HAEMODIALYSIS Shofa chasani HIGHLIGHTS n n HD is









- Slides: 23
HAEMODIALYSIS Shofa chasani
HIGHLIGHTS n n HD is term used to describe the process whereby the solute composition of blood is altered by its contact with another solution through a semipermeable membrane HD remove solute from the blood by 2 processes: - diffusion (movement of a solute across the membrane down a concentration gradient) - convection (‘solvent drag’/ ‘ultrafiltration’), whereby solutes in the blood are pushed through a membrane by a pressure gradient (analogous to filtration)
HIGHLIGHTS n n Conventional HD relies predominantly of difussion with a small component of convective transport Sometimes blood purification is performed entirely by convection using a membrane of high permeability (HF). HF can also be combined with dialysis (HDF) but in this case most of the solute removal is by convection and not diffusion



Determinants of solute transport during haemodialysis Determinants of the rate of diffusive solute removal § § § Blood flow rate through the dialyser Surface area of the dialysis membrane Permeability of the membrane Dialysate flow rate Concentration gradient across membrane Molecular size of the solute –not only do large molecules move more slowly than small molecules but they may be too large to pass through the membrane pores

Determinants of solute transport during hemodialysis Determinants of the rate of convective solute transport n n n Surface area and water permeability of the membrane Membrane porosity Blood flow rate through the dialyser Size of the solute Pressure differential across the membrane
Determinants of solute transport during hemodialysis Effect of membrane porosity on solute removal The porosity of the dialysis membrane refers to the size of the molecules that can pass through the pores of the membrane. A highly porous membrane allows movement of large molecules, which would be excluded by a low porosity membrane (pore size <500 daltons). Generally, membranes with a high kuf are also highly porous.
Determinants of solute transport during hemodialysis Effect of transmembrane pressure on solute removal The transmembrane pressure is continually monitored during HD or HF and can be varied in a number of ways to influence the rate of convective transport.

Determinants of solute transport during hemodialysis Solute removal by membrane adsorption Large-MW molecules, such as β 2 -microglobulin, may also be removed by adsorption, a process whereby the molecule attaches to the dialysis membrane. The adsorptive capacity of a dialysis membrane is largely determined by its composition.
Methods of blood purification using diffusive & convective therapies Conventional Haemodialysis n n In conventional HD, the blood & dialysate fluid compartments are separated by a semipermeable membrane. This membranes can be made from various materials The patient’s blood flows in the opposite direction to the dialysate (countercurrent flow), which maximizes diffusive solute transfer
Methods of blood purification using diffusive & convective therapies High-flux & high-efficiency haemodialysis n n Compared to conventional HD, high-flux membranes rely, to a larger degree, on convective solute transport, which make them more effective at removing higher molecular weight solutes, such as β 2 -microglobulin Although observational studies have demonstrated improvement in BP control & neuropathic symptoms using high-flux therapies, there are no randomized controlled on long-term outcomes, such as mortality, cardiovascular events or bone disease
Methods of blood purification using diffusive & convective therapies High-flux & high-efficiency Haemodialysis n Most high-flux membranes in use can also be classified as ‘high efficiency’ because of their large surface area, making them also more efficient at removing low-MW solutes Although there was initially some interest in using these membranes to shorten dialysis treatment times, this approach is not recommended
Methods of blood purification using diffusive & convective therapies Haemofiltration & haemodiafiltration n n As mentioned above, HF relies solely on convective solute transport to remove uraemic toxins from the blood. HF is most commonly used in patients receiving continuous treatment in the intensive care setting. Replacement fluid is infuse directly into the patient’s blood, usually using a prepared sterile solution HDF combines HF with HD to introduce a component of diffusive transport. In the chronic setting, this therapy is most effective at removing high-MW solutes but is considerably more expensive & requires ultra-pure dialysis water.

Methods of blood purification using diffusive & convective therapies Haemofiltration & haemodiafiltration n Because of its expense, HDF is generally reserved for patients receiving continous tratment in the intensivecare setting or chronic dialysis patients who have complications possibly related to the accumulation of high. MW uraemic toxins, including β 2 -microglobulin associated amyloidosis and uraemic neuropathy



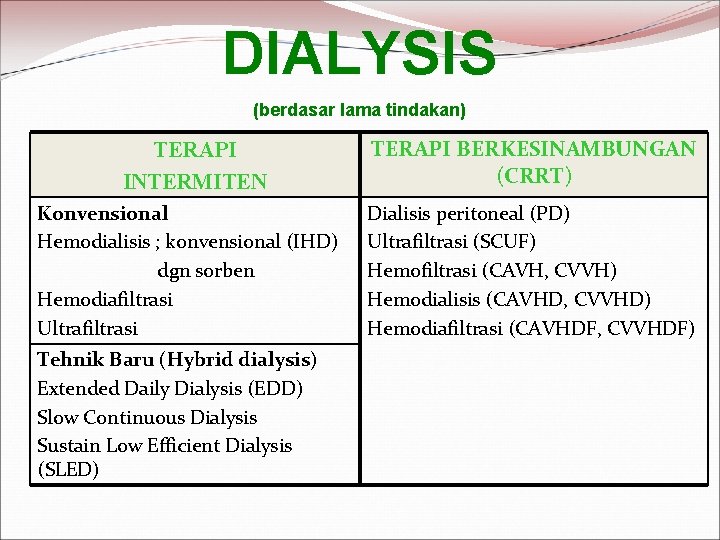
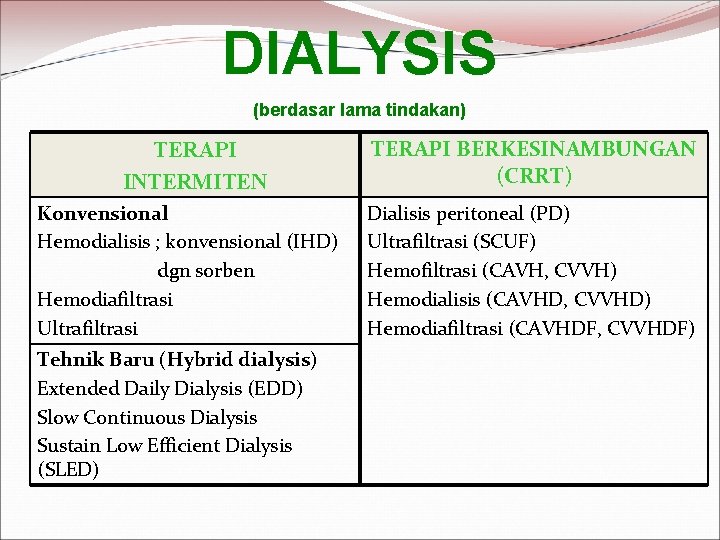
DIALYSIS (berdasar lama tindakan) TERAPI INTERMITEN Konvensional Hemodialisis ; konvensional (IHD) dgn sorben Hemodiafiltrasi Ultrafiltrasi Tehnik Baru (Hybrid dialysis) Extended Daily Dialysis (EDD) Slow Continuous Dialysis Sustain Low Efficient Dialysis (SLED) TERAPI BERKESINAMBUNGAN (CRRT) Dialisis peritoneal (PD) Ultrafiltrasi (SCUF) Hemofiltrasi (CAVH, CVVH) Hemodialisis (CAVHD, CVVHD) Hemodiafiltrasi (CAVHDF, CVVHDF)