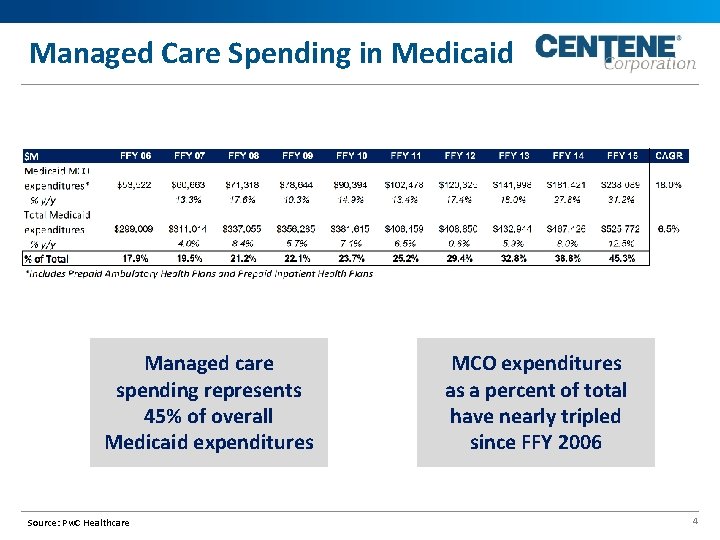
Managed Care Spending in Medicaid Managed care spending represents 45% of overall Medicaid expenditures Source: Pw. C Healthcare MCO expenditures as a percent of total have nearly tripled since FFY 2006 4
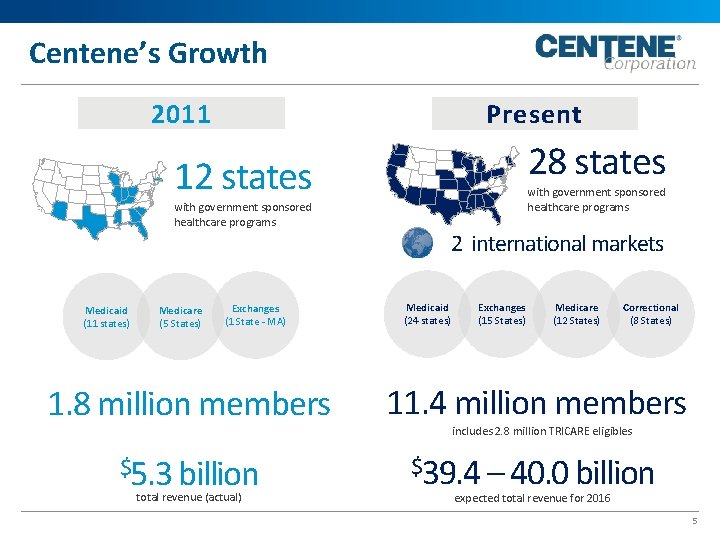
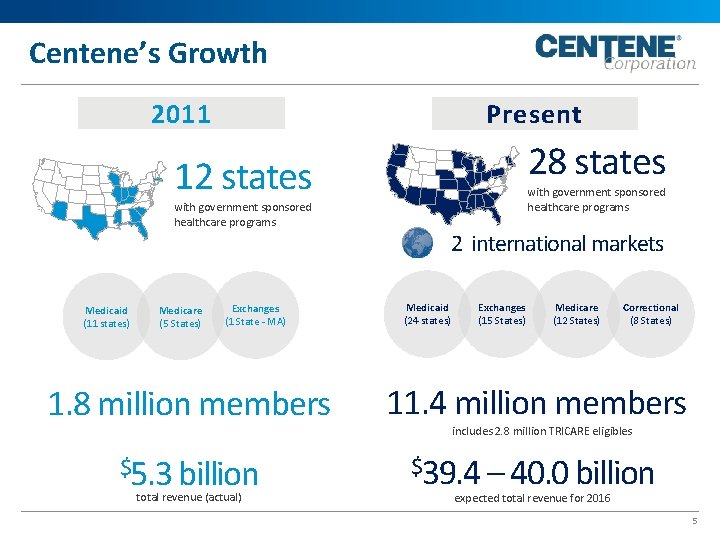
Centene’s Growth 2011 Present 28 states 12 states with government sponsored healthcare programs Medicaid (11 states) Medicare (5 States) Exchanges (1 State - MA) 2 international markets Medicaid (24 states) Exchanges (15 States) Medicare (12 States) Correctional (8 States) 1. 8 million members 11. 4 million members $5. 3 billion $39. 4 – 40. 0 billion total revenue (actual) includes 2. 8 million TRICARE eligibles expected total revenue for 2016 5

National Trends
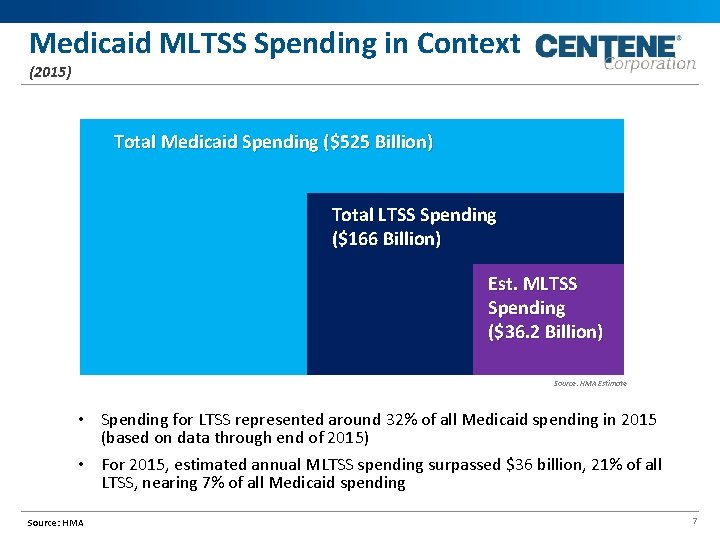
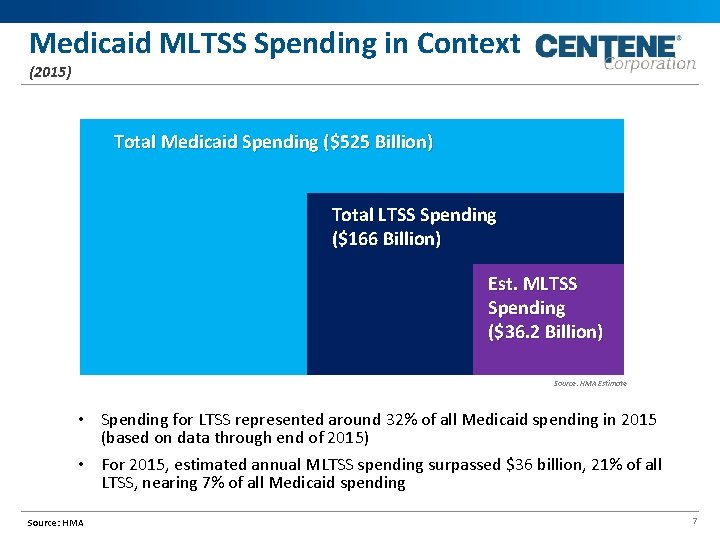
Medicaid MLTSS Spending in Context (2015) Total Medicaid Spending ($525 Billion) Total LTSS Spending ($166 Billion) Est. MLTSS Spending ($36. 2 Billion) Source: HMA Estimate • Spending for LTSS represented around 32% of all Medicaid spending in 2015 (based on data through end of 2015) • For 2015, estimated annual MLTSS spending surpassed $36 billion, 21% of all LTSS, nearing 7% of all Medicaid spending Source: HMA 7
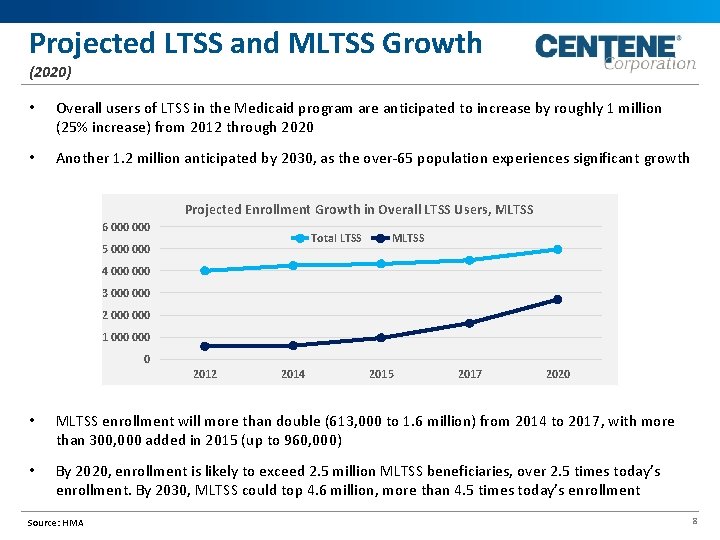
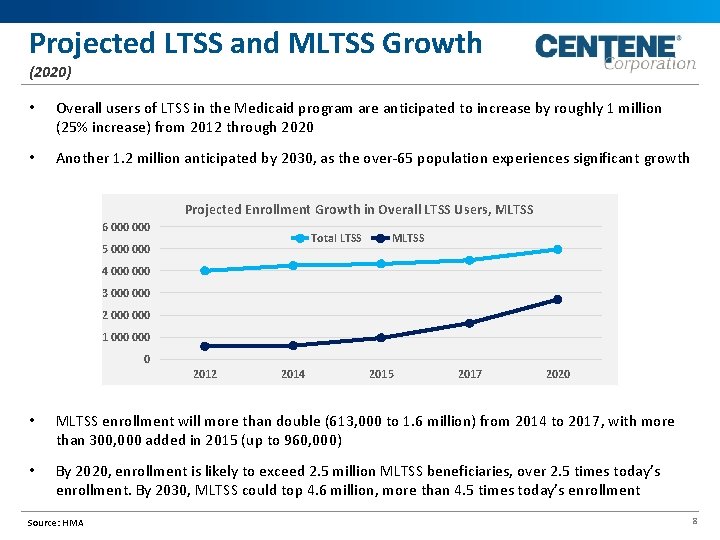
Projected LTSS and MLTSS Growth (2020) • Overall users of LTSS in the Medicaid program are anticipated to increase by roughly 1 million (25% increase) from 2012 through 2020 • Another 1. 2 million anticipated by 2030, as the over-65 population experiences significant growth Projected Enrollment Growth in Overall LTSS Users, MLTSS 6 000 Total LTSS 5 000 MLTSS 4 000 3 000 2 000 1 000 0 2012 2014 2015 2017 2020 • MLTSS enrollment will more than double (613, 000 to 1. 6 million) from 2014 to 2017, with more than 300, 000 added in 2015 (up to 960, 000) • By 2020, enrollment is likely to exceed 2. 5 million MLTSS beneficiaries, over 2. 5 times today’s enrollment. By 2030, MLTSS could top 4. 6 million, more than 4. 5 times today’s enrollment Source: HMA 8
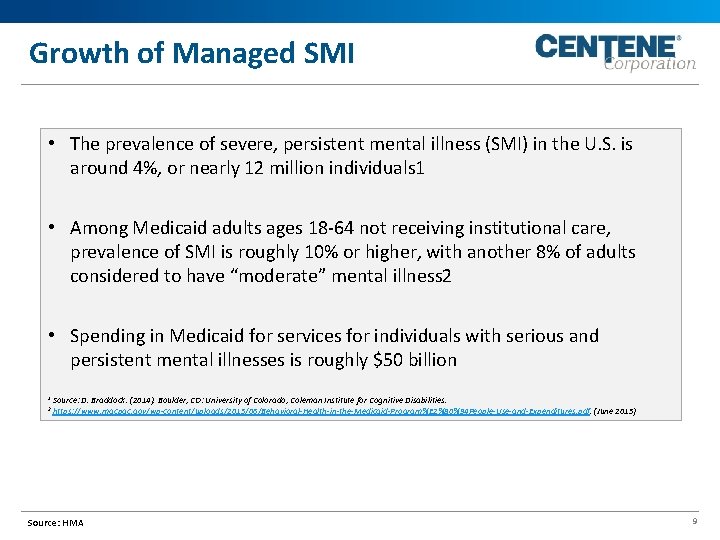
Growth of Managed SMI • The prevalence of severe, persistent mental illness (SMI) in the U. S. is around 4%, or nearly 12 million individuals 1 • Among Medicaid adults ages 18 -64 not receiving institutional care, prevalence of SMI is roughly 10% or higher, with another 8% of adults considered to have “moderate” mental illness 2 • Spending in Medicaid for services for individuals with serious and persistent mental illnesses is roughly $50 billion 1 2 Source: D. Braddock. (2014). Boulder, CO: University of Colorado, Coleman Institute for Cognitive Disabilities. https: //www. macpac. gov/wp-content/uploads/2015/06/Behavioral-Health-in-the-Medicaid-Program%E 2%80%94 People-Use-and-Expenditures. pdf. (June 2015) Source: HMA 9
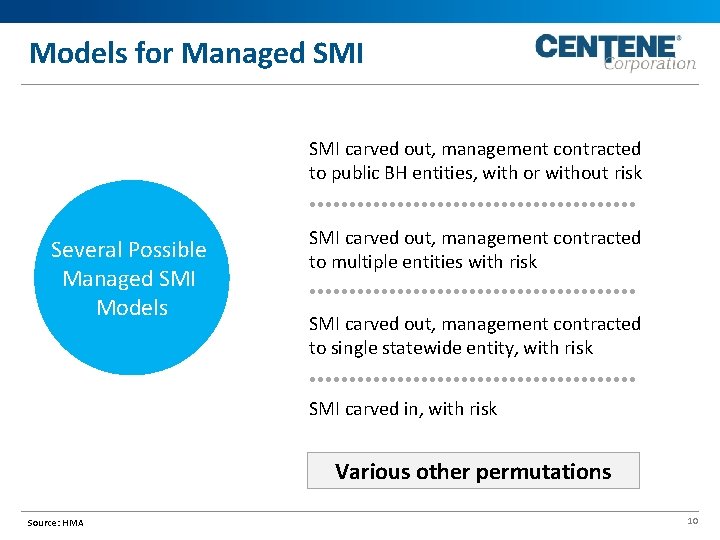
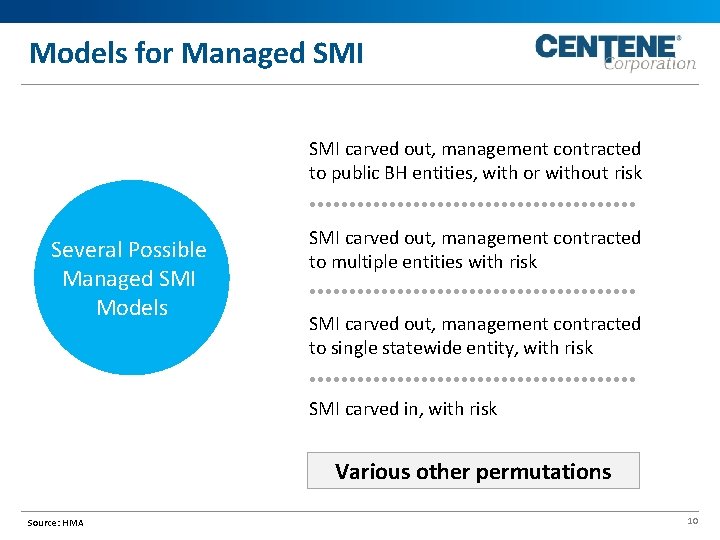
Models for Managed SMI carved out, management contracted to public BH entities, with or without risk Several Possible Managed SMI Models SMI carved out, management contracted to multiple entities with risk SMI carved out, management contracted to single statewide entity, with risk SMI carved in, with risk Various other permutations Source: HMA 10
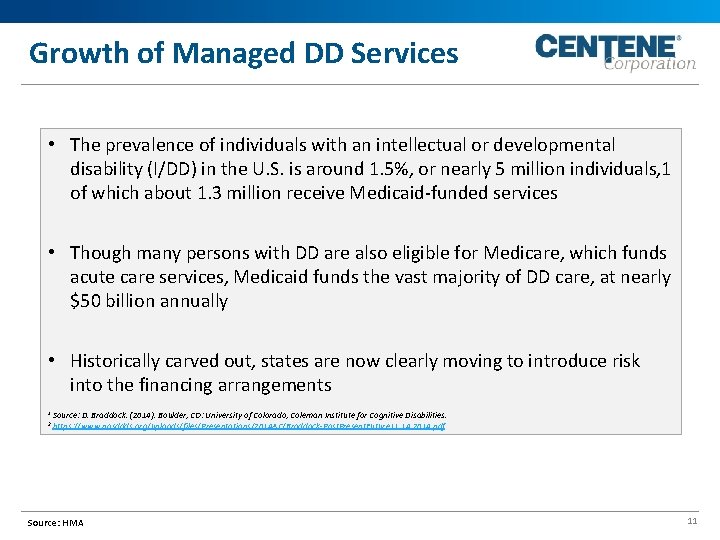
Growth of Managed DD Services • The prevalence of individuals with an intellectual or developmental disability (I/DD) in the U. S. is around 1. 5%, or nearly 5 million individuals, 1 of which about 1. 3 million receive Medicaid-funded services • Though many persons with DD are also eligible for Medicare, which funds acute care services, Medicaid funds the vast majority of DD care, at nearly $50 billion annually • Historically carved out, states are now clearly moving to introduce risk into the financing arrangements 1 2 Source: D. Braddock. (2014). Boulder, CO: University of Colorado, Coleman Institute for Cognitive Disabilities. https: //www. nasddds. org/uploads/files/Presentations/2014 AC/Braddock-Past. Present. Future 11. 14. 2014. pdf Source: HMA 11
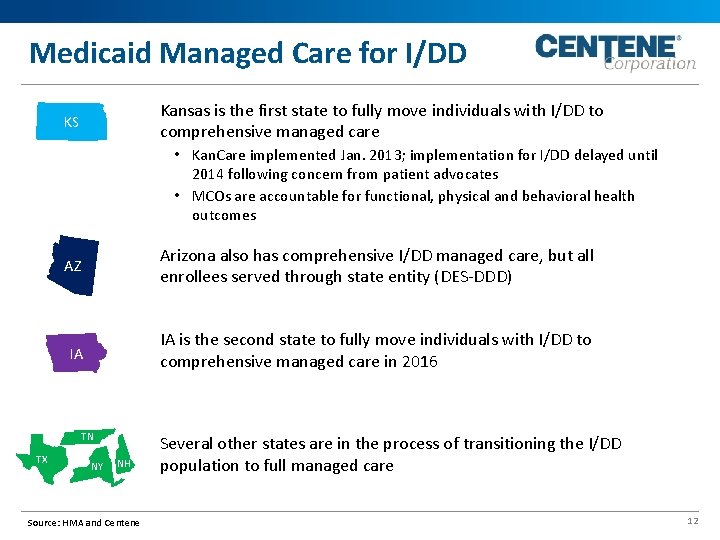
Medicaid Managed Care for I/DD Kansas is the first state to fully move individuals with I/DD to comprehensive managed care KS • Kan. Care implemented Jan. 2013; implementation for I/DD delayed until 2014 following concern from patient advocates • MCOs are accountable for functional, physical and behavioral health outcomes AZ Arizona also has comprehensive I/DD managed care, but all enrollees served through state entity (DES-DDD) IA IA is the second state to fully move individuals with I/DD to comprehensive managed care in 2016 TN TX NY NH Source: HMA and Centene Several other states are in the process of transitioning the I/DD population to full managed care 12
Serving Complex Members The differences between who we serve today and more complex members are dramatic: • Now serving members who can be with the plan for life who are often frequent users of multiple specialty healthcare providers • Complex members often seek choice, control and independence at a different level • Plans are being forced to think through a new integrated model of care • A new framework for the services we must deliver: medical, social, nutritional, housing, employment • New intellectual assets: people who understand this population • New systems for tracking and measuring performance • New ways of assembling, organizing, and paying providers into new kinds of delivery systems Source: HMA 13
Changing Dynamics Palliative Care Telehealth 14
Home-Based Palliative Care (HBPC) • 107 referrals, 79 enrolled into HBPC (73. 8%) • 34 Cancer, 15 ESRD, 5 CHF, 5 Neuro, 4 COPD, 3 ESLD, 13 Others • ALOS=4 months • Avoidable Acute Admits=69, Avoidable ER visits=19 • 40% enrollment in hospice, Mean time in hospice=22. 4 days, Median time in hospice=8 days • Death rate in home= 67% vs national average is 25. 4% • Net savings per enrollee=$14, 550 15
Telehealth Solutions ELECTRONIC CONSULTATION STORE - AND FORWARD LIVE VIDEO 16
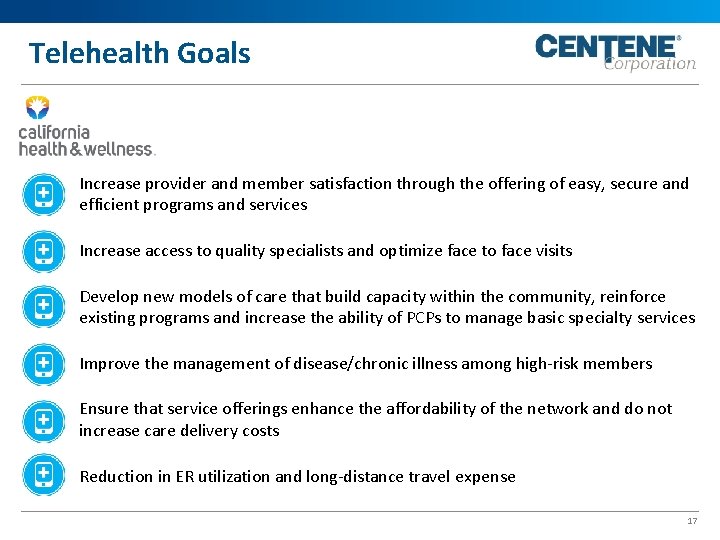
Telehealth Goals Increase provider and member satisfaction through the offering of easy, secure and efficient programs and services Increase access to quality specialists and optimize face to face visits Develop new models of care that build capacity within the community, reinforce existing programs and increase the ability of PCPs to manage basic specialty services Improve the management of disease/chronic illness among high-risk members Ensure that service offerings enhance the affordability of the network and do not increase care delivery costs Reduction in ER utilization and long-distance travel expense 17
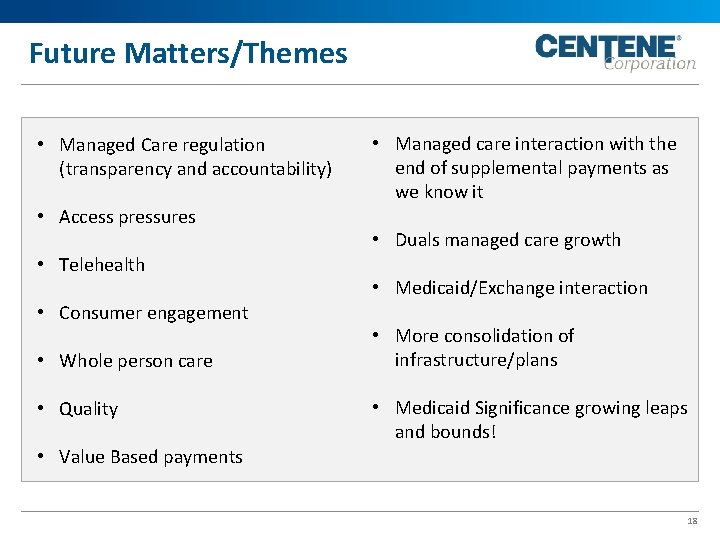
Future Matters/Themes • Managed Care regulation (transparency and accountability) • Access pressures • Telehealth • Consumer engagement • Whole person care • Quality • Managed care interaction with the end of supplemental payments as we know it • Duals managed care growth • Medicaid/Exchange interaction • More consolidation of infrastructure/plans • Medicaid Significance growing leaps and bounds! • Value Based payments 18
 Changing marketing landscape
Changing marketing landscape 6-1 a changing landscape
6-1 a changing landscape Section 6-1 a changing landscape
Section 6-1 a changing landscape The changing marketing landscape rapid globalization
The changing marketing landscape rapid globalization Arizona landscape contractors association
Arizona landscape contractors association Wind and hail insurance biloxi ms
Wind and hail insurance biloxi ms Mississippi association of school business officials
Mississippi association of school business officials Landscape section of a health policy analysis
Landscape section of a health policy analysis Rocky mountain health plans dualcare plus
Rocky mountain health plans dualcare plus Mental health policy, plans and programmes michelle funk
Mental health policy, plans and programmes michelle funk Po box 1220 philadelphia pa 19105 provider phone number
Po box 1220 philadelphia pa 19105 provider phone number Mhc fully integrated managed care
Mhc fully integrated managed care Wisconsin public health association
Wisconsin public health association Virginia health information management association
Virginia health information management association Cham malawi
Cham malawi New york counseling association
New york counseling association Mental health lawyers association
Mental health lawyers association American association on health and disability
American association on health and disability Wisconsin public health association
Wisconsin public health association