Hypertonicity What is it and how should we
- Slides: 34
Hypertonicity What is it and how should we be managing it? Elishia Scobie Bach. App Sci (Physiotherapy) Grad. Dip. Neurological Rehabilitation
Content • What is hypertonicity? • What causes hypertonicity? • What is the impact of hypertonicity? • What motor disorders does the term hypertonicity include? • How to we assess hypertonicity? • What can be done to manage of hypertonicity?
Hypertonicity “ Greater than expected resistance to lengthening of a relaxed muscle” (Stolov 1966) • Hypertonicity is an umbrella term used to describe a group of motor disorders caused by an upper motor neurone lesion (UMNL) • • • Spasticity Clonus Tendon hyper-reflexia Flexor spasms Muscular co-contraction Dystonia Sheean & Mc. Guire 2009
Impact of hypertonicity on function • Impaired voluntary movement • Pain • Orthopaedic injury • Increased energy expenditure • Reduced quality of life • Poor hygiene • Increased burden of care (Lundstrom et al 2010) (Zorowitz et al 2013)
Spasticity “Spasticity is a disorder of the sensorimotor system characterized by a velocity-dependent increase in tonic stretch reflexes (‘muscle tone’) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflex, as one component of the upper motoneuron syndrome” Lance 1980
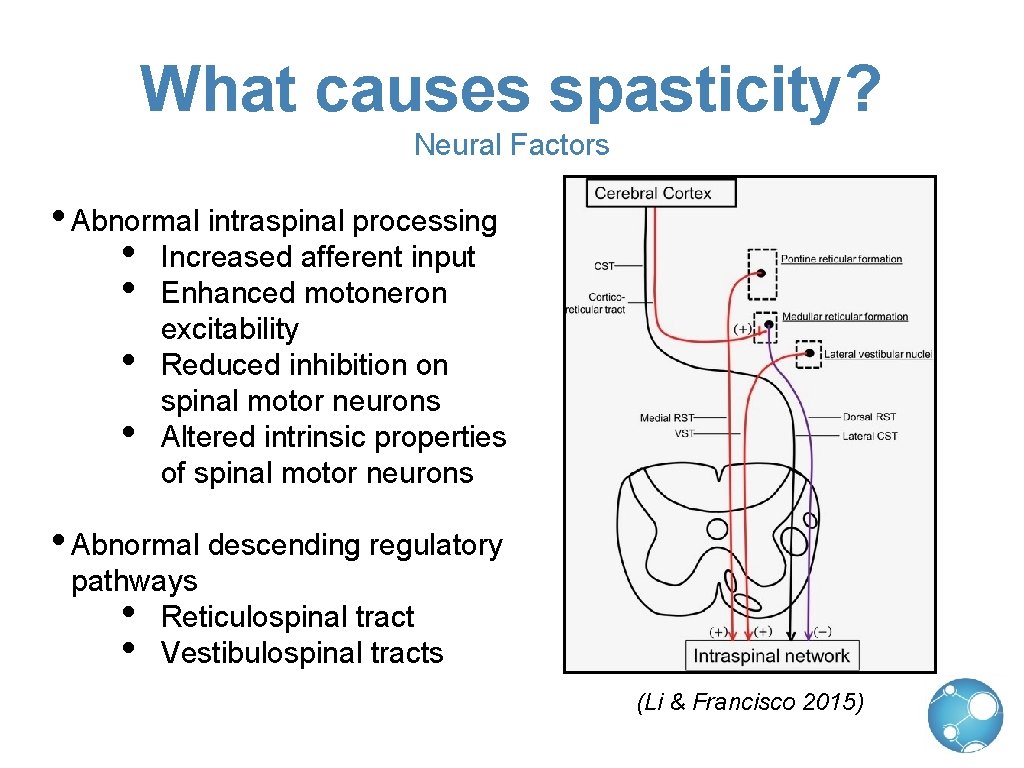
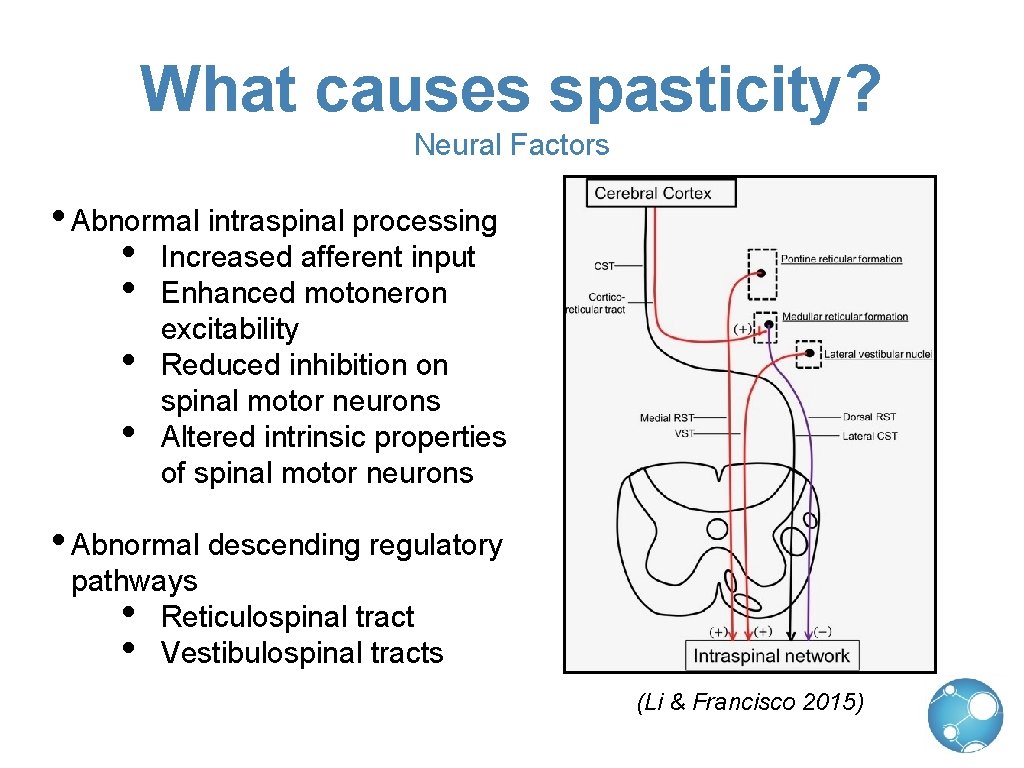
What causes spasticity? Neural Factors • Abnormal intraspinal processing • Increased afferent input • Enhanced motoneron • • excitability Reduced inhibition on spinal motor neurons Altered intrinsic properties of spinal motor neurons • Abnormal descending regulatory pathways • Reticulospinal tract • Vestibulospinal tracts (Li & Francisco 2015)
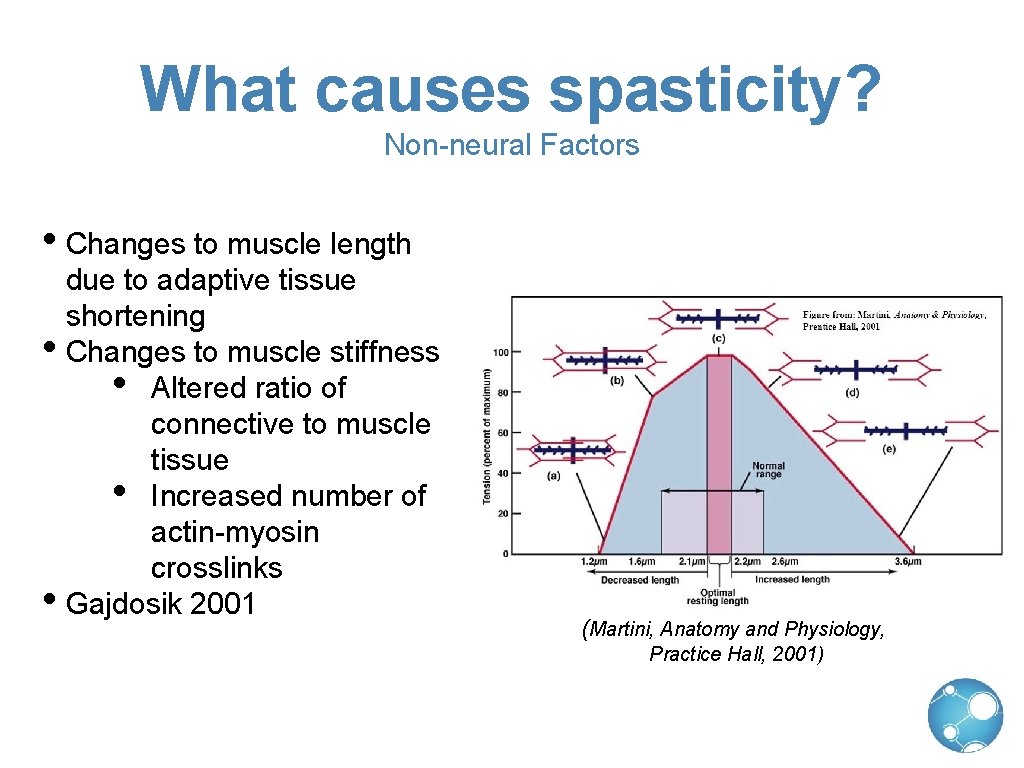
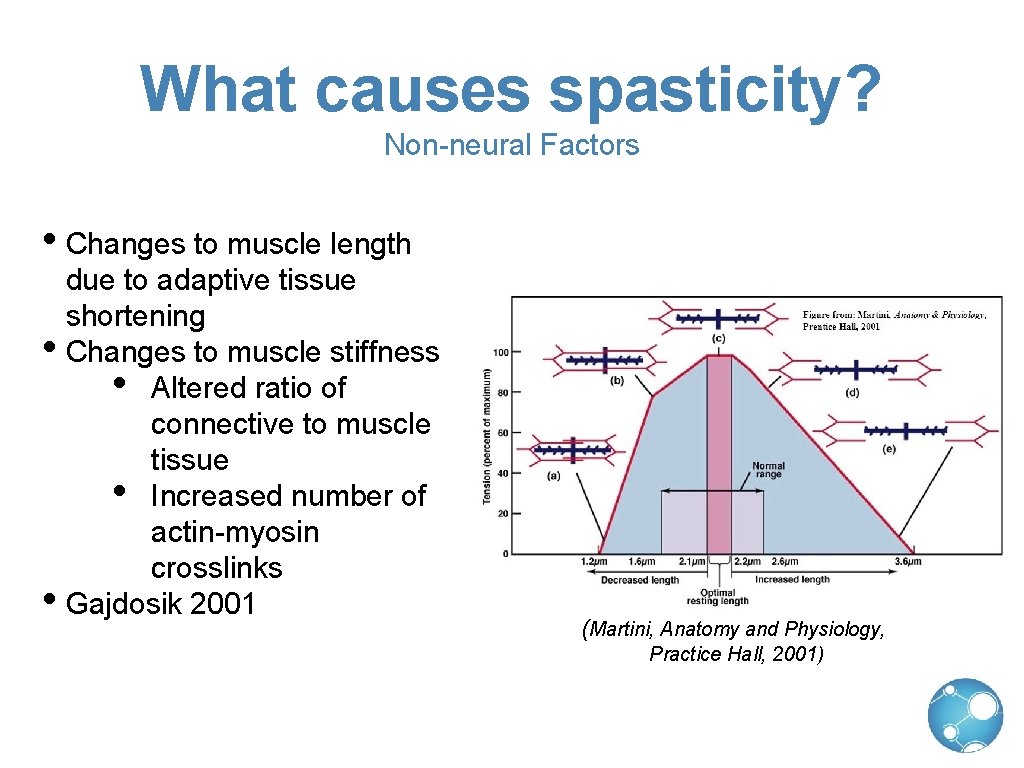
What causes spasticity? Non-neural Factors • Changes to muscle length due to adaptive tissue shortening • Changes to muscle stiffness • Altered ratio of connective to muscle tissue • Increased number of actin-myosin crosslinks • Gajdosik 2001 (Martini, Anatomy and Physiology, Practice Hall, 2001)
Dystonia “ a movement disorder characterized by sustained or intermittent muscle contractions causing abnormal, often repetitive, movements, postures, or both. Dystonic movements are typically patterned and twisting, and may be tremulous. ” Albanese et al (2013) • Dystonia is often initiated or worsened by voluntary action and associated with overflow muscle activation.
Dystonia • Dystonia is classified based on: • • Clinical characteristics • • age at onset, body distribution, temporal pattern associated features Etiology • • Nervous system pathology Genetic factors
Rigidity “velocity-independent bidirectional resistant to external imposed movement” Sanger et al (2003) Key component: • Resistance to movement at very low speeds • Bidirectional co-contraction of agonists and antagonists is • • present Absence of particular fixed posture Voluntary movement of distant muscle groups does not cause involuntary movement about the rigid joints https: //youtu. be/4 t. WPNan 12 -U
Clonus “A series of involuntary and rhythmic muscle contractions at a frequency of 5 -8 Hz which may occur in any muscle, caused by a permanent lesion in descending motor neurons” Suspected cause: • Hyperactive stretch reflexes • Rhythmical stimulation of lower motor neurons mediated by development of central pattern generators
Assessment of Hypertonicity
Assessment Outline • • Subjective Examination • Medical background • Previous treatment • Social situation • Function (PADL’s and DADL’s) • GOALS (function, pain, self-care, cosmetics) • Goal Attainment Scale • Patient Specific Functional Scale Objective Examination • Observation of resting posture • Quantification of pain • Active and passive range of motion • Muscle tone • Function • Qualitative assessment of function, participation, QOL
Resting Posture • Informally observe • What to look for? • • Sitting balance and endurance Fixed posturing Tonal activity during stress Presence of tremor Presence of dystonia Neglect Use of external aids and garments Footwear
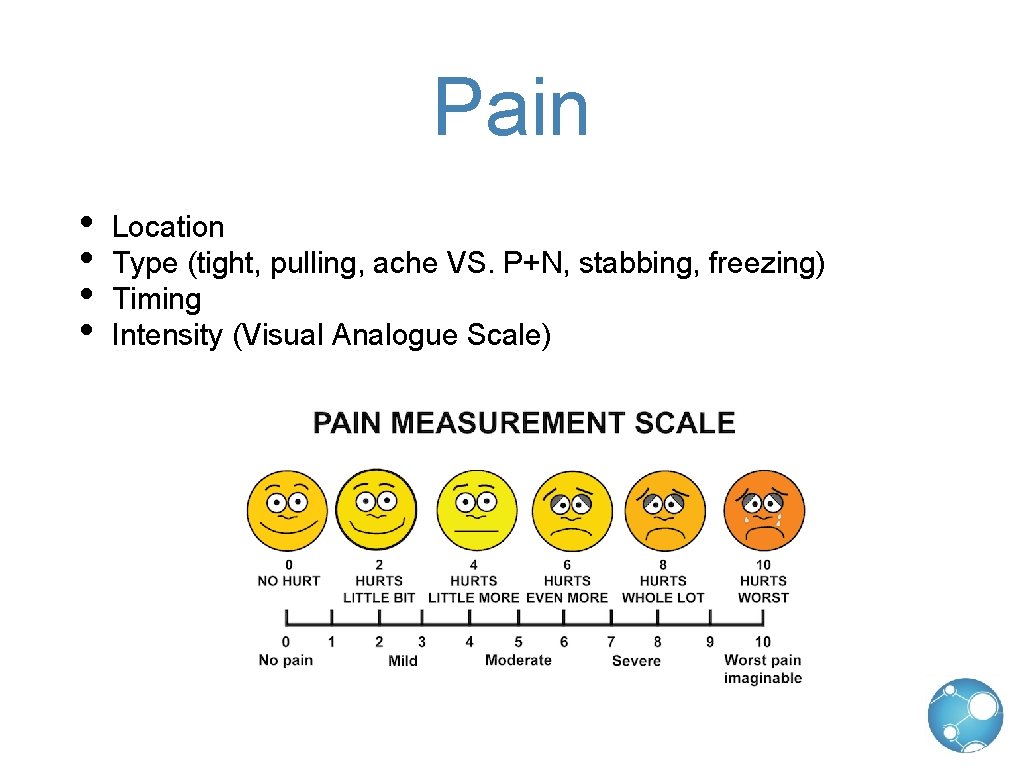
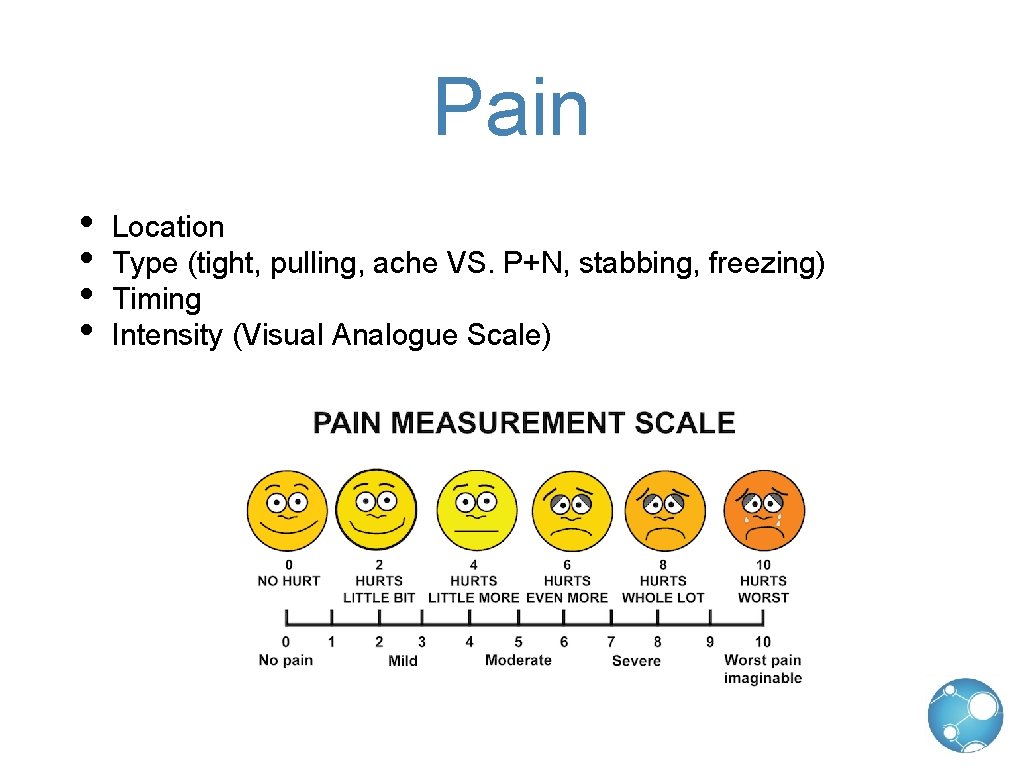
Pain • • Location Type (tight, pulling, ache VS. P+N, stabbing, freezing) Timing Intensity (Visual Analogue Scale)
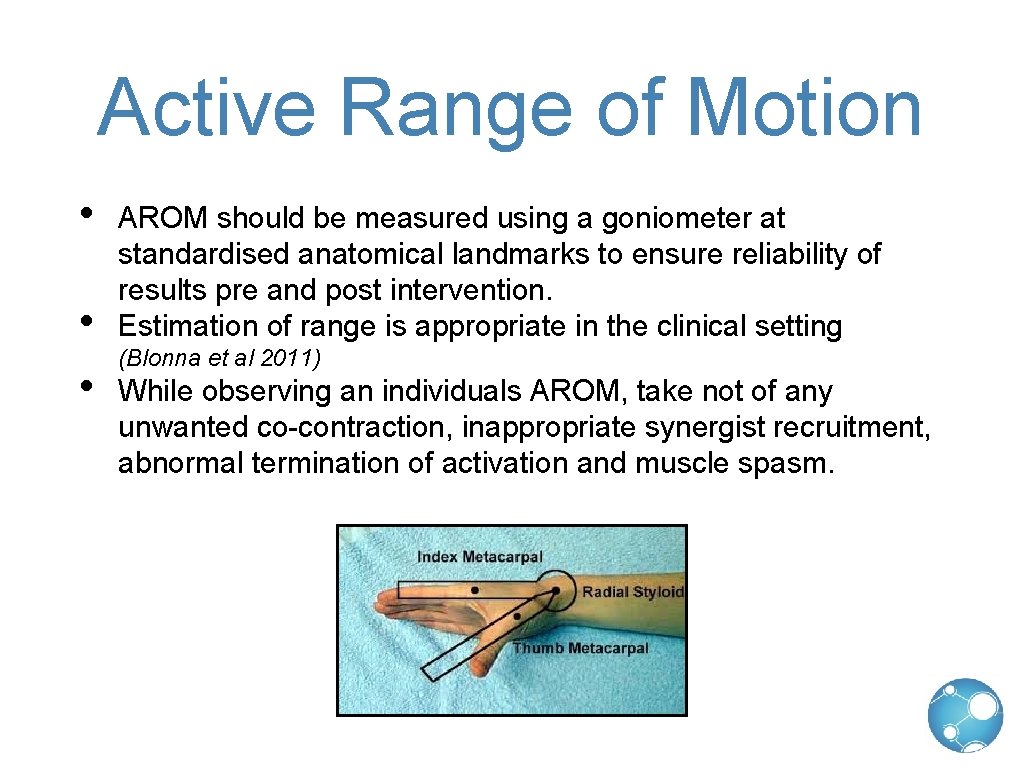
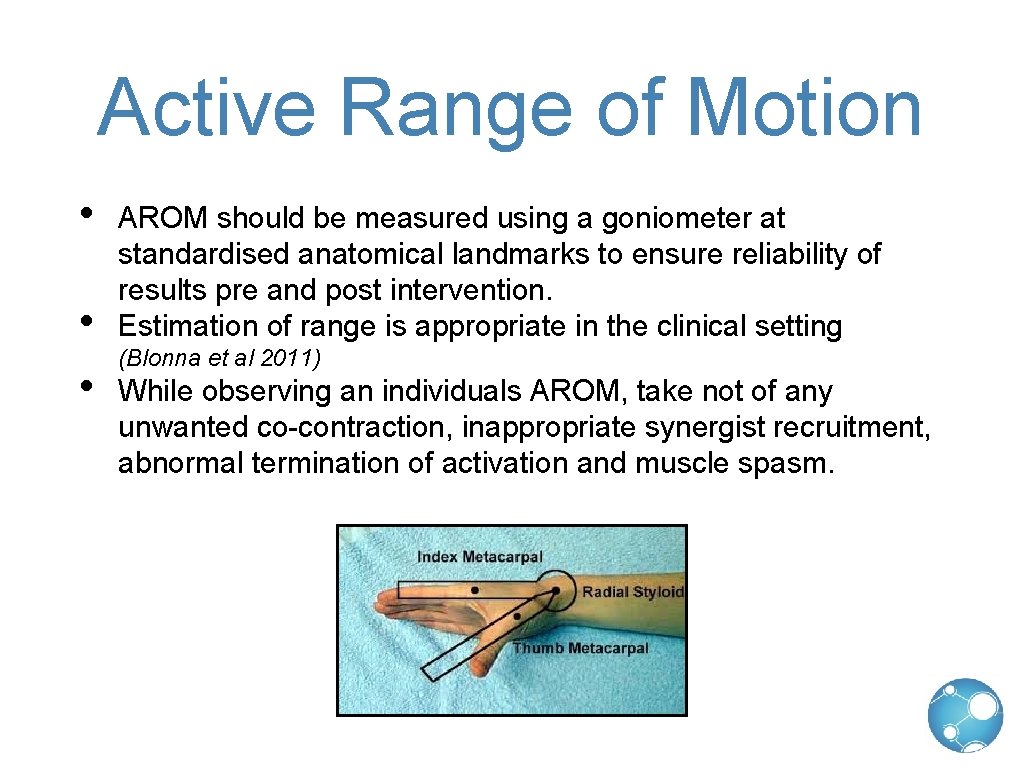
Active Range of Motion • • • AROM should be measured using a goniometer at standardised anatomical landmarks to ensure reliability of results pre and post intervention. Estimation of range is appropriate in the clinical setting (Blonna et al 2011) While observing an individuals AROM, take not of any unwanted co-contraction, inappropriate synergist recruitment, abnormal termination of activation and muscle spasm.
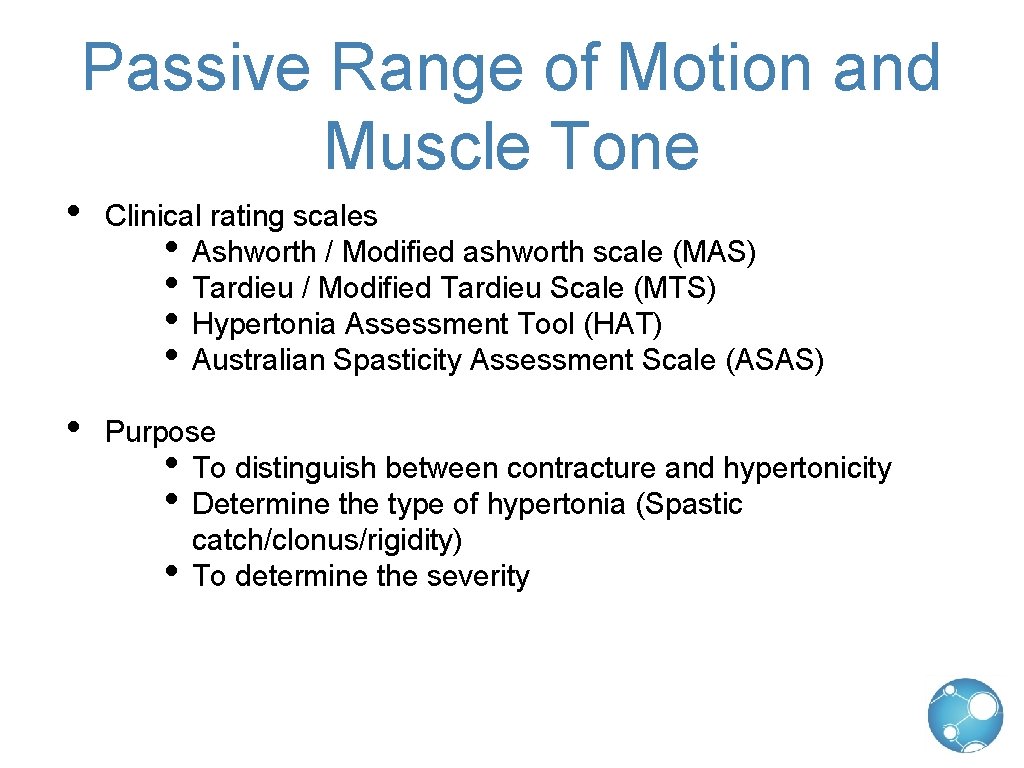
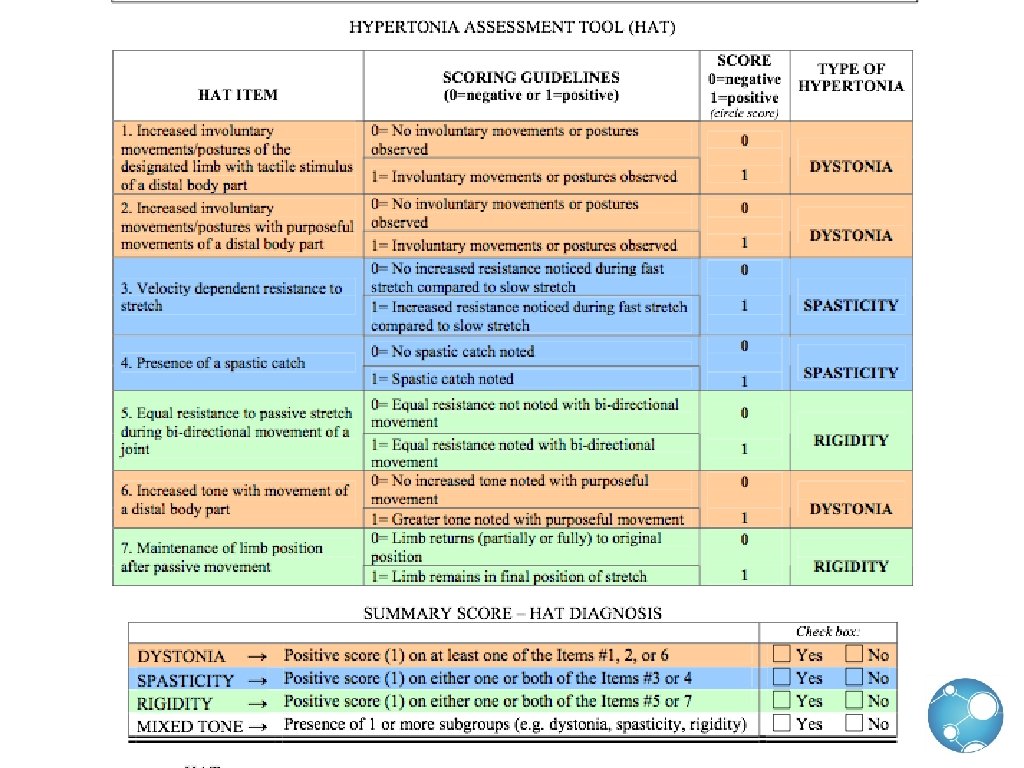
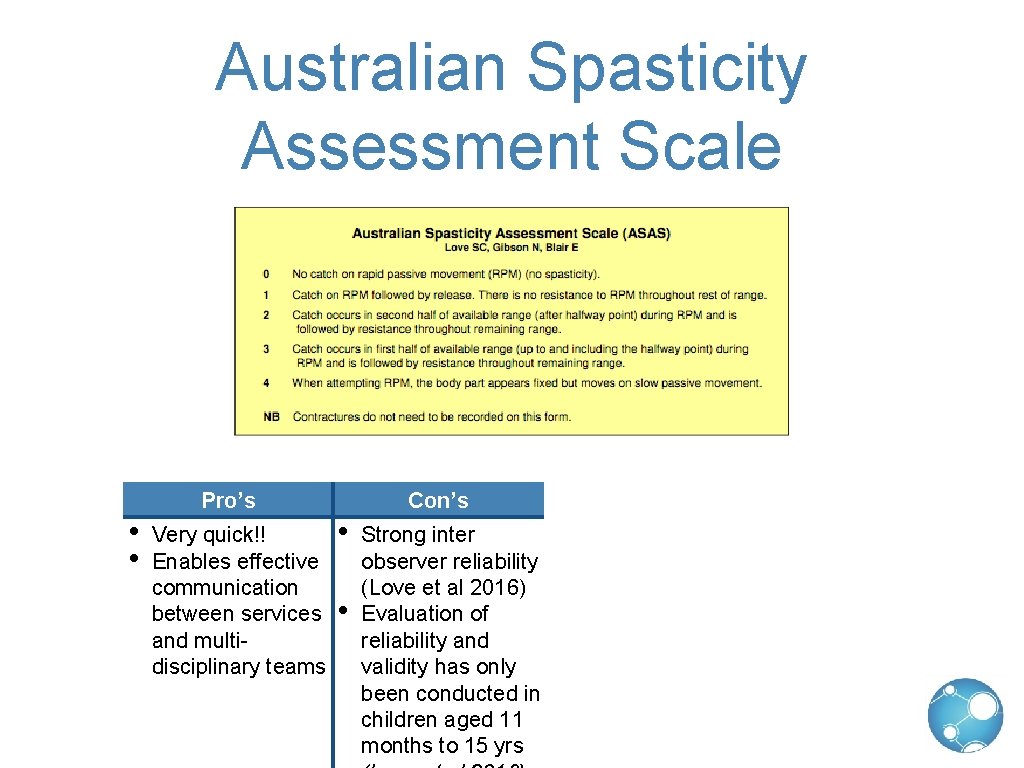
Passive Range of Motion and Muscle Tone • Clinical rating scales • Ashworth / Modified ashworth scale (MAS) • Tardieu / Modified Tardieu Scale (MTS) • Hypertonia Assessment Tool (HAT) • Australian Spasticity Assessment Scale (ASAS) • Purpose • To distinguish between contracture and hypertonicity • Determine the type of hypertonia (Spastic catch/clonus/rigidity) • To determine the severity
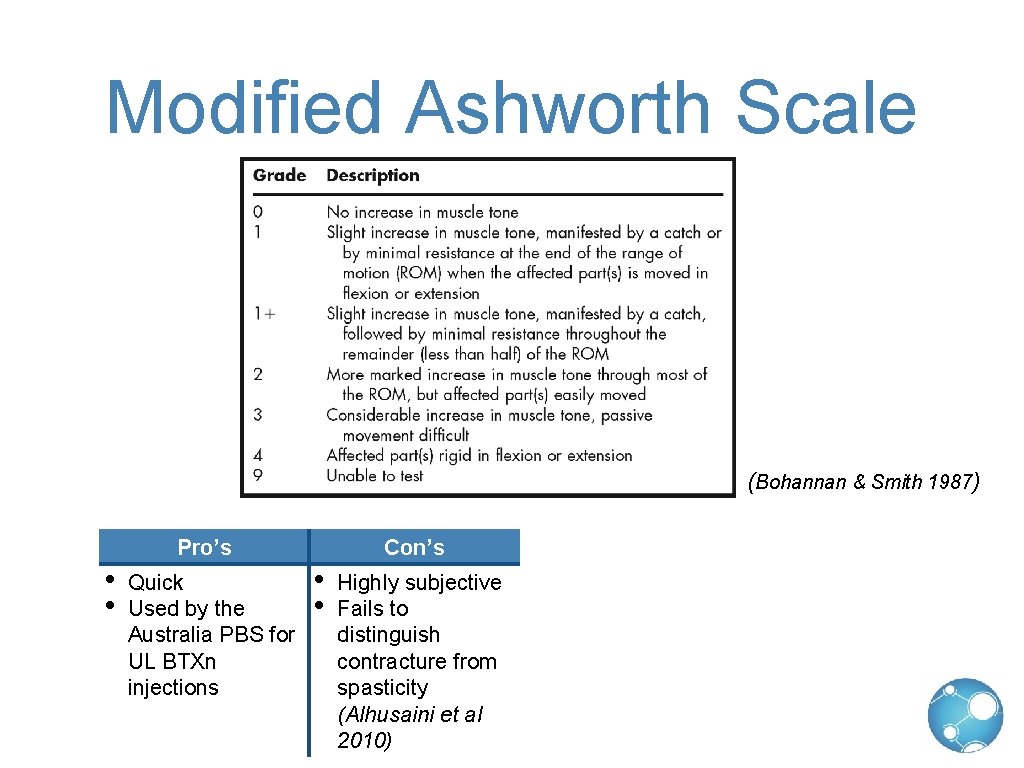
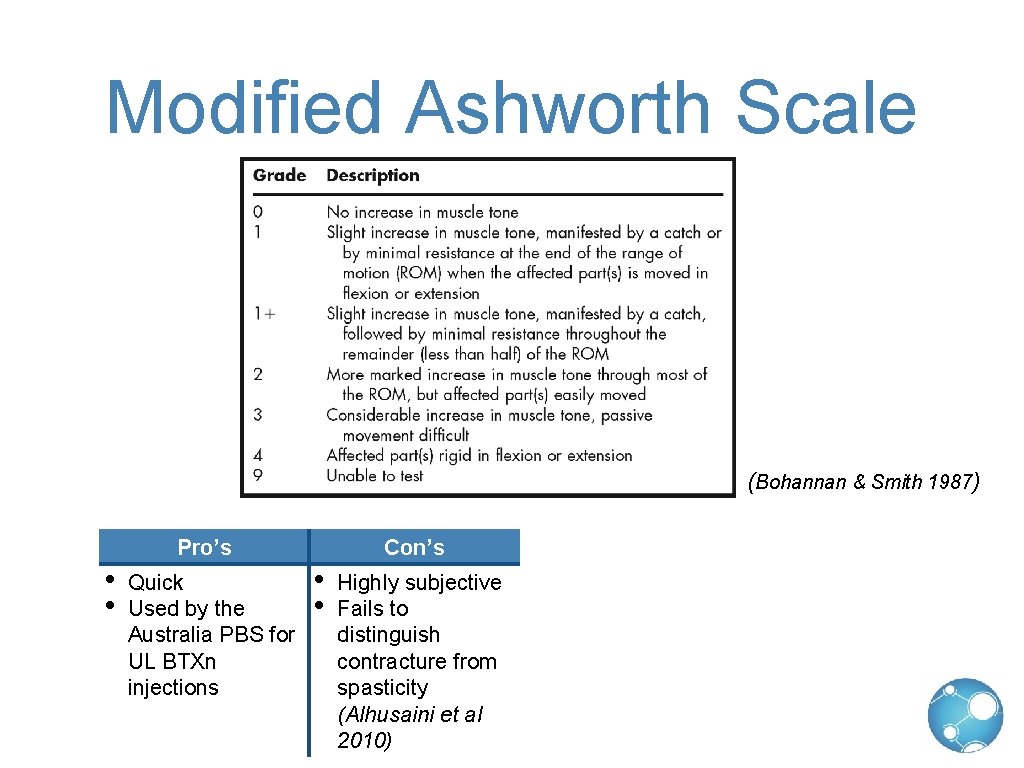
Modified Ashworth Scale (Bohannan & Smith 1987) Pro’s • • Quick Used by the Australia PBS for UL BTXn injections Con’s • • Highly subjective Fails to distinguish contracture from spasticity (Alhusaini et al 2010)
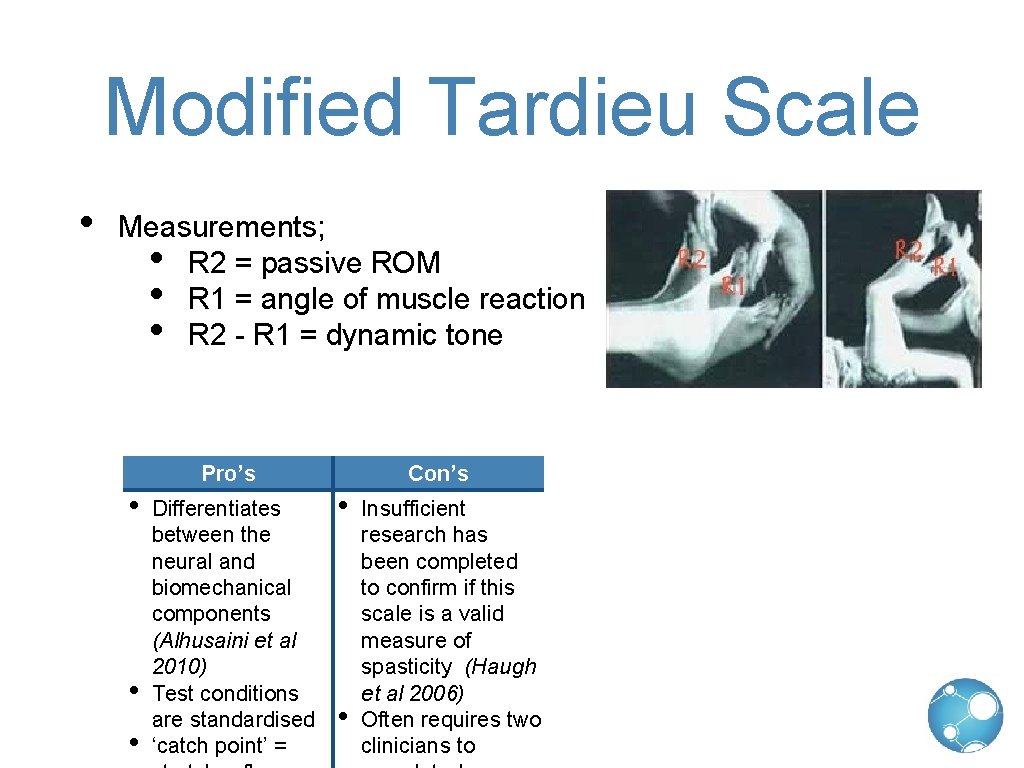
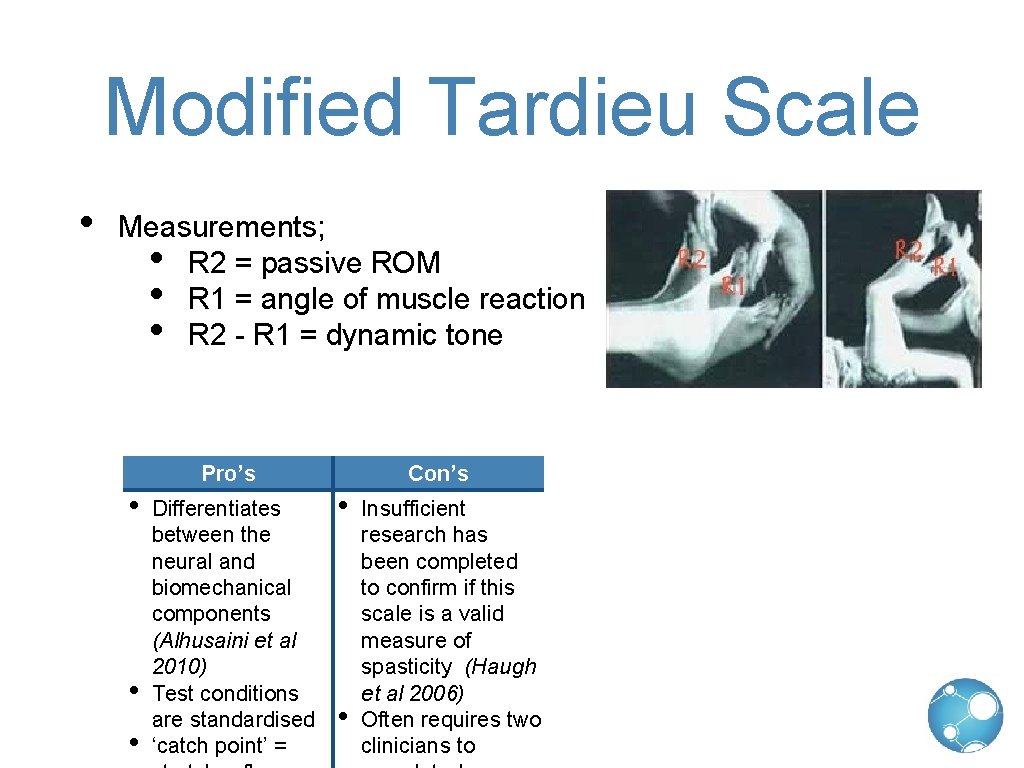
Modified Tardieu Scale • Measurements; • R 2 = passive ROM • R 1 = angle of muscle reaction • R 2 - R 1 = dynamic tone Pro’s • • • Differentiates between the neural and biomechanical components (Alhusaini et al 2010) Test conditions are standardised ‘catch point’ = Con’s • • Insufficient research has been completed to confirm if this scale is a valid measure of spasticity (Haugh et al 2006) Often requires two clinicians to
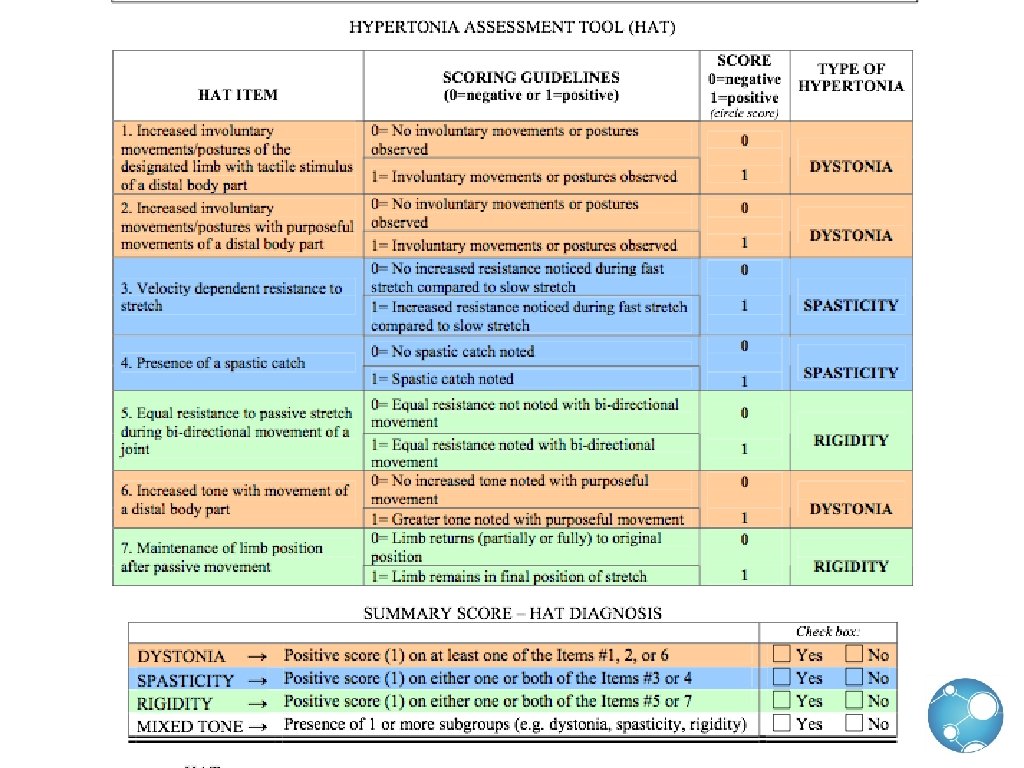
Hypertonia Assessment Tool Pro’s • • Allows differentiation between spasticity, dystonia and rigidity Only takes 5 minutes to complete Con’s • Evaluation of reliability and validity has only been conducted in children aged 419 yrs (Jethwa et al 2010) http: //research. hollandbloorview. ca/outcomemeasures/hatmanuals
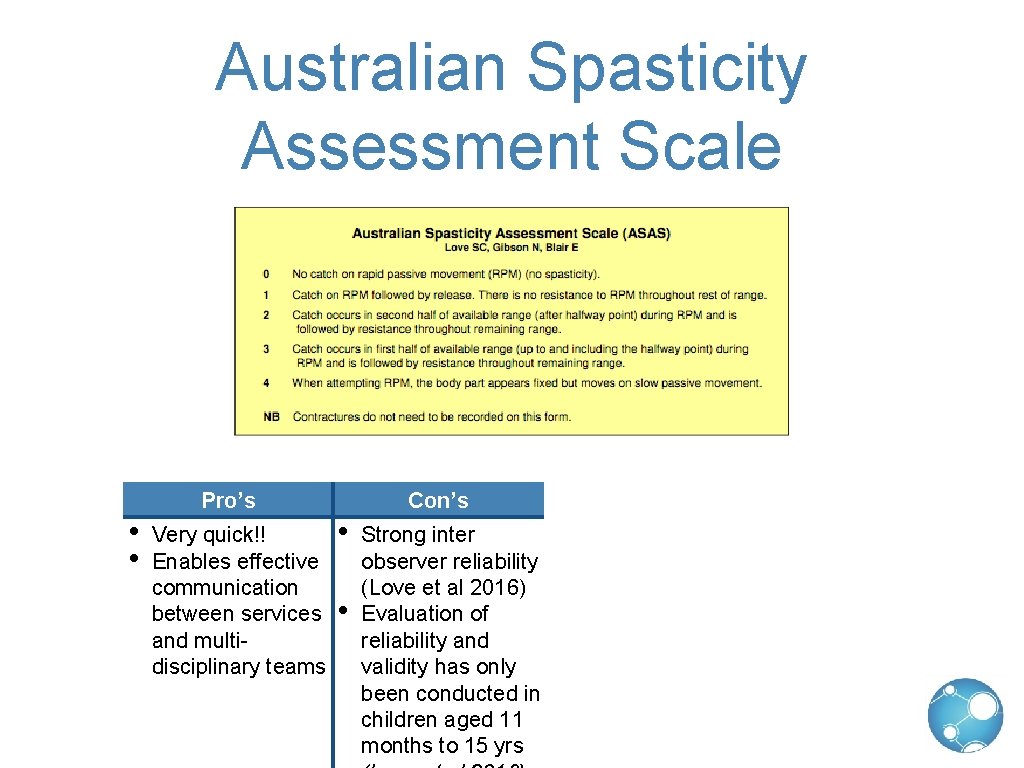
Australian Spasticity Assessment Scale Pro’s • • Very quick!! Enables effective communication between services and multidisciplinary teams Con’s • • Strong inter observer reliability (Love et al 2016) Evaluation of reliability and validity has only been conducted in children aged 11 months to 15 yrs
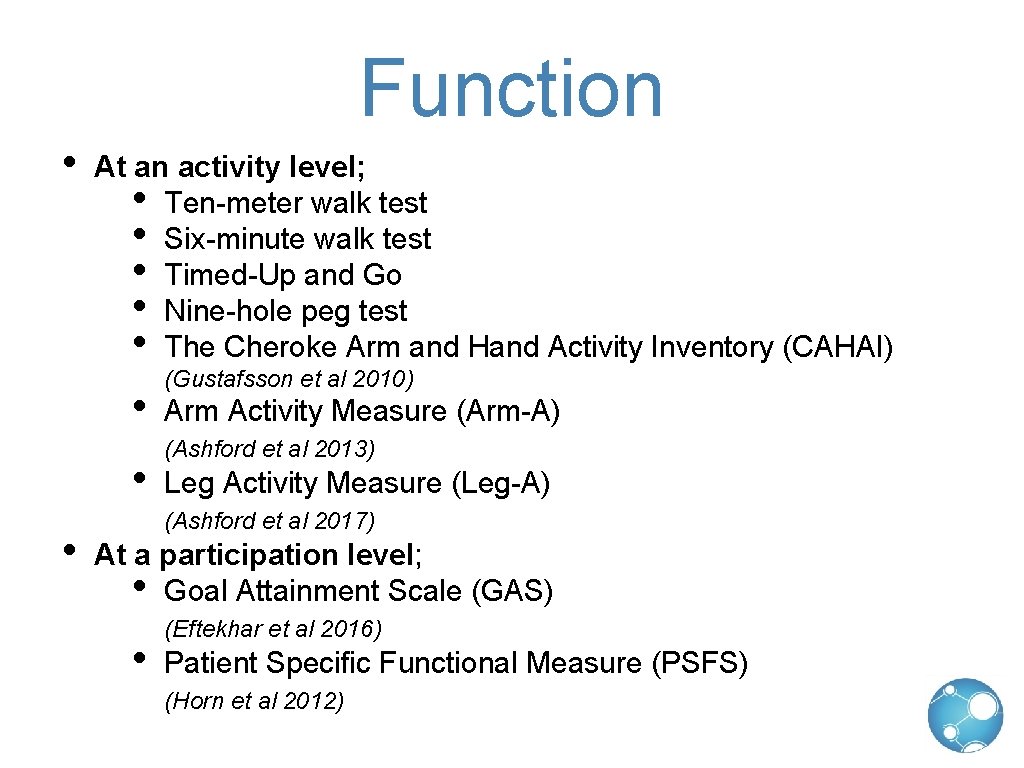
Function • At an activity level; • Ten-meter walk test • Six-minute walk test • Timed-Up and Go • Nine-hole peg test • The Cheroke Arm and Hand Activity Inventory (CAHAI) • • • (Gustafsson et al 2010) Arm Activity Measure (Arm-A) (Ashford et al 2013) Leg Activity Measure (Leg-A) (Ashford et al 2017) At a participation level; • Goal Attainment Scale (GAS) • (Eftekhar et al 2016) Patient Specific Functional Measure (PSFS) (Horn et al 2012)
Management of Hypertonicity
Management Menu • • • Educate the individual, their family/carer/other staff Prevention Stretching • • Splinting Serial Casting Neuromuscular electrical stimulation Functional retraining Medical management
Stretching ‘Regular stretch does not produce clinically important changes in joint mobility, pain, spasticity or activity limitation in patients with neurological conditions. ’ (Katalinic et al 2011) • What is the aim? • PREVENTION or CORRECTION • When using stretching to facilitate structural change it must be prolonged in nature, at end range to encourage adaptation. with increased sarcomere numbers
Splinting ‘ There is strong evidence that wearing a splint all night has no additional effect in reducing spasticity over usual therapy or in preventing contracture…’ Lannin & Ada (2011) Why splint? • Maintain joint integrity • Promote mechanical advantage • Reduce pain
Serial Casting ‘The process of applying and removing corrective plaster to increase the extensibility of soft tissue around a joint. ’ (Cusick 1990) ‘Grade B recommendation could be given for the use of casting to increase passive range of motion or to prevent its loss. ’ (Mortensen & Eng 2003)
Neuromuscular Electrical Stimulation • The use of NMES has been shown to improve motor recovery post UMNL (Lin & Yan 2011) • Application in hypertonicity: • Stimulate weak antagonist muscle groups • Induce reciprocal inhibition • Induce plastic effects within spinal cord pathways to • temporarily reduce spasticity (Motta-Oishi el al 2013) Encourages the uptake of BTXn when used in the first 2 -3 days (Olver et al 2010)
Functional Retraining • • Key elements; • Task-specific • Control vs strength • Attainable • Specificity to goal Bayona et al (2005)
Medical Management • Medical management options; A. Systemic Pharmacology • • Oral muscle relaxants of antispasmodics Baclofen pump B. Focal Pharmacology • • Chemodenervation Neurolysis “Medication should rarely be used in isolation but is usually C. Surgical • Tenotomy part of a whole treatment strategy” (Barnes, 2008)
Summary • Hypertonicity is an umbrella term • Neural and non-neural factors need to be assessed • Treatment should be designed by a MDT • Treatment involves the coordination of multiple interventions • Treatment must be goal driven • Hypertonicity is life long
References • ALHUSAINI, A. A. , DEAN, C. M. , CROSBIE, J. , SHEPHERD, R. B. & LEWIS, J. 2010. Evaluation of spasticity in children with cerebral palsy using Ashworth and Tardieu Scales compared with laboratory measures. J Child Neurol, 25, 1242 -7. • ASHFORD, S. , JACKSON, D. , MAHAFFEY, P. , VANDERSTAY, R. & TURNER-STOKES, L. 2017. Conceptualization and Development of the Leg Activity Measure (Leg. A) for Patient and Carer Reported Assessment of Activity in the Paretic Leg. Physiother Res Int, 22. • ASHFORD, S. , SLADE, M. & TURNER-STOKES, L. 2013. Conceptualisation and development of the arm activity measure (Arm. A) for assessment of activity in the hemiparetic arm. Disability and Rehabilitation, 35, 1513 -1518. • BAYONA, N. A. , BITENSKY, J. , SALTER, K. & TEASELL, R. 2005. The Role of Task-Specific Training in Rehabilitation Therapies. Topics in Stroke Rehabilitation, 12, 58 -65. • BARNES, M. P. , BEST, D. , KIDD, L. , ROBERTS, B. , STARK, S. , WEEKS, P. & WHITAKER, J. 2005. The use of botulinum toxin type-B in the treatment of patients who have become unresponsive to botulinum toxin type-A – initial experiences. European Journal of Neurology, 12, 947 -955. • BLONNA, D. , ZARKADAS, P. C. , FITZSIMMONS, J. S. & O'DRISCOLL, S. W. 2012. Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Surg Sports Traumatol Arthrosc, 20, 1378 -85. • BOHANNON, R. W. & SMITH, M. B. 1987. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther, 67, 206 -7. • BOYD, R. N. & GRAHAM, H. K. 1999. Objective measurement of clinical findings in the use of botulinum toxin type A for the management of children with cerebral palsy. European Journal of Neurology, 6, s 23 -s 35. • BOYRAZ, I. , UYSAL, H. , KOC, B. & SARMAN, H. 2015. Clonus: definition, mechanism, treatment. Med Glas (Zenica), 12, 19 -26. • EFTEKHAR, P. , MOCHIZUKI, G. , DUTTA, T. , RICHARDSON, D. & BROOKS, D. 2016. Goal Attainment Scaling in Individuals with Upper Limb Spasticity Post Stroke. Occupational Therapy International, 23, 379 -389. • FOSANG, A. L. , GALEA, M. P. , MCCOY, A. T. , REDDIHOUGH, D. S. & STORY, I. 2003. Measures of muscle and joint performance in the lower limb of children with cerebral palsy. Dev Med Child Neurol, 45, 664 -70. • GRACIES, J. M. , MAROSSZEKY, J. E. , RENTON, R. , SANDANAM, J. , GANDEVIA, S. C. & BURKE, D. 2000. Short-term effects of dynamic lycra splints on upper limb in hemiplegic patients. Arch Phys Med Rehabil, 81, 1547 -55. • GUSTAFSSON, L. A. , TURPIN, M. J. & DORMAN, C. M. 2010. Clinical Utility of the Chedoke Arm and Hand Activity Inventory for Stroke Rehabilitation. Canadian Journal of Occupational Therapy, 77, 167 -173. • HAUGH, A. B. , PANDYAN, A. D. & JOHNSON, G. R. 2006. A systematic review of the Tardieu Scale for the measurement of spasticity. Disabil Rehabil, 28, 899 -907. • HORN, K. K. , JENNINGS, S. , RICHARDSON, G. , VLIET, D. V. , HEFFORD, C. & ABBOTT, J. H. 2012. The Patient-Specific Functional Scale: Psychometrics, Clinimetrics, and Application as a Clinical Outcome Measure. Journal of Orthopaedic & Sports Physical Therapy, 42, 30 -D 17.
References • • • ` • • • JETHWA, A. , MINK, J. , MACARTHUR, C. , KNIGHTS, S. , FEHLINGS, T. & FEHLINGS, D. 2010. Development of the Hypertonia Assessment Tool (HAT): a discriminative tool for hypertonia in children. Dev Med Child Neurol, 52, e 83 -7. LANNIN, N. A. & ADA, L. 2011. Neurorehabilitation splinting: theory and principles of clinical use. Neuro. Rehabilitation, 28, 21 -8. LI, S. & FRANCISCO, G. E. 2015. New insights into the pathophysiology of post-stroke spasticity. Frontiers in Human Neuroscience, 9. LIN, Z. & YAN, T. 2011. Long-term effectiveness of neuromuscular electrical stimulation for promoting motor recovery of the upper extremity after stroke. J Rehabil Med, 43, 506 -10. LOVE, S. , GIBSON, N. , SMITH, N. , BEAR, N. & BLAIR, E. 2016. Interobserver reliability of the Australian Spasticity Assessment Scale (ASAS). Dev Med Child Neurol, 58 Suppl 2, 18 -24. LOVE, S. C. , NOVAK, I. , KENTISH, M. , DESLOOVERE, K. , HEINEN, F. , MOLENAERS, G. , O'FLAHERTY, S. & GRAHAM, H. K. 2010. Botulinum toxin assessment, intervention and after-care for lower limb spasticity in children with cerebral palsy: international consensus statement. Eur J Neurol, 17 Suppl 2, 9 -37. LUNDSTROM, E. , SMITS, A. , BORG, J. & TERENT, A. 2010. Four-fold increase in direct costs of stroke survivors with spasticity compared with stroke survivors without spasticity: the first year after the event. Stroke, 41, 319 -24. MORTENSON, P. A. & ENG, J. J. 2003. The use of casts in the management of joint mobility and hypertonia following brain injury in adults: a systematic review. Phys Ther, 83, 648 -58. MOTTA-OISHI, A. A. , MAGALHAES, F. H. & MICOLIS DE AZEVEDO, F. 2013. Neuromuscular electrical stimulation for stroke rehabilitation: is spinal plasticity a possible mechanism associated with diminished spasticity? Med Hypotheses, 81, 784 -8. OLVER, J. , ESQUENAZI, A. , FUNG, V. S. , SINGER, B. J. & WARD, A. B. 2010. Botulinum toxin assessment, intervention and aftercare for lower limb disorders of movement and muscle tone in adults: international consensus statement. Eur J Neurol, 17 Suppl 2, 57 -73. SANGER, T. D. , DELGADO, M. R. , GAEBLER-SPIRA, D. , HALLETT, M. & MINK, J. W. 2003. Classification and definition of disorders causing hypertonia in childhood. Pediatrics, 111, e 89 -97. SHEEAN, G. & MCGUIRE, J. R. 2009. Spastic Hypertonia and Movement Disorders: Pathophysiology, Clinical Presentation, and Quantification. PM&R, 1, 827 -833. SHEEAN, G. , LANNIN, N. A. , TURNER-STOKES, L. , RAWICKI, B. & SNOW, B. J. 2010. Botulinum toxin assessment, intervention and after-care for upper limb hypertonicity in adults: international consensus statement. Eur J Neurol, 17 Suppl 2, 74 -93. STOLOV, W. C. 1966. The concept of normal muscle tone, hypotonia and hypertonia. Arch Phys Med Rehabil, 47, 156 -68. ZOROWITZ, R. D. , GILLARD, P. J. & BRAININ, M. 2013. Poststroke spasticity: Sequelae and burden on stroke survivors and caregivers. Neurology, 80, S 45 -S 52.