Endoscopy Recovery Upper GI Suspected Cancer Recognition Referral
- Slides: 12
Endoscopy Recovery
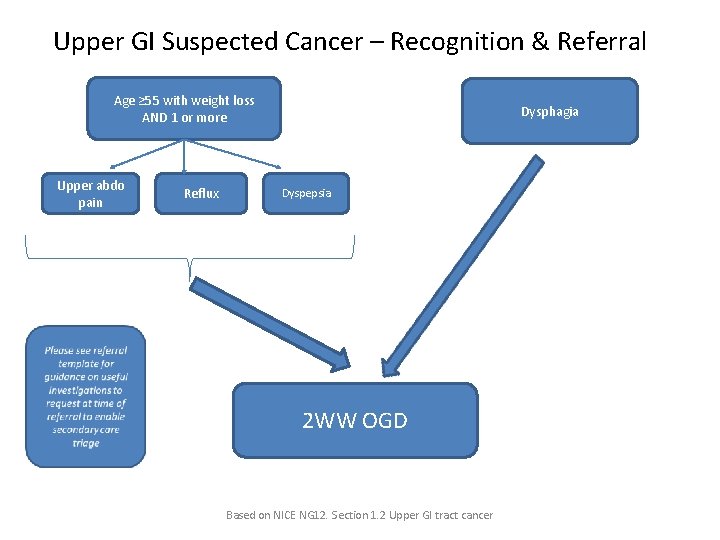
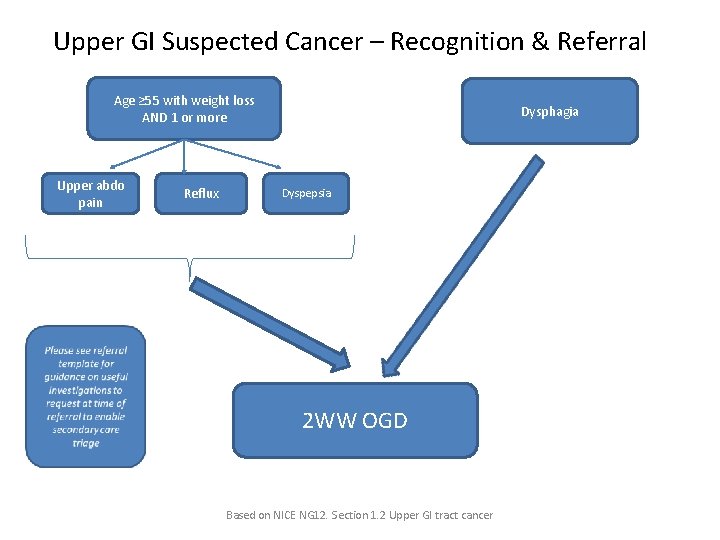
Upper GI Suspected Cancer – Recognition & Referral Age ≥ 55 with weight loss AND 1 or more Upper abdo pain Reflux Dysphagia Dyspepsia 2 WW OGD Based on NICE NG 12. Section 1. 2 Upper GI tract cancer
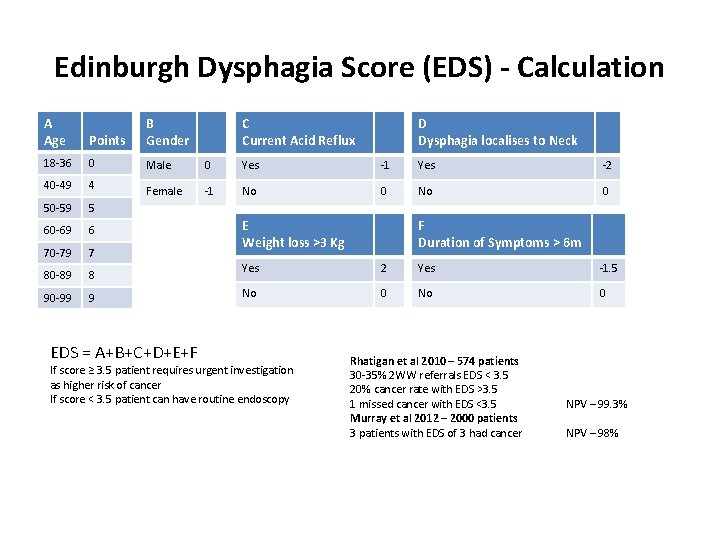
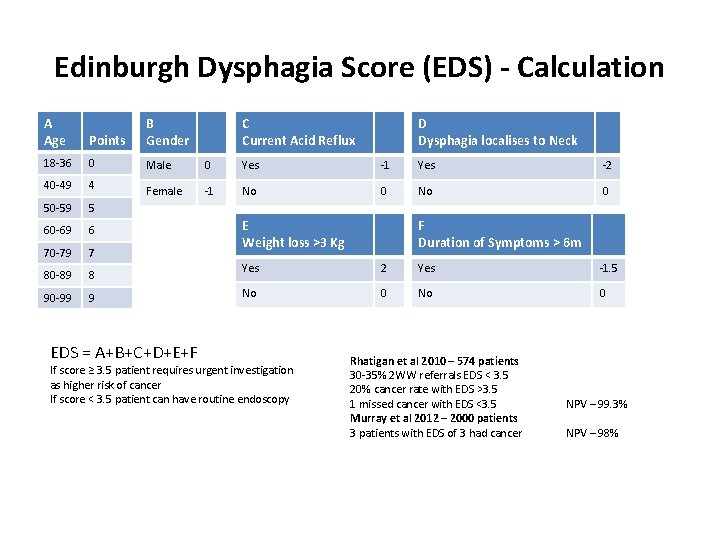
Edinburgh Dysphagia Score (EDS) - Calculation A Age Points B Gender 18 -36 0 Male 0 Yes -1 Yes -2 40 -49 4 Female -1 No 0 50 -59 5 60 -69 6 70 -79 7 80 -89 8 90 -99 9 EDS = A+B+C+D+E+F C Current Acid Reflux D Dysphagia localises to Neck E Weight loss >3 Kg F Duration of Symptoms > 6 m Yes 2 Yes -1. 5 No 0 If score ≥ 3. 5 patient requires urgent investigation as higher risk of cancer If score < 3. 5 patient can have routine endoscopy Rhatigan et al 2010 – 574 patients 30 -35% 2 WW referrals EDS < 3. 5 20% cancer rate with EDS >3. 5 1 missed cancer with EDS <3. 5 Murray et al 2012 – 2000 patients 3 patients with EDS of 3 had cancer NPV – 99. 3% NPV – 98%
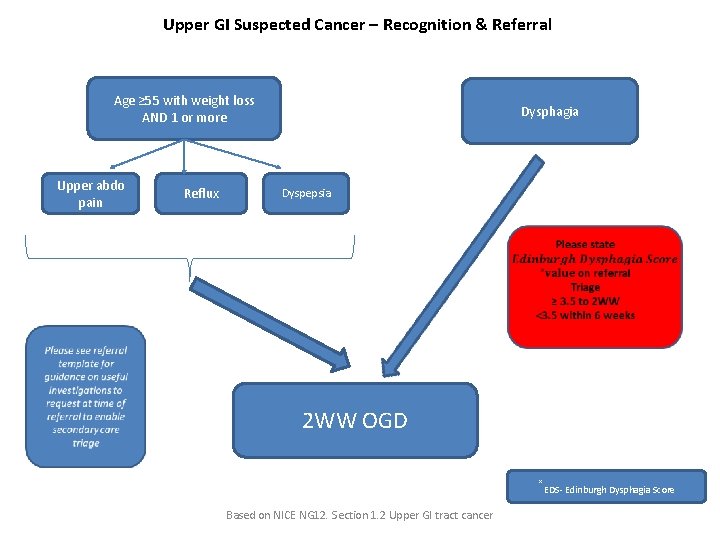
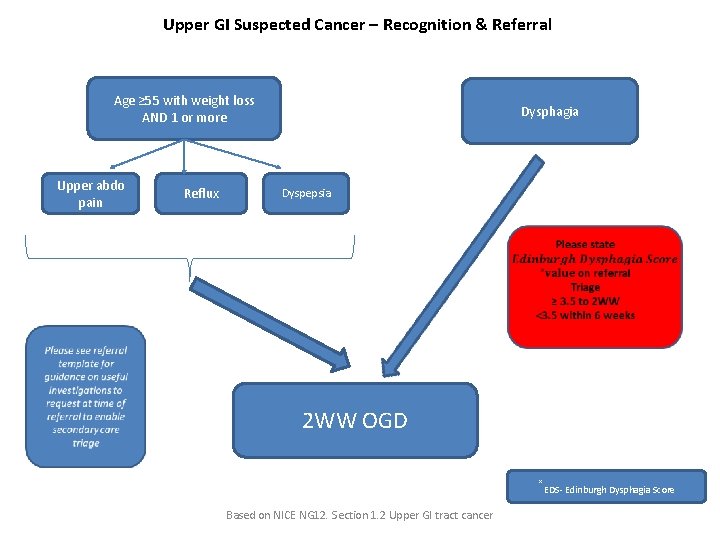
Upper GI Suspected Cancer – Recognition & Referral Age ≥ 55 with weight loss AND 1 or more Upper abdo pain Reflux Dysphagia Dyspepsia 2 WW OGD ˟EDS- Edinburgh Dysphagia Score Based on NICE NG 12. Section 1. 2 Upper GI tract cancer
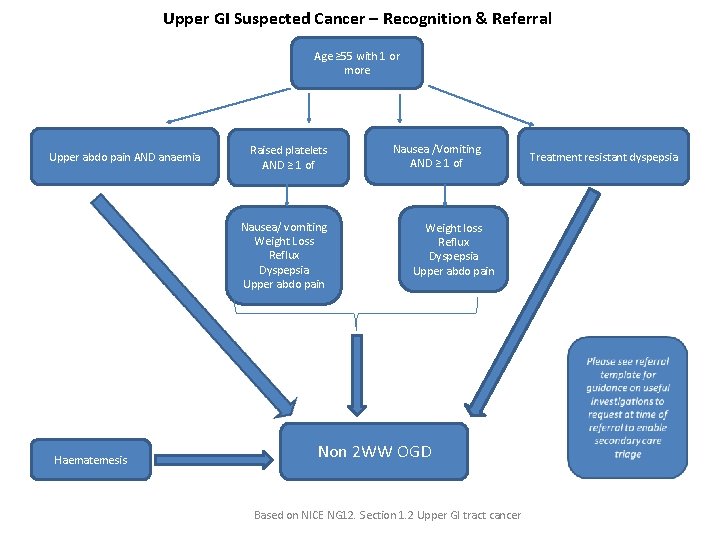
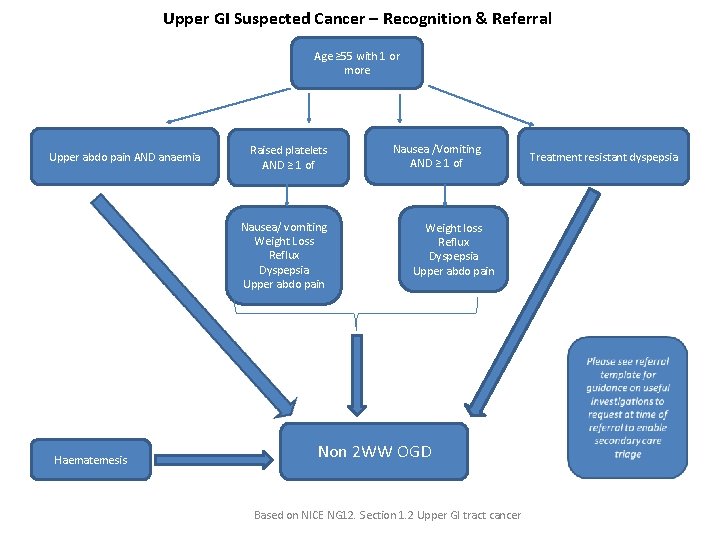
Upper GI Suspected Cancer – Recognition & Referral Age ≥ 55 with 1 or more Upper abdo pain AND anaemia Raised platelets AND ≥ 1 of Nausea/ vomiting Weight Loss Reflux Dyspepsia Upper abdo pain Haematemesis Nausea /Vomiting AND ≥ 1 of Weight loss Reflux Dyspepsia Upper abdo pain Non 2 WW OGD Based on NICE NG 12. Section 1. 2 Upper GI tract cancer Treatment resistant dyspepsia
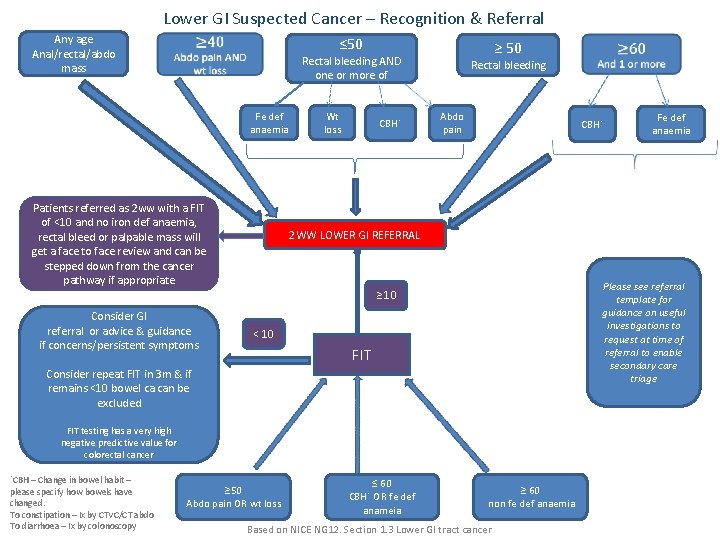
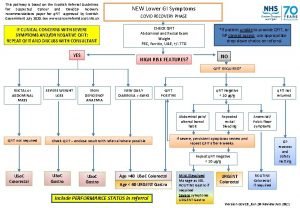
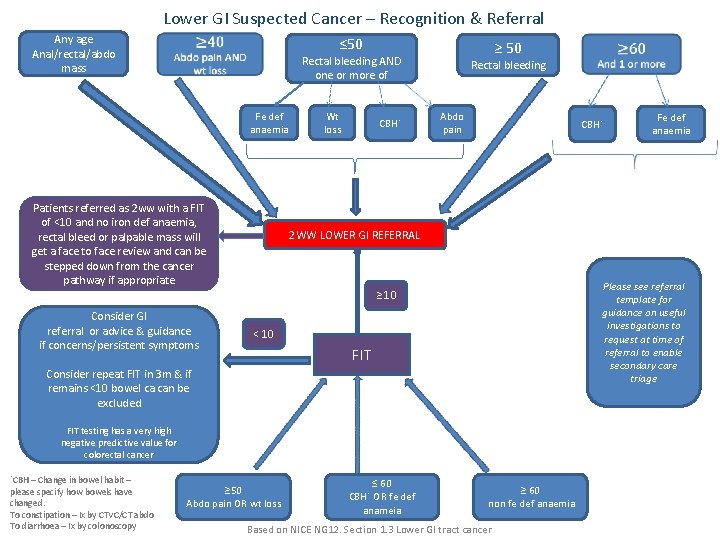
Lower GI Suspected Cancer – Recognition & Referral Any age Anal/rectal/abdo mass ≤ 50 ≥ 50 Rectal bleeding AND one or more of Fe def anaemia Patients referred as 2 ww with a FIT of <10 and no iron def anaemia, rectal bleed or palpable mass will get a face to face review and can be stepped down from the cancer pathway if appropriate Wt loss CBH˟ Rectal bleeding Abdo pain CBH˟ Please see referral template for guidance on useful investigations to request at time of referral to enable secondary care triage ˂ 10 FIT Consider repeat FIT in 3 m & if remains <10 bowel ca can be excluded FIT testing has a very high negative predictive value for colorectal cancer ˟CBH – Change in bowel habit – please specify how bowels have changed. To constipation – Ix by CTVC/CT abdo To diarrhoea – Ix by colonoscopy Fe def anaemia 2 WW LOWER GI REFERRAL ≥ 10 Consider GI referral or advice & guidance if concerns/persistent symptoms ≥ 50 Abdo pain OR wt loss ≤ 60 CBH˟ OR fe def anameia ≥ 60 non fe def anaemia Based on NICE NG 12. Section 1. 3 Lower GI tract cancer
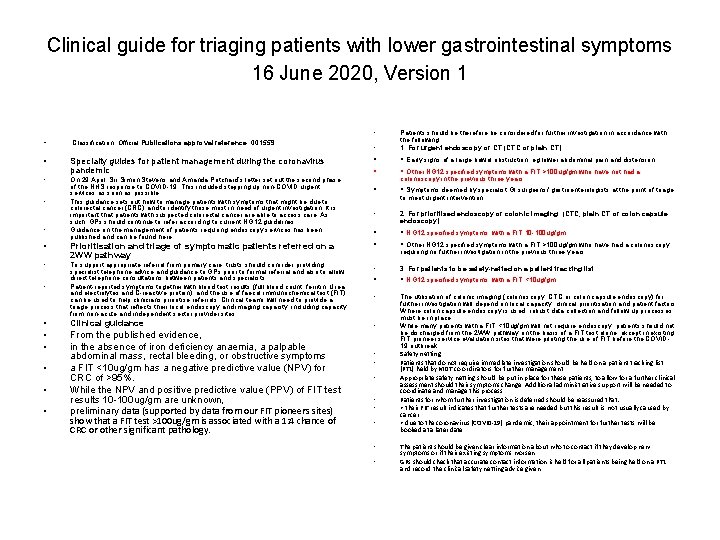
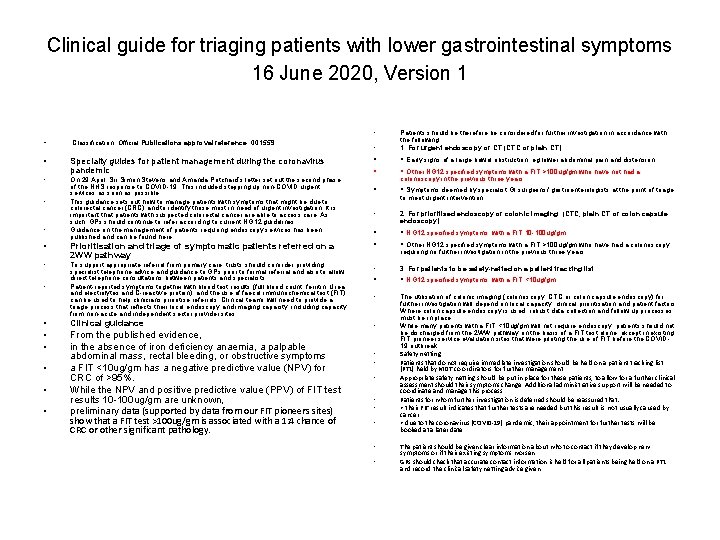
Clinical guide for triaging patients with lower gastrointestinal symptoms 16 June 2020, Version 1 • • Classification: Official Publications approval reference: 001559 • Specialty guides for patient management during the coronavirus pandemic • On 29 April, Sir Simon Stevens and Amanda Pritchard’s letter set out the second phase of the NHS response to COVID-19. This included stepping up non-COVID urgent services as soon as possible. This guidance sets out how to manage patients with symptoms that might be due to colorectal cancer (CRC) and to identify those most in need of urgent investigation. It is important that patients with suspected colorectal cancer are able to access care. As such, GPs should continue to refer according to current NG 12 guidelines. Guidance on the management of patients requiring endoscopy services has been published and can be found here. • • • Patients should be therefore be considered for further investigation in accordance with the following: 1. For urgent endoscopy or CT (CTC or plain CT) • • • Early signs of a large bowel obstruction, eg lower abdominal pain and distension. • Other NG 12 specified symptoms with a FIT >100 ug/gm who have not had a • • Symptoms deemed by specialist GI surgeons/ gastroenterologists at the point of triage, • 2. For prioritised endoscopy or colonic imaging: (CTC, plain CT or colon capsule endoscopy) • • • NG 12 specified symptoms, with a FIT 10 -100 ug/gm. • Other NG 12 specified symptoms with a FIT >100 ug/gm who have had a colonoscopy in the previous three years. to merit urgent intervention. • Prioritisation and triage of symptomatic patients referred on a 2 WW pathway • To support appropriate referral from primary care, trusts should consider providing specialist telephone advice and guidance to GPs prior to formal referral and also to allow direct telephone consultations between patients and specialists. Patient-reported symptoms together with blood test results (full blood count, ferritin, Urea and electrolytes and C-reactive protein), and the use of faecal immunochemical test (FIT) can be used to help clinicians prioritise referrals. Clinical teams will need to provide a triage process that reflects their local endoscopy and imaging capacity, including capacity from non-acute and independent sector provider sites. • 3. For patients to be safety-netted on a patient tracking list • • NG 12 specified symptoms, with a FIT <10 ug/gm. • • Clinical guidance • • From the published evidence, in the absence of iron deficiency anaemia, a palpable abdominal mass, rectal bleeding, or obstructive symptoms a FIT <10 ug/gm has a negative predictive value (NPV) for CRC of >95%. While the NPV and positive predictive value (PPV) of FIT test results 10 -100 ug/gm are unknown, preliminary data (supported by data from our FIT pioneers sites) show that a FIT test >100 ug/gm is associated with a 1: 4 chance of CRC or other significant pathology. • The utilisation of colonic imaging (colonoscopy, CTC or colon capsule endoscopy) for further investigation will depend on local capacity, clinical prioritisation and patient factors. Where colon capsule endoscopy is used, robust data collection and follow up processes must be in place. While many patients with a FIT <10 ug/gm will not require endoscopy, patients should not be discharged from the 2 WW pathway on the basis of a FIT test alone, except in existing FIT pioneer service evaluation sites that were piloting the use of FIT before the COVID 19 outbreak. Safety netting Patients that do not require immediate investigation should be held on a patient tracking list (PTL) held by MDT co-ordinators for further management. Appropriate safety netting should be put in place for these patients, to allow for a further clinical assessment should their symptoms change. Additional administrative support will be needed to coordinate and manage this process. Patients for whom further investigation is deferred should be reassured that: • their FIT result indicates that further tests are needed but this result is not usually caused by cancer • due to the coronavirus (COVID-19) pandemic, their appointment for further tests will be booked at a later date. • • • requiring no further investigation in the previous three years. The patient should be given clear information about who to contact if they develop new symptoms or if their existing symptoms worsen. GPs should check that accurate contact information is held for all patients being held on a PTL and record the clinical safety netting advice given.
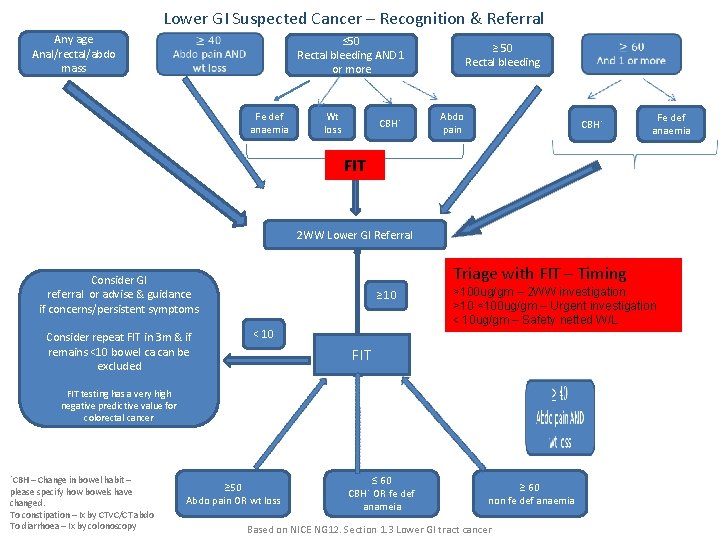
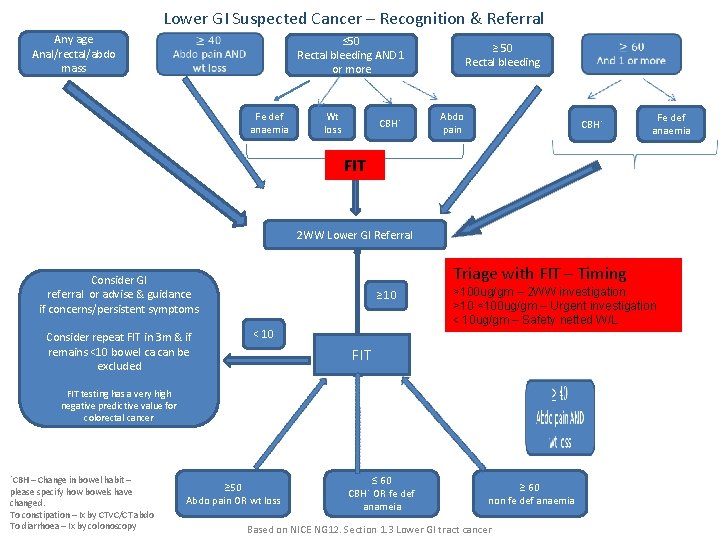
Lower GI Suspected Cancer – Recognition & Referral Any age Anal/rectal/abdo mass ≤ 50 Rectal bleeding AND 1 or more Fe def anaemia Wt loss CBH˟ ≥ 50 Rectal bleeding Abdo pain CBH˟ Fe def anaemia FIT 2 WW Lower GI Referral Triage with FIT – Timing Consider GI referral or advise & guidance if concerns/persistent symptoms Consider repeat FIT in 3 m & if remains <10 bowel ca can be excluded ≥ 10 ˂ 10 >100 ug/gm – 2 WW investigation >10 <100 ug/gm – Urgent investigation < 10 ug/gm – Safety netted W/L FIT testing has a very high negative predictive value for colorectal cancer ˟CBH – Change in bowel habit – please specify how bowels have changed. To constipation – Ix by CTVC/CT abdo To diarrhoea – Ix by colonoscopy ≥ 50 Abdo pain OR wt loss ≤ 60 CBH˟ OR fe def anameia ≥ 60 non fe def anaemia Based on NICE NG 12. Section 1. 3 Lower GI tract cancer
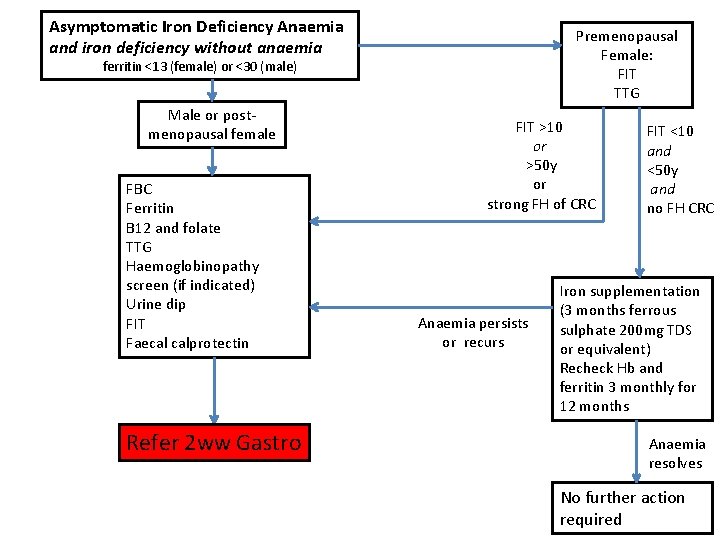
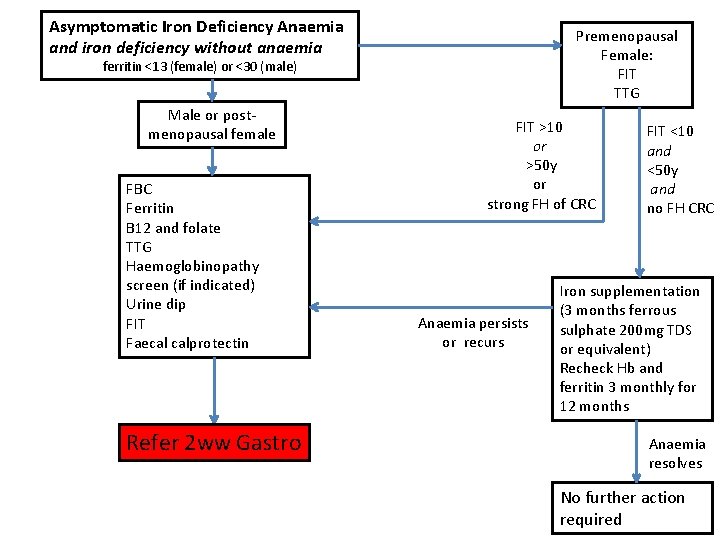
Asymptomatic Iron Deficiency Anaemia and iron deficiency without anaemia Premenopausal Female: FIT TTG ferritin <13 (female) or <30 (male) Male or postmenopausal female FBC Ferritin B 12 and folate TTG Haemoglobinopathy screen (if indicated) Urine dip FIT Faecal calprotectin Refer 2 ww Gastro FIT >10 or >50 y or strong FH of CRC Anaemia persists or recurs FIT <10 and <50 y and no FH CRC Iron supplementation (3 months ferrous sulphate 200 mg TDS or equivalent) Recheck Hb and ferritin 3 monthly for 12 months Anaemia resolves No further action required
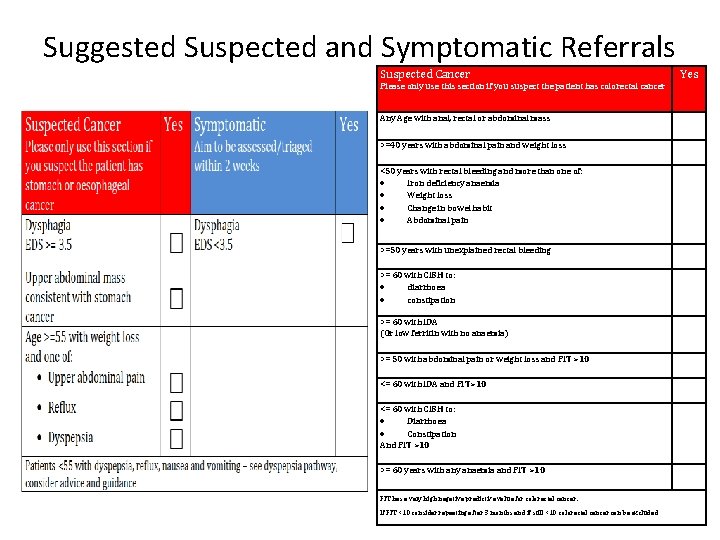
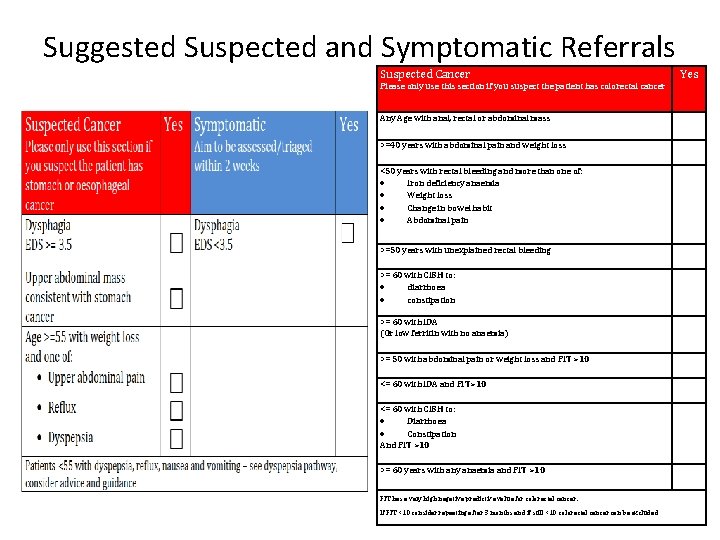
Suggested Suspected and Symptomatic Referrals Suspected Cancer Yes Please only use this section if you suspect the patient has colorectal cancer Any Age with anal, rectal or abdominal mass >=40 years with abdominal pain and weight loss <50 years with rectal bleeding and more than one of: Iron deficiency anaemia Weight loss Change in bowel habit Abdominal pain >=50 years with unexplained rectal bleeding >= 60 with CIBH to: diarrhoea constipation >= 60 with IDA (Or low ferritin with no anaemia) >= 50 with abdominal pain or weight loss and FIT >10 <= 60 with IDA and FIT>10 <= 60 with CIBH to: Diarrhoea Constipation And FIT >10 >= 60 years with any anaemia and FIT >10 FIT has a very high negative predictive value for colorectal cancer. If FIT <10 consider repeating after 3 months and if still <10 colorectal cancer can be excluded
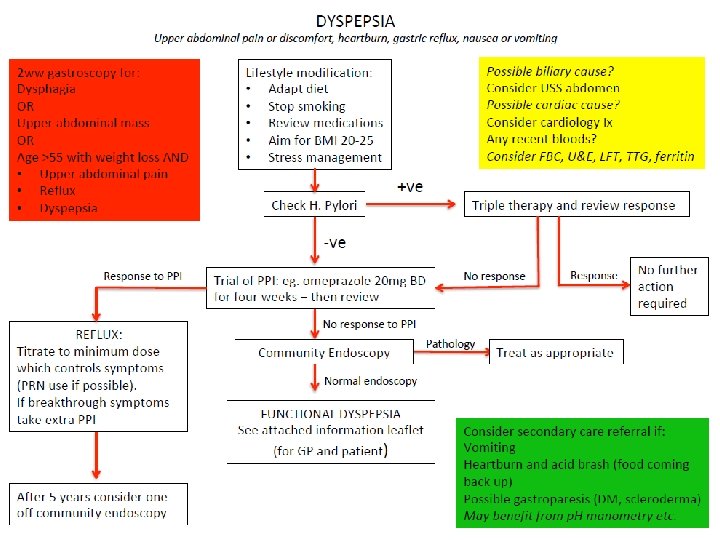
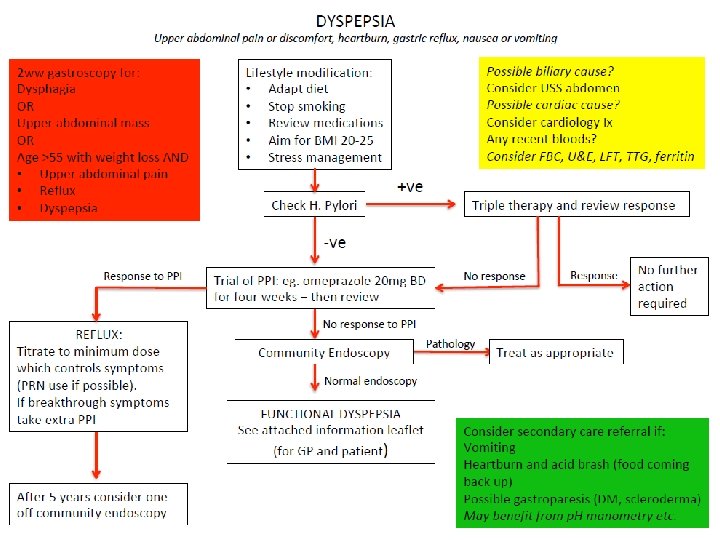
Dyspepsia Guidelines 2020 – Supporting notes Endoscopy Where community endoscopy is not available refer to secondary care This indication will currently be triaged as a Category 3 and patients will be placed on the routine endoscopy waiting list H. Pylori Treat according to local guidelines Advice and Guidance Consider discussion with local gastroenterology where there any concerns or where patient symptoms not responding
 Suspected cancer recognition and referral
Suspected cancer recognition and referral Suspected cancer recognition and referral
Suspected cancer recognition and referral Nrl head injury recognition and referral form
Nrl head injury recognition and referral form Scottish cancer referral guidelines
Scottish cancer referral guidelines Endoscopy terminology
Endoscopy terminology Purpose of endoscopy
Purpose of endoscopy Endoscopy
Endoscopy Colostomy irrigation procedure
Colostomy irrigation procedure Endoscopy total internal reflection
Endoscopy total internal reflection National endoscopy database
National endoscopy database Upper gi small bowel follow through
Upper gi small bowel follow through Hup endoscopy
Hup endoscopy Endoscopy in pregnancy guidelines
Endoscopy in pregnancy guidelines