Healthcare Leadership Course Patient and Family Centered Care

- Slides: 14
Healthcare Leadership Course: Patient and Family Centered Care Power. Point INTRODUCTION TO PATIENT AND FAMILY CENTERED CARE BY KEVIN BLACKMAN RN BSCN
Highlights After completing this lesson, you will be able to: 1. Explain the definition and goals of patient- and family-centered care. 2. Describe the experience of being a patient, based on first-hand experience or close attention to the experience of a friend or family member. 3. Explain the reasons for the increasing focus on patient- and family-centered care, particularly its relation to improved health outcomes.
Section 1: History HISTORY Now, there are many definitions of “patient-centered care. ” References to “patient-centered care” date to the 1950 s, and the concept of “patient-centered medicine” was introduced by Balint and colleagues in 1970. In June of 2006 a one-day invitational meeting was convened by the Institute for Family-Centered Care (IFCC) in collaboration with the Institute for Healthcare Improvement (IHI), which helped to better define the meaning of “Patient and Family Centered care. In preparation for the meeting, each participant received a copy of a background paper titled, “partnering with Patients and Families to Design a Patient- and Family-Centered Health Care System: A Roadmap for the Future. ” This document defined Patient and Family Centered care, “as an approach to the planning, delivery, and evaluation of health care that is grounded in mutually beneficial partnerships among health care providers, patients, and families (Partnering with Patients and Families to Design a Patient and Family-Centered Health Care System, 2008). ”
Definitions and Goals � � “The American Academy of Family Physicians defines family as “a group of individuals with a continuing legal, genetic and/or emotional relationship. ” This includes, “close friends or significant others. ” This right is important to various pieces of the care process, such as when healthcare workers are visiting with their patients, or patients are participating in the decision-making process. What exactly is meant by “patient- and family-centered care, ” and why should you care about it? In this lesson, you’ll think in a new way about what it’s like to be a patient in today’s health care system. You’ll begin to examine the differences – in assumptions and in practice – between patient-centered care and provider-centered care, and you will learn that providing patient- and family-centered care is an essential component of safe, reliable care. Since the 1980 s, multiple definitions of “patient-centered care” and "patient- and family-centered care" have evolved. In partnership with patients, families, health care leaders, and researchers, the Institute for Patient- and Family-Centered Care (IPFCC), a leading organization in the field, defined patient- and family-centered care as “an approach to the planning, delivery, and evaluation of health care that is grounded in mutually beneficial partnerships among health care providers, patients, and families (Partnering with Patients and Families to Design a Patient and Family. Centered Health Care System, 2008). ” They further identified Patient and Family-Centered Care, as having the following core concepts: CONCEPTS: � Dignity and Respect. Health care practitioners listen to and honor patient and family perspectives and choices. Patient and family knowledge, values, beliefs, and cultural backgrounds are incorporated into the planning and delivery of care. � Information Sharing. Health care practitioners communicate and share complete and unbiased information with patients and families in ways that are affirming and useful. Patients and families receive timely, complete, and accurate information in order to effectively participate in care and decision-making. � Participation. Patients and families are encouraged and supported in participating in care and decisionmaking at the level they choose. � Collaboration. Patients, families, health care practitioners, and health care leaders collaborate in policy and program development, implementation, and evaluation; in facility design; and in professional education, as well as in the delivery of care.
Definitions and Goals (Cont) The Institute for Patient- and Family-Centered Care (IPFCC), a leading organization in the field, defined patient - and family-centered care as: � Dignity and Respect. Health care practitioners listen to and honor patient and family perspectives and choices. Patient and family knowledge, values, beliefs, and cultural backgrounds are incorporated into the planning and delivery of care. � Information Sharing. Health care practitioners communicate and share complete and unbiased information with patients and families in ways that are affirming and useful. Patients and families receive timely, complete, and accurate information in order to effectively participate in care and decision-making. � Participation. Patients and families are encouraged and supported in participating in care and decision-making at the level they choose. � Collaboration. Patients, families, health care practitioners, and health care leaders collaborate in policy and program development, implementation, and evaluation; in facility design; and in professional education, as well as in the delivery of care. � The Children’s Hospital of Philadelphia built on this definition, tailoring it to the priorities of its organization. It defines patient- and family-centered care as a series of values or principles: � Dignity and Respect. We listen to and honor patient and family perspectives and choices. We incorporate patient and family knowledge, values, beliefs, and cultural background into care planning and delivery. � Information Sharing. We communicate and share complete and unbiased information with patients and families in affirming and useful ways. Patients and families receive timely and accurate information so they may effectively participate in care and decision-making. � Participation. We encourage patients and families to participate in care and decision-making at the level they choose. � Collaboration. We invite patients and family members to work with our care providers and hospital leaders on policy and program development, execution, and evaluation; in health care facility design; and in professional education and care delivery. � Access. The care we provide is equitable and flexible, and is delivered as efficiently and timely as possible. � Care Coordination. We focus on the coordination of patient care and patient and family needs. Our health care teams are trained, and our systems are designed, to support transition, integration, and continuity of care. Emphasis is placed on continuous healing relationships.
THREE MAXIMS TO PFCC �DON BERICK’S THREE MAXIMS OF PATIENT AND FAMILY CENTERED CARE INCLUDE: �(1) ‘The needs of the patient come first. �(2) ‘Nothing about me without me. �(3) ‘Every patient is the only patient. ’
Definitions and Goals (Cont) � SECTION 2: EXPERIENCES � Every one of us has a story about being a patient. Maybe it’s the simple story of your last doctor’s appointment – or maybe it’s the story of your mother, your father, a loved one, a friend, or family member. We invite you to tell your story here. How were you (or your friend, or your family member) treated? How did it feel to be a patient – or to see your friend or loved one being a patient? What would you like to say to the people who were caring for you (or for your friend or family member)? � In 2001, Cincinnati Children’s Hospital was trying to improve outcomes for patients at its Cystic Fibrosis (CF) Center. In a very unusual step, the hospital met with parents, shared the data on the center’s performance, and asked them to weigh in on what the hospital could do better. Parents welcomed the invitation, and soon they were contributing to the design of care in real, tangible ways. � WATCH VIDEO AND THINK Video: Pursuing Perfection in Health Care Involving Patients � https: //www. youtube. com/watch? v=vm. TIPIi. As.
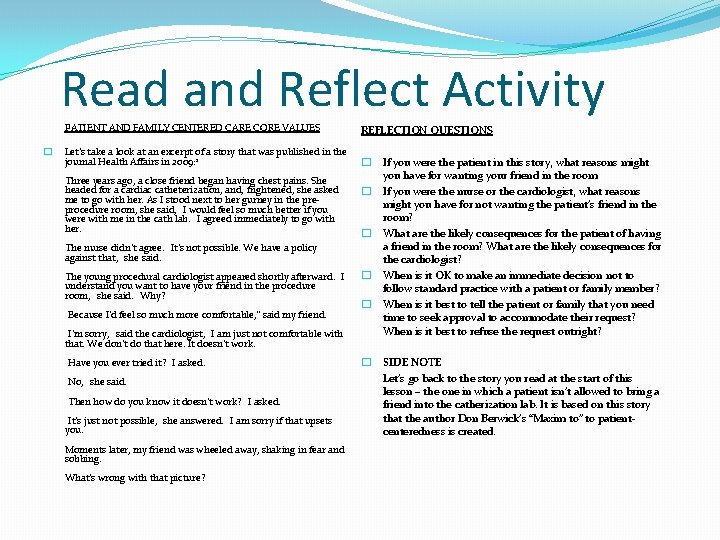
Read and Reflect Activity PATIENT AND FAMILY CENTERED CARE CORE VALUES � Let’s take a look at an excerpt of a story that was published in the journal Health Affairs in 2009: 1 Three years ago, a close friend began having chest pains. She headed for a cardiac catheterization, and, frightened, she asked me to go with her. As I stood next to her gurney in the preprocedure room, she said, "I would feel so much better if you were with me in the cath lab. " I agreed immediately to go with her. The nurse didn’t agree. "It’s not possible. We have a policy against that, " she said. The young procedural cardiologist appeared shortly afterward. "I understand you want to have your friend in the procedure room, " she said. "Why? " "Because I’d feel so much more comfortable, ” said my friend. "I’m sorry, " said the cardiologist, "I am just not comfortable with that. We don’t do that here. It doesn’t work. " "Have you ever tried it? " I asked. "No, " she said. "Then how do you know it doesn’t work? " I asked. "It’s just not possible, " she answered. "I am sorry if that upsets you. " Moments later, my friend was wheeled away, shaking in fear and sobbing. What’s wrong with that picture? REFLECTION QUESTIONS � If you were the patient in this story, what reasons might you have for wanting your friend in the room � If you were the nurse or the cardiologist, what reasons might you have for not wanting the patient’s friend in the room? � What are the likely consequences for the patient of having a friend in the room? What are the likely consequences for the cardiologist? � When is it OK to make an immediate decision not to follow standard practice with a patient or family member? � When is it best to tell the patient or family that you need time to seek approval to accommodate their request? When is it best to refuse the request outright? � SIDE NOTE Let’s go back to the story you read at the start of this lesson – the one in which a patient isn’t allowed to bring a friend into the catherization lab. It is based on this story that the author Don Berwick’s “Maxim to” to patientcenteredness is created.
Section 3: Reasons to Increase Focus � VIDEO: Patient- and Family-Centered Care: Why it Matters and How to Practice It � https: //www. youtube. com/watch? v=7 g-5 I 7 DO 1 r. Q
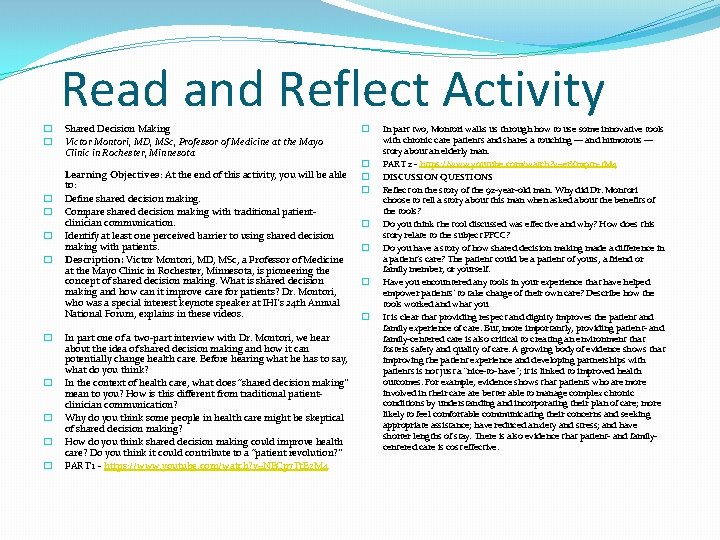
Read and Reflect Activity � � � Shared Decision Making Victor Montori, MD, MSc, Professor of Medicine at the Mayo Clinic in Rochester, Minnesota Learning Objectives: At the end of this activity, you will be able to: Define shared decision making. Compare shared decision making with traditional patientclinician communication. Identify at least one perceived barrier to using shared decision making with patients. Description: Victor Montori, MD, MSc, a Professor of Medicine at the Mayo Clinic in Rochester, Minnesota, is pioneering the concept of shared decision making. What is shared decision making and how can it improve care for patients? Dr. Montori, who was a special interest keynote speaker at IHI’s 24 th Annual National Forum, explains in these videos. In part one of a two-part interview with Dr. Montori, we hear about the idea of shared decision making and how it can potentially change health care. Before hearing what he has to say, what do you think? In the context of health care, what does “shared decision making” mean to you? How is this different from traditional patientclinician communication? Why do you think some people in health care might be skeptical of shared decision making? How do you think shared decision making could improve health care? Do you think it could contribute to a “patient revolution? ” PART 1 - https: //www. youtube. com/watch? v=NECp 7 Tt. Ez. M 4 � � � � In part two, Montori walks us through how to use some innovative tools with chronic care patients and shares a touching — and humorous — story about an elderly man. PART 2 - https: //www. youtube. com/watch? v=er. Xm 9 tn-t. M 4 DISCUSSION QUESTIONS Reflect on the story of the 92 -year-old man. Why did Dr. Montori choose to tell a story about this man when asked about the benefits of the tools? Do you think the tool discussed was effective and why? How does this story relate to the subject PFCC? Do you have a story of how shared decision making made a difference in a patient’s care? The patient could be a patient of yours, a friend or family member, or yourself. Have you encountered any tools in your experience that have helped empower patients’ to take charge of their own care? Describe how the tools worked and what you It is clear that providing respect and dignity improves the patient and family experience of care. But, more importantly, providing patient- and family-centered care is also critical to creating an environment that fosters safety and quality of care. A growing body of evidence shows that improving the patient experience and developing partnerships with patients is not just a “nice-to-have”; it is linked to improved health outcomes. For example, evidence shows that patients who are more involved in their care better able to manage complex chronic conditions by understanding and incorporating their plan of care; more likely to feel comfortable communicating their concerns and seeking appropriate assistance; have reduced anxiety and stress; and have shorter lengths of stay. There is also evidence that patient- and familycentered care is cost effective.
The Values and Value of Patient-Centered Care ATTACHED ARTICLE “The Values and Value of Patient-Centered Care (Annals of Family Medicine) LINK: http: //www. annfammed. org/content/9/2/100. full Altogether, there is a growing body of evidence that patient- and family-centered care improves patient outcomes and satisfaction, and it leads to more cost-effective care. Providing patient- and family-centered care has become a large and complex field – including issues around choice, self -efficacy, shared decision-making, and individualization of care. The goals of patient- and family-centered care include involving patients and their loved ones more deeply and significantly in making the decisions that affect their care and outcomes, and in designing and improving the systems that care with and for them. But for all its complexity, patient- and family-centered care is simple: it’s about treating your patients as you would want your loved ones to be treated. Here’s what care looks like when providers truly treat patients and families with dignity and respect, and honor Patient and Family Centered Care: (Ronald M. Epstein, 2014) 1) Health care practitioners listen to and honor patient and family perspectives and choices. 2) Patient and family knowledge, values, beliefs, and cultural background are incorporated into the planning and delivery of care. 3) Patient and family needs are anticipated and physical comforts are met in a clean, safe environment. 4) The health care team provides emotional support and strives to alleviate fear and anxiety. The next slide includes research articles that have helped to prove that Patient and Family Centered Care is beneficial to the overall levels of care patients receive:

Four Leading Organizations in Patient- and Family-Centered Care The Picker Institute: http: //www. pickerinstitute. org The Institute for Patient- and Family-Centered Care: http: //www. ipfcc. org Planetree: http: //www. planetree. org The Schwartz Center: http: //www. theschwartzcenter. org
Four Leading Organizations in PFCC Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment: Results of a randomized controlled trial. Diabetes Care. 1995; 18: 943 -949. Balint M, Hunt J, Joyce D, Marinker M, Woodcock J. Treatment or Diagnosis: A Study of Repeat Prescriptions in General Practice. Philadelphia, PA: J. B. Lippincott; 1970. Balik B, Conway J, Zipperer L, Watson J. Achieving an Exceptional Patient and Family Experience of Inpatient Hospital Care. IHI Innovation Series white paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2011. Available online at http: //www. ihi. org/knowledge/Pages/IHIWhite. Papers/Achieving. Exceptional. Patient. Family. Experience. Inpatient. Hospital. Care. White. Paper. aspx Bergeson SC, Dean JD. A systems approach to patient-centered care. JAMA. 2006 Dec; 296(23): 2848 -2851. Bertakis K, Azari R. Patient-Centered Care is Associated with Decreased Health Care Utilization. J Am Board Fam Med. May-June 2011; 24: 229 -239. Berwick D. What ‘patient-centered’ should mean: Confessions of an extremist. Health Affairs. 2009; 28(4): w 555 -w 565. Available online at http: //content. healthaffairs. org/content/28/4/w 555. full Bleich SN, Ozaltin E, Murray CK. How does satisfaction with the health-care system relate to patient experience? Bull World Health Organ. 2009; 87: 271– 278. Brady C, Conway JB. Chapter 13: Integrating quality and safety with patient-centered care. In: Frampton SB, Charmel P, Planetree (editors). Putting Patients First: Best Practices in Patient. Centered Care (2 nd edition). San Francisco: Jossey-Bass Publishers; 2008: 249 -265. Charmel P, Frampton S. Building the business case for patient centered care. Healthcare Financial Management. March 2008; 62(3): 80 -85. Available online at http: //www. planetree. org/HFMbusiness%20 case%20 for%20 Planetree. pdf Children’s Hospital of Philadelphia. Family-Centered Care. Accessed March 1, 2011. Available online at http: //www. chop. edu/service/family-centered-care/about-family-centered-care/ Coleman K, Austin B, Brach C Wagner E. Evidence on the Chronic Care Model in the new millennium. Health Affairs. 2009; 28: 75 -85. Huang E. The cost effectiveness of improving diabetes care in US federally qualified community health centers. Health Services Research. 2007; 42(6): 2174 -2193. Johnson B, Abraham M, Coway J, Simmons L, Edgman-Levitan S, Sodomka P, et al. Partnering with patients and families to design a patient- and family-centered health care system. Accessed June 21, 2011. Available online at http: //www. familycenteredcare. org/pdf/Partneringwith. Patientsand. Families. pdf Institute of Healthcare Improvement (2014). Intro to Patient and Family Centered Care. Retrieved From: http: //app. ihi. org/lms/lessonpageworkflow. aspx? &Catalog. Guid=4 cc 435 f 0 -d 43 b-438184 b 8 -899 b 35082938&Course. Guid=8 eb 52137 -21 d 7 -4 b 30 -afcd-fd 781 de 6 d 6 d 5&Lesson. Guid=bd 4 bedf 3 -8 d 89 -4 a 66 -bc 9 e-dcc 7439 cb 78 e&Restart=1 Institute of Patient and Family Centered Care (2008). Partnering with Patients and Families to Design a Patient and Family-Centered Health Care System. Retrieved From: http: //www. ihi. org/resources/Pages/Publications/Partneringwith. Patientsand. Families. Recommendations. Promising. Practices. aspx Picker Institute Europe. Investment in Engagement. Accessed July 22, 2011. Available online at http: //www. investinengagement. info/ Reid RJ, Fishman PA, Yu O et al. Patient-Centered Medical Home Demonstration: A Prospective, Quasi-Experimental, Before and After Evaluation. The American Journal of Managed Care. 2009; 15(9): e 71 -e 87. Available online at http: //www. ajmc. com/articles/managed-care/AJMC_09 sep_Reid. WEb. X_e 71 toe 87 Ronald M. Epstein (2014). The Values and Value of Patient-Centered Care. Annals of Medicine. Retrieved From: http: //www. annfammed. org/content/9/2/100. full
 Qsen competencies safety examples
Qsen competencies safety examples Patient centered primary care collaborative
Patient centered primary care collaborative Patient centered care collaborative
Patient centered care collaborative Patient centered care
Patient centered care Strategies of family centered care
Strategies of family centered care Family centered care definition
Family centered care definition Paradigm shift teacher-centered to student-centered
Paradigm shift teacher-centered to student-centered Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Patient centered medical home conference
Patient centered medical home conference Patient centered medical home
Patient centered medical home Boss centered leadership
Boss centered leadership Boss centered leadership
Boss centered leadership Principle centered leadership summary
Principle centered leadership summary Boss centered leadership
Boss centered leadership