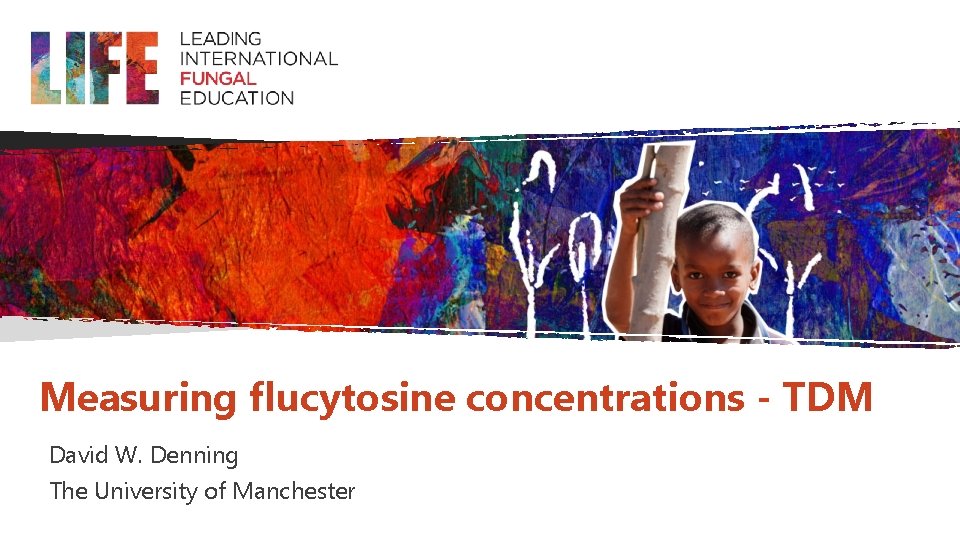
Measuring flucytosine concentrations TDM David W Denning The
- Slides: 12
Measuring flucytosine concentrations - TDM David W. Denning The University of Manchester
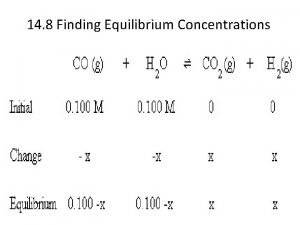
Intended Learning Outcomes To understand the pharmacokinetics of flucytosine, relevant to under- and over-dosing To appreciate the different methods used for measuring flucytosine concentrations To know how to interpret flucytosine concentrations in the clinical setting
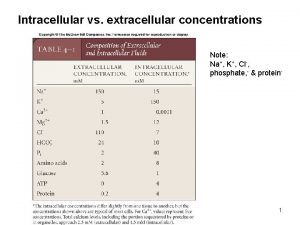
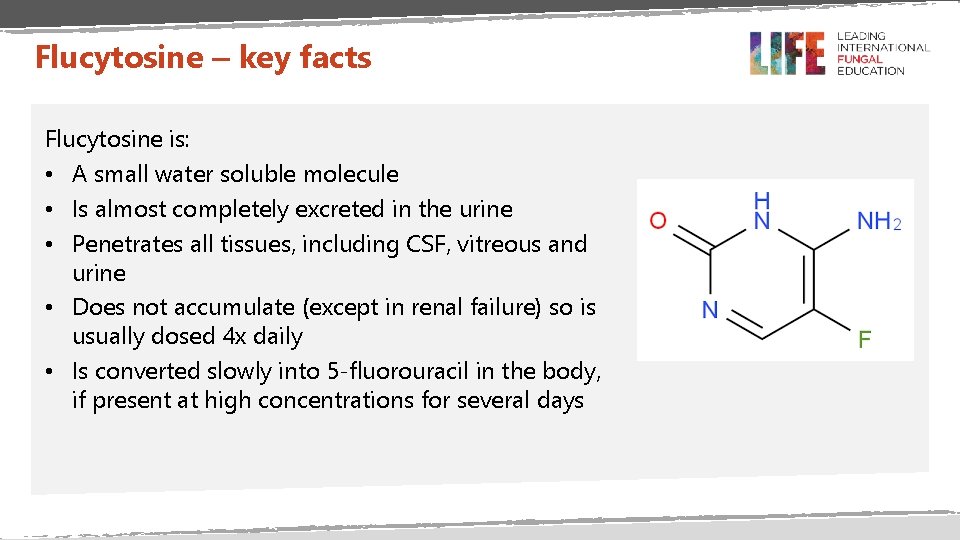
Flucytosine – key facts Flucytosine is: • A small water soluble molecule • Is almost completely excreted in the urine • Penetrates all tissues, including CSF, vitreous and urine • Does not accumulate (except in renal failure) so is usually dosed 4 x daily • Is converted slowly into 5 -fluorouracil in the body, if present at high concentrations for several days
Flucytosine dosing Standard dosing is 25 mg/kg every 6 hours So a 50 kg woman would receive 1. 25 g 4 x a day (a total of 5 g per day) A 10 kg child would receive 250 mg 4 x a day A 100 kg adult would receive 2. 5 g 4 x a day (a total of 10 g per day) Older literature and current data sheets recommend 37. 5 - 50 mg/kg every 6 hours - this is unnecessarily high
Flucytosine dosing and renal failure Dosing frequency adjustment in renal dysfunction • Creatinine clearance <40 to >20 ml /min: 25 mg/kg every 12 hours • Creatinine clearance <20 to >10 ml /min: 25 mg/kg every 24 hours • Creatinine clearance <10 ml /min: an initial single dose of 25 mg/kg; subsequent doses should be calculated according to the results of regular monitoring of the serum concentration of the drug, which should not be allowed to exceed 80 micrograms/ml • Blood levels of 25 to 50 micrograms/ml (mg/L) are normally effective
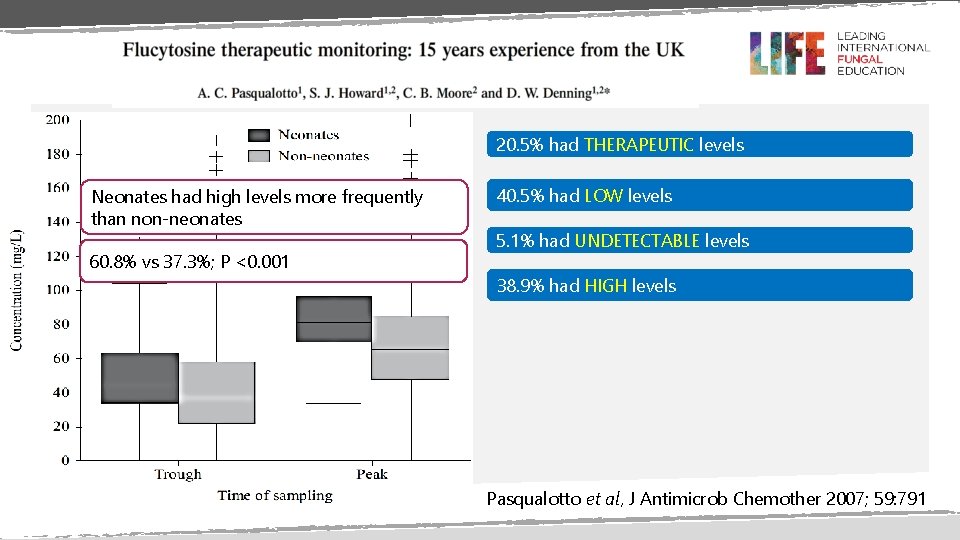
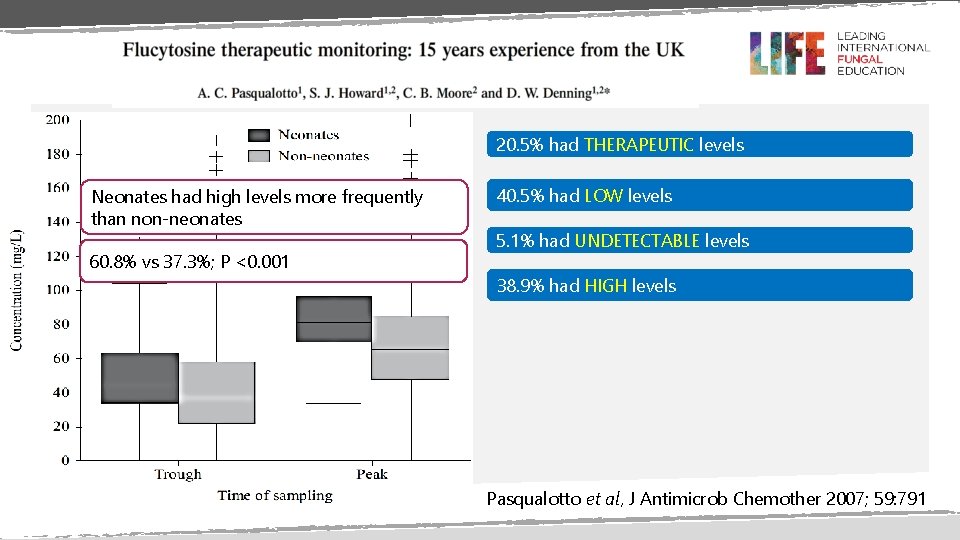
20. 5% had THERAPEUTIC levels Neonates had high levels more frequently than non-neonates 60. 8% vs 37. 3%; P <0. 001 40. 5% had LOW levels 5. 1% had UNDETECTABLE levels 38. 9% had HIGH levels Pasqualotto et al, J Antimicrob Chemother 2007; 59: 791
Indications for flucytosine TDM Not usually required except in: • Renal failure and impairment • Neonates • Patients on haemofiltration and/or dialysis • Patients on ECMO or other filters • Patients with very short guts (usually on long term total parenteral nutrition) • In long term therapy to check appropriate oral dosing Ashbee et al, J Antimicrob Chemother 2014; 69: 1162
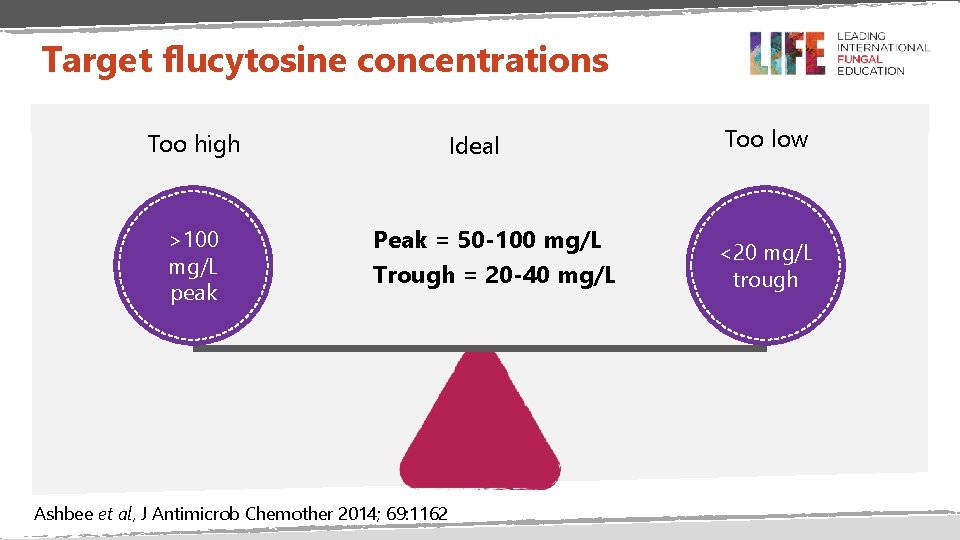
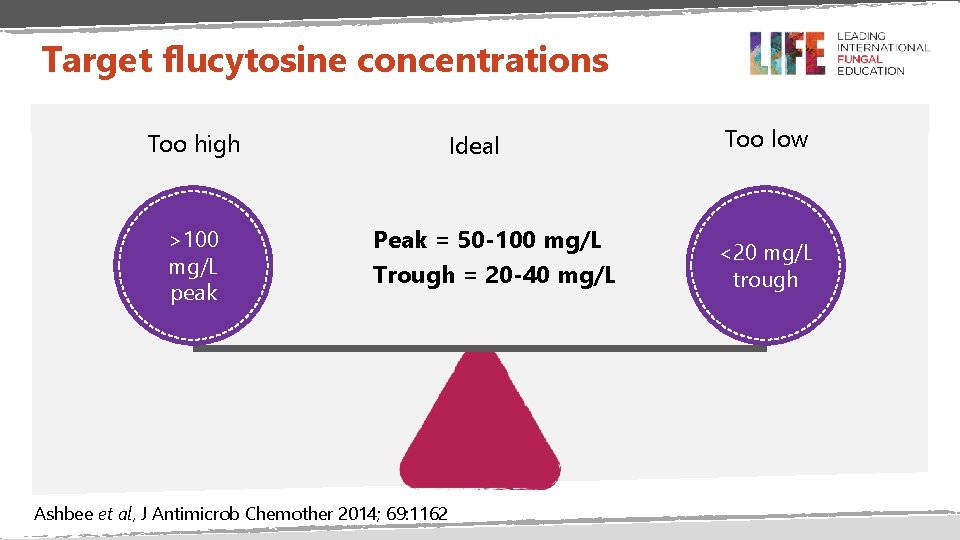
Target flucytosine concentrations Too high >100 mg/L peak Ideal Peak = 50 -100 mg/L Trough = 20 -40 mg/L Ashbee et al, J Antimicrob Chemother 2014; 69: 1162 Too low <20 mg/L trough
Flucytosine assay methods • • • Bioassay High-pressure liquid chromatography (HPLC) Gas-liquid chromatography Fluorometry Enzymatic methods
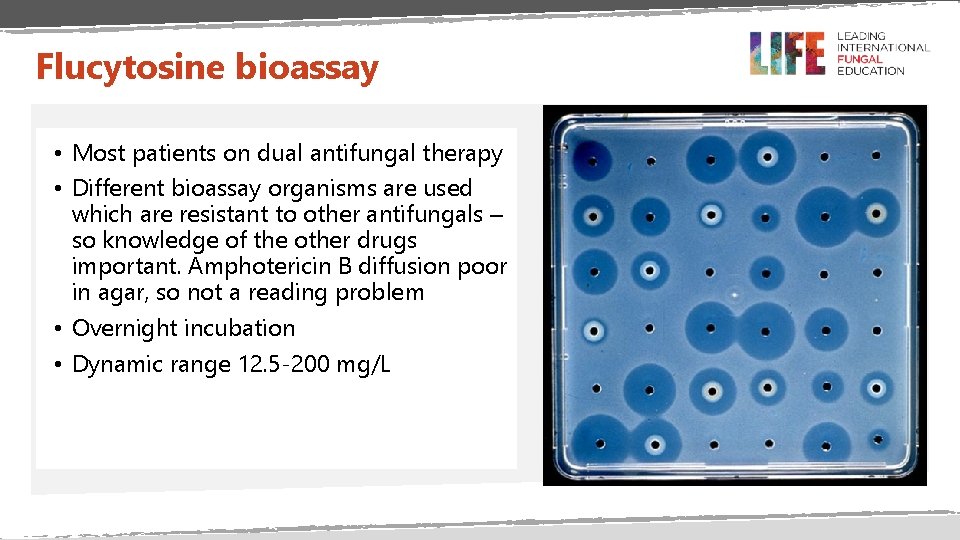
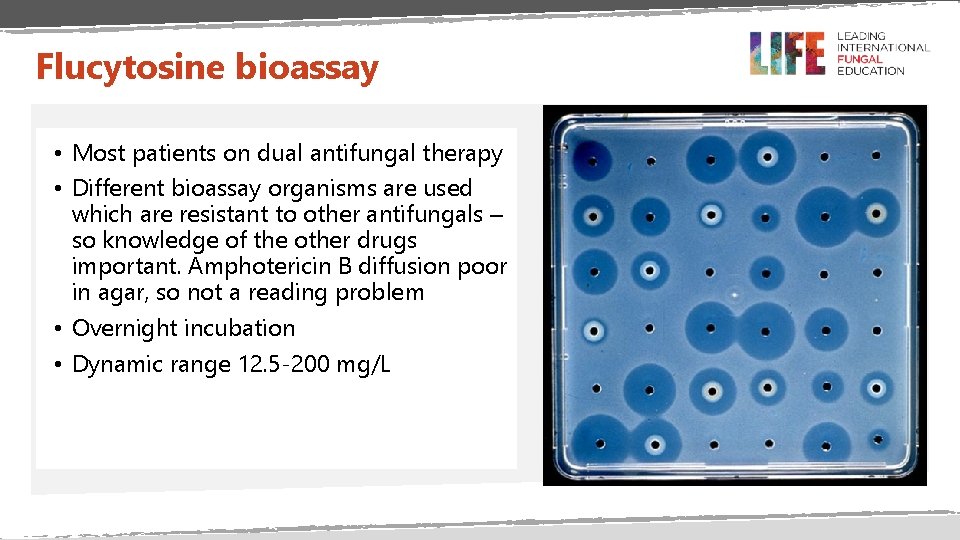
Flucytosine bioassay • Most patients on dual antifungal therapy • Different bioassay organisms are used which are resistant to other antifungals – so knowledge of the other drugs important. Amphotericin B diffusion poor in agar, so not a reading problem • Overnight incubation • Dynamic range 12. 5 -200 mg/L
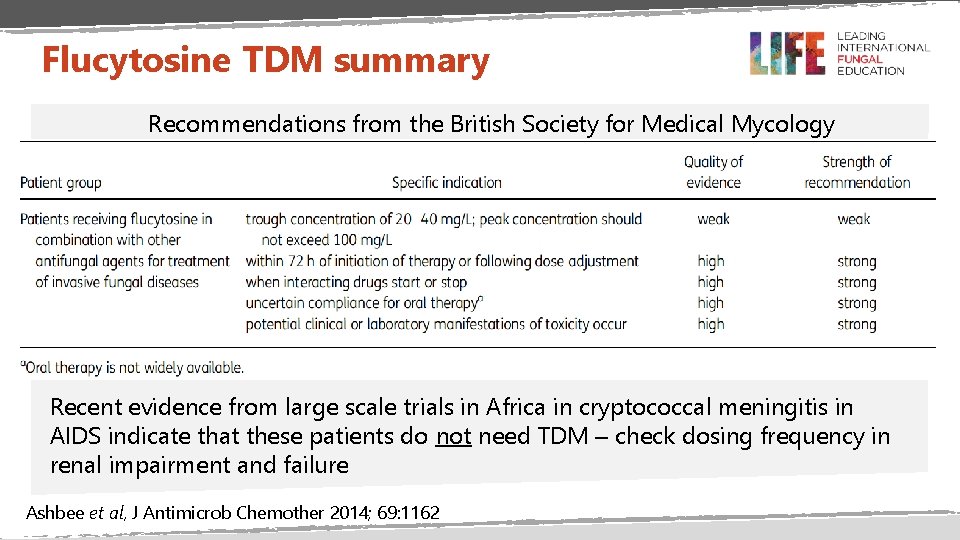
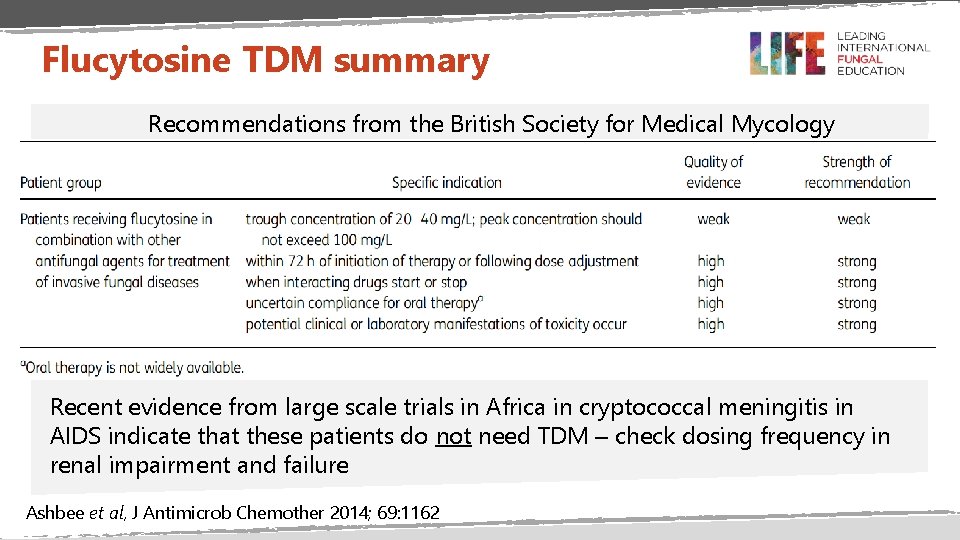
Flucytosine TDM summary Recommendations from the British Society for Medical Mycology Recent evidence from large scale trials in Africa in cryptococcal meningitis in AIDS indicate that these patients do not need TDM – check dosing frequency in renal impairment and failure Ashbee et al, J Antimicrob Chemother 2014; 69: 1162
Thank You
 Flucytosine mechanism of action
Flucytosine mechanism of action Flucytosine mechanism of action
Flucytosine mechanism of action Antifungal drugs classification
Antifungal drugs classification Mucormycosis
Mucormycosis Cl intracellular concentration
Cl intracellular concentration Lattice based access control example
Lattice based access control example Graham-denning model
Graham-denning model Stuffinspace
Stuffinspace When does her wonderful adventure begin?
When does her wonderful adventure begin? Graham denning model
Graham denning model Objectives of interpretation
Objectives of interpretation Nikki denning
Nikki denning Phil denning
Phil denning